Amiodarone pulmonary toxicity
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]; Associate Editor(s)-in-Chief: Hardik Patel, M.D.
Overview
Amiodarone is an antiarrhythmic drug which is commonly used to treat ventricular and supraventricular arrhythmias, in particular following pulmonary and cardiac surgery, due to a higher incidence of postoperative atrial fibrillation in these patients. It is an iodine-containing compound that tends to accumulate in several organs, including the lungs. It has been associated with a variety of adverse effects. Most individuals administered amiodarone on a chronic basis will experience at least one side effect. The most serious adverse effect is amiodarone-induced pulmonary toxicity. It occurs mostly in patients receiving large doses of the drug over prolonged periods.
Amiodarone Pulmonary Toxicity
Pulmonary toxicity is the most serious adverse effect of amiodarone, which may occur in up to 5–10% of treated patients.[1]
Types
Acute Pulmonary Toxicity
- Acute respiratory distress syndrome:
The rare but the most dangerous form of pulmonary toxicity is a sudden, life-threatening, diffuse lung involvement called acute respiratory distress syndrome (ARDS). Patients with ARDS rapidly develop severe dyspnea and hypoxia. They usually must be placed on mechanical ventilators, and their mortality rate even with intensive therapy approaches 50%. ARDS related to amiodarone is seen most often following major surgical procedures, especially cardiac surgery, but it can be seen at any time and without any obvious precipitating causes.
Intermediate Pulmonary Toxicity
- Diffuse alveolar hemorrhage
- Pneumonia
Chronic Pulmonary Toxicity
- Chronic interstitial pneumonitis:
The most common presentation of amiodarone-induced pulmonary toxicity is the chronic interstitial pneumonitis. It has an insidious and gradual onset. It is characterized by the slowly progressing dyspnea, cough, weight loss, and easy fatigue. These symptoms are easy to mistaken for heart disease or the effects of aging, as many patients taking amiodarone have a history of heart disease.
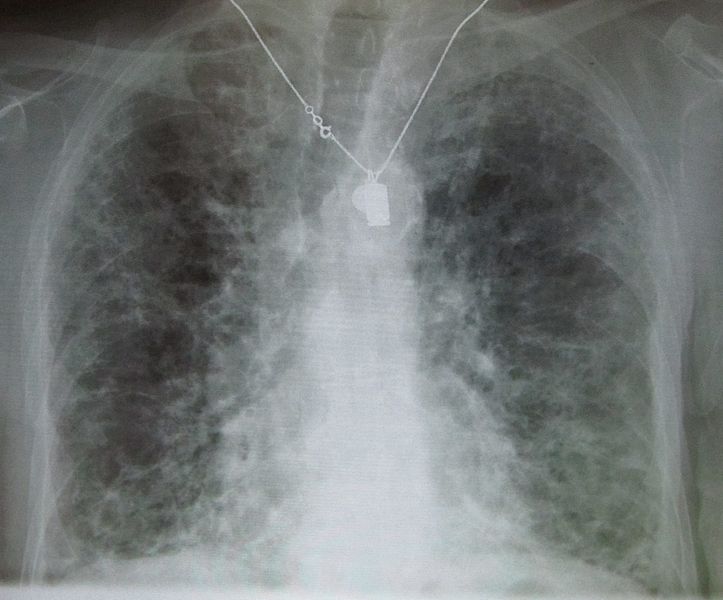
Copyleft image obtained courtesy of http://en.wikipedia.org/wiki/File:IPF_amiodarone.JPG; James Heilman, MD.
- Solitary lung mass
Risk Factors
Anyone taking amiodarone is at risk. Patients on higher doses and one who have been taking the drug for a long period of time appear to have a higher risk, and some evidence suggests that individuals with underlying lung disease are also more likely to develop toxicity with amiodarone.
- High cumulative dose (more than 400 milligrams per day)
- Duration over two months
- Increased age
- Preexisting pulmonary disease
Some individuals were noted to develop pulmonary fibrosis after a week of treatment, while others did not develop it after years of continuous use. Common practice is to avoid the drug if possible in individuals with decreased lung function.
Clinical Presentation
The clinical manifestations of amiodarone-induced pulmonary toxicity are vague and include dyspnea, nonproductive cough, and any new pulmonary symptom in patient taking amiodarone
References
- ↑ Martin WJ, Rosenow EC (1988). "Amiodarone pulmonary toxicity. Recognition and pathogenesis (Part I)". Chest. 93 (5): 1067–75. PMID 3282816.