Amblyopia (patient information)
For the WikiDoc page for this topic, click here
| Amblyopia | |
 | |
|---|---|
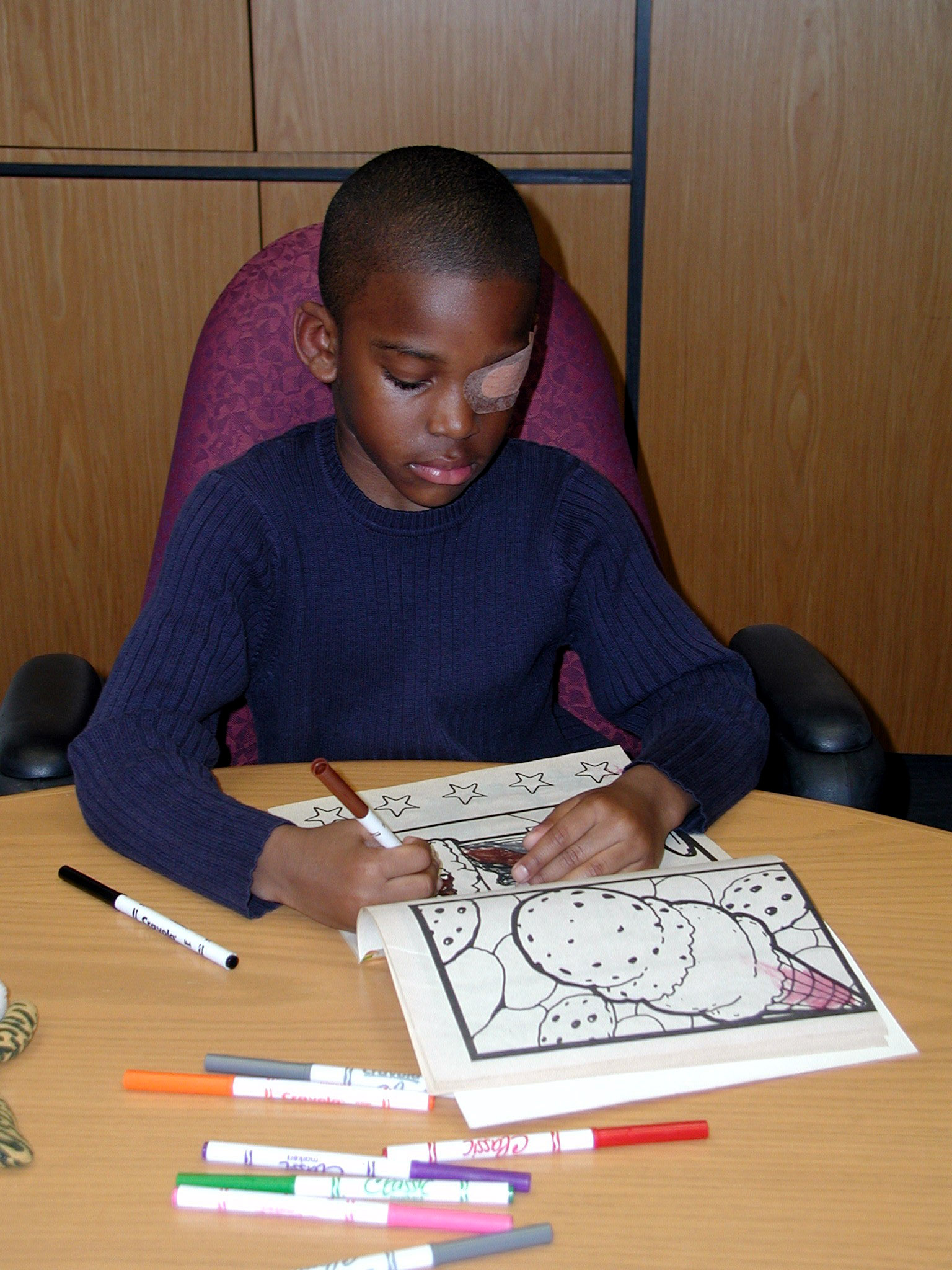
| A child wearing an adhesive eyepatch to correct amblyopia | |
| ICD-10 | H53.0 |
| ICD-9 | 368.0 |
| DiseasesDB | 503 |
| MedlinePlus | 001014 |
| MeSH | D000550 |
Editor-in-Chief: Erin E. Lord
Assistant Editor-In-Chief: Amanda Chirlin
Overview
Amblyopia (commonly referred to as "lazy eye") is the failure of one eye to develop normal vision and see details properly, although the eye itself is otherwise physically normal. It is the most common cause of vision problems in children.
What are the symptoms of amblyopia?
Amblyopia can often go undetected to the untrained observer. In fact, many people with amblyopia, especially those who are only mildly so, are not even aware they have the condition until tested at older ages since the vision in their stronger eye is normal. However, people with more severe amblyopia may experience associated visual disorders, most notably poor depth perception. Other symptoms include:
- Eyes that turn in or out
- Eyes that do not appear to work together
- Poor spatial acuity
- Low sensitivity to contrast
- Problems of binocular vision:
- Limited depth perception
- Difficulty seeing the three-dimensional images in hidden stereoscopic displays such as autostereograms.[1]
- Some "higher-level" vision problems, such as reduced sensitivity to motion [2]
What are the causes of amblyopia?
The brain and the eye work together to produce vision. Light enters the eye and is changed into nerve signals that travel along the optic nerve to the brain. Amblyopia is the medical term used when the vision in one of the eyes is reduced because the eye and the brain are not working together properly. The eye itself looks normal, but it is not being used normally because the brain is favoring the other eye. As a result, the affected eye fails to develop normal vision, and therefore has trouble seeing details. It has been estimated to affect 1–5% of the population.[3]
Amblyopia is caused primarily by one of two factors: improper alignment of the eyes (known as strabismus), or unequal refractive power. If the child's eyes are not properly aligned, the brain will receive two different images from the eyes. Perceiving double vision, the brain will not use the image from the weaker eye. This eye, through lack of use, gradually loses its ability to function.
The second primary cause of amblyopia is significantly unequal refractive power in the two eyes. For example, one eye may be very farsighted or nearsighted while the other eye may have normal vision. Again the brain receives different images from the two eyes and suppresses the image from the weaker eye.
Other causes of amblyopia include:
- Family history of amblyopia
- Astigmatism in both eyes
- Childhood cataracts
Ambylopia can also occur physiologically after tobacco or alcohol consumption.
Who is at highest risk for amblyopia?
Those with a family history of amblyopia have an increased risk of the disorder. Additionally, young children with an astigmatism in both eyes, childhood cataracts, strabismus, and unequal refractive power are at increased risk of amblyopia. Ambylopia can also occur physiologically after tobacco or alcohol consumption.
How to know you have amblyopia?
Amblyopia often goes undetected to the untrained observer, but is usually easily diagnosed with a complete examination of the eyes. Special tests are not typically required.
When to seek urgent medical care?
Although not considered a medical emergency, amblyopia should be treated as early as possible. An ophthalmologist or optometrist should be seen if a vision problem is suspected in a young child so that proper treatment may begin before permanent vision loss occurs.
Treatment options
There are several methods currently used to treat amblyopia:
- Patching: Patching is the main method used to treat amblyopia. An opaque, adhesive patch is worn over the stronger eye for weeks to months. This therapy forces the child to use the eye with amblyopia. Patching stimulates vision in the weaker eye and helps the part of the brain that manages vision to develop more completely.
- Atropine: A drop of a drug called atropine is placed in the stronger eye once a day to temporarily blur the vision so that the child will prefer to use the eye with amblyopia. Similar to patching, treatment with atropine stimulates vision in the weaker eye and helps the part of the brain that manages vision to develop more completely.
- Surgery is sometimes necessary if severe strabismus is present. The surgery is usually an outpatient procedure, and will properly align the eye muscle attachments.
- Glasses: If the lazy eye is due to a vision problem (nearsightedness or farsightedness), glasses or contact lenses will be prescribed. However, glasses alone will not correct amblyopia.
- Orthoptics are a controversial practice of using eye exercises to teach new vision habits. As with glasses, eye exercises alone will not correct amblyopia.
Previously, eye care professionals often thought that treating amblyopia in older children would be of little benefit. However, surprising results from a nationwide clinical trial, An Evaluation Of Treatment Of Amblyopia In Children 7 To < 18 Years Old (ATS3), show that many children age 7 through 17 with amblyopia may benefit from treatments that are more commonly used on younger children.[4] This study shows that age alone should not be used as a factor to decide whether or not to treat a child for amblyopia.
For treatment of crossed eyes, see: Strabismus
Where to find medical care for amblyopia?
Directions to Hospitals Treating amblyopia
Prevention of amblyopia
Amblyopia cannot be prevented from initially occurring, but early recognition and treatment of the problem in children can help to prevent permanent vision loss. All children should have a complete eye examination at least once between ages 3 and 5.
What to expect (Outlook/Prognosis)?
Vision screening by age 4 can successfully detect reduced vision in one or both eyes resulting from amblyopia. Children who receive treatment before age 5 usually have a near complete recovery of normal vision.
Children will not outgrow either amblyopia or strabismus, so early examinations are essential. Delaying treatment can result in permanent vision problems. After age 10, only a partial recovery of vision can be expected. A child whose amblyopia or strabismus is left untreated will grow into an adult who has poor or little vision.
Additional links
http://www.nei.nih.gov/health/amblyopia/amblyopia_guide.asp
http://www.nlm.nih.gov/medlineplus/ency/article/001014.htm
http://www.sightandhearing.org/sightcenter/ambly.asp
Sources
- ↑ Tyler, C.W. (2004). "Binocular Vision In, Duane's Foundations of Clinical Ophthalmology. Vol. 2, Tasman W., Jaeger E.A. (Eds.), J.B. Lippincott Co.: Philadelphia".
- ↑ Hess, R.F., Mansouri, B., Dakin, S.C., & Allen, H.A. (2006). "Integration of local motion is normal in amblyopia". J Opt Soc Am a Opt Image Sci Vis. 23 (5): 986–992. doi:10.1364/JOSAA.23.000986. PMID 16642175.
- ↑ Weber, JL; Wood, Joanne (2005). "Amblyopia: Prevalence, Natural History, Functional Effects and Treatment" ([dead link] – Scholar search). Clinical and Experimental Optometry. 88 (6): 365–375. doi:10.1111/j.1444-0938.2005.tb05102.x. PMID 16329744.
- ↑ http://www.nei.nih.gov/news/pressreleases/041105.asp
- CS1 maint: Multiple names: authors list
- All articles with dead external links
- Articles with dead external links from June 2008
- Articles with invalid date parameter in template
- Patient information
- Opthalmology
- Opthalmology patient information
- Optometry
- Pediatrics
- Pediatrics patient information
- Disease state
- Mature chapter