Neurofibromatosis
| Neurofibromatosis | |
 | |
|---|---|
| Back of an elderly woman with Neurofibromatosis. | |
| ICD-10 | Q85.0 |
| ICD-9 | 237.7 |
| ICD-O: | 9540/0 |
| eMedicine | derm/287 |
| MeSH | D017253 |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]
|
WikiDoc Resources for Neurofibromatosis |
|
Articles |
|---|
|
Most recent articles on Neurofibromatosis Most cited articles on Neurofibromatosis |
|
Media |
|
Powerpoint slides on Neurofibromatosis |
|
Evidence Based Medicine |
|
Cochrane Collaboration on Neurofibromatosis |
|
Clinical Trials |
|
Ongoing Trials on Neurofibromatosis at Clinical Trials.gov Trial results on Neurofibromatosis Clinical Trials on Neurofibromatosis at Google
|
|
Guidelines / Policies / Govt |
|
US National Guidelines Clearinghouse on Neurofibromatosis NICE Guidance on Neurofibromatosis
|
|
Books |
|
News |
|
Commentary |
|
Definitions |
|
Patient Resources / Community |
|
Patient resources on Neurofibromatosis Discussion groups on Neurofibromatosis Patient Handouts on Neurofibromatosis Directions to Hospitals Treating Neurofibromatosis Risk calculators and risk factors for Neurofibromatosis
|
|
Healthcare Provider Resources |
|
Causes & Risk Factors for Neurofibromatosis |
|
Continuing Medical Education (CME) |
|
International |
|
|
|
Business |
|
Experimental / Informatics |
Please Take Over This Page and Apply to be Editor-In-Chief for this topic: There can be one or more than one Editor-In-Chief. You may also apply to be an Associate Editor-In-Chief of one of the subtopics below. Please mail us [2] to indicate your interest in serving either as an Editor-In-Chief of the entire topic or as an Associate Editor-In-Chief for a subtopic. Please be sure to attach your CV and or biographical sketch.
Overview
Neurofibromatosis is a genetically-inherited disease in which nerve tissue grows tumors (e.g. neurofibromas) that may be harmless or may cause serious damage by compressing nerves and other tissues. The disorder affects all neural crest cells (Schwann cells, melanocytes, endoneurial fibroblasts). Cellular elements from these cell types proliferate excessively throughout the body forming tumors and the melanocytes function abnormally resulting in disordered skin pigmentation.The tumors may cause bumps under the skin, colored spots, skeletal problems, pressure on spinal nerve roots, and other neurological problems. [1]
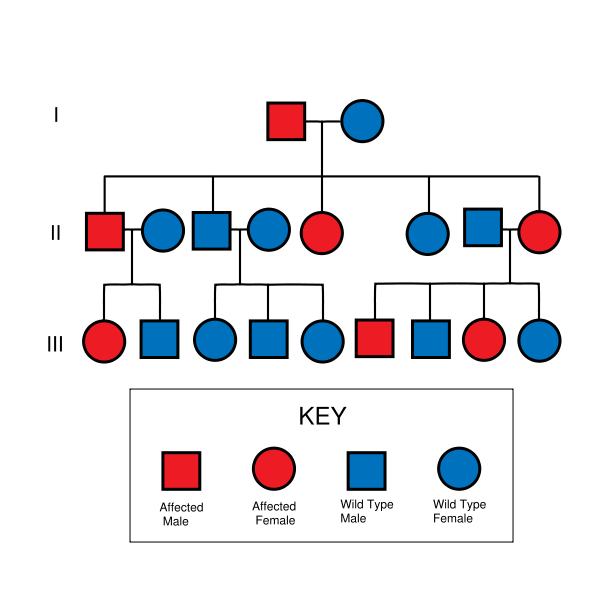
Neurofibromatosis is autosomal dominant, which means that it affects males and females equally and is dominant (only one copy of the affected gene is needed to get the disorder). Therefore, if only one parent has neurofibromatosis, his or her children have a 50% chance of developing the condition as well. Disease severity in affected individuals, however, can vary (this is called variable expressivity). Moreover, in around half of cases there is no other affected family member because a new mutation has occurred.
Types
- Neurofibromatosis type I Incidence is 1:3,500 live births
- Neurofibromatosis type II (or "MISME Syndrome"). Incidence is 1:25,000
- Schwannomatosis. Incidence is unknown but thought to be 1:40,000
Diagnostic Criteria
Neurofibromatosis type 1
Neurofibromatosis type 1 - mutation of neurofibromin chromosome 17q11.2. The diagnosis of NF1 is made if any two of the following seven criteria are met:
- Two or more neurofibromas on the skin or under the skin or one plexiform neurofibroma (a large cluster of tumors involving multiple nerves); Neurofibromas are the subcutaneous lumps that are characteristic of the disease and increase in number with age.
- Freckling of the groin or the axilla (arm pit).
- Café au lait spots (pigmented birthmarks). Six or more measuring 5 mm in greatest diameter in prepubertal individuals and over 15 mm in greatest diameter in postpubertal individuals
- Skeletal abnormalities, such as sphenoid dysplasia or thinning of the cortex of the long bones of the body (i.e. bones of the leg, potentially resulting in bowing of the legs)
- Lisch nodules (hamartomas of iris), freckling in the iris.
- Tumors on the optic nerve, also known as an optic glioma
- A first-degree relative with a diagnosis of NF1


Neurofibromatosis type 2
Neurofibromatosis type 2 - mutation of merlin chromosome 22q12
- bilateral tumors, acoustic neuromas on the vestibulocochlear nerve, located on the eighth cranial nerve leading to hearing loss
- In fact, the hallmark of NF 2 is hearing loss due to acoustic neuromas around the age of twenty
- the tumors may cause:
- headache
- balance problems, and Vertigo
- facial weakness/paralysis
- patients with NF2 may also develop other brain tumors, as well as spinal tumors
- Deafness and Tinnitus
- Any relative with NF-2, diagnosed or not
Schwannomatosis
Schwannomatosis - gene involved has yet to be identified
- Multiple Schwannomas occur.
- The Schwannomas develop on cranial, spinal and peripheral nerves.
- Chronic pain, and sometimes numbness, tingling and weakness.
- About 1/3 of patients have segmental Schwannomatosis, which means that the Schwannomas are limited to a single part of the body, such as an arm, a leg or the spine.
- Unlike the other forms of NF, the Schwannomas do not develop on vestibular nerves, and as a result, no loss of hearing is associated with Schwannomatosis.
- Patients with Schwannomatosis do not have learning disabilities related to the disease.
One must keep in mind, however, that neurofibromatosis can't occur in or affect any of the organ systems, whether that entails simply compressing them (from tumor growth) or in fact altering the organs in some fundamental way. This disparity in the disease is one of many factors that makes it difficult to diagnose, and eventually find a prognosis for.
Genetics and Hereditability
Neurofibromatosis type 1 is due to mutation on chromosome 17q11.2 , the gene product being Neurofibromin ( a GTPase activating enzyme).[2]
Neurofibromatosis type 2 is due to mutation on chromosome 22q , the gene product is Merlin, a cytoskeletal protein.
Both NF1 and NF2 are autosomal dominant disorders, meaning that only one copy of the mutated gene need be inherited to pass the disorder. A child of a parent with NF1 or NF2 and an unaffected parent will have a 50% chance of inheriting the disorder.
Complicating the question of heritability is the distinction between genotype and phenotype, that is, between the genetics and the actual manifestation of the disorder.
In the case of NF1, no clear links between genotype and phenotype have been found, and the severity and specific nature of the symptoms may vary widely among family members with the disorder.[3] In the case of NF2, however, manifestations are similar among family members; a strong genotype-phenotype correlation is believed to exist (ibid).
Both NF1 and NF2 can also appear to be spontaneous mutation, with no family history. These cases account for about one half of neurofibromatosis cases (ibid).
Similar to polydactyly, although NF is a dominant mutation, it is not prevalent in society. Neurofibromatosis-1 is found in approximately 1 in 2,500-3,000 live births (carrier incidence 0.0004, gene frequency 0.0002). NF-2 is less common, having one case in 50,000-120,000 live births.[4]
Mechanism
Neurofibromatosis affects humans on a genetic level, meaning that it either destroys, or renders defective a specific gene. NF-1
- The gene that NF-1 affects is large, on band 17q11.2. It encodes for a protein called neurofibromin, otherwise known as "the tumor suppressor" protein. Neurofibromatosis alters or weakens this protein, rapid, radical growth of cells is allowed all over the body, especially around the nervous system. This leads to the normal symptoms for neurofibromatosis - clumpings of these tumors, called neurofibromas and schwannomas.
- Less is known about the NF-2 linked gene. However, it is on band 22q1 and also codes for a protein, most likely one similar to NF-1's.
Effects
People with Neurofibromatosis can be affected in many different ways.
- There is a high incidence of learning disabilities in people with NF. It is believed that at least 50% of people with NF have learning disabilities of some type.
- increased chances of development of petit mal epilepsy (a Partial absence seizure disorder)
- The tumors that occur can grow anywhere a nerve is present. This means that:
- They can grow in places that are very visible to people that a patient may encounter on the street.
- The tumors can also grow in places that can cause other medical issues that may require them to be removed for the patient's safety.
- Affected individuals may need multiple surgeries, depending on where the tumors are located.
Treatment
Because there is no cure for the disease itself, the only therapy for people with neurofibromatosis is a program of treatment by a team of specialists to manage symptoms or complications. Surgery may be needed when the tumors compress organs or other structures. Less than 10% people with neurofibromatosis develop cancerous growths; in these cases, chemotherapy may be successful.[5]
History
Neurofibromatosis was discovered in 1882 by the German pathologist Friedrich Daniel von Recklinghausen. He wrote on it and published it in Hämochromatose, Tageblatt der Naturforschenden Versammlung.[6]
Joseph Merrick, the Elephant Man, was once considered to have been affected with either elephantiasis or neurofibromatosis type I. However, it is now generally believed that Merrick suffered from the very rare Proteus syndrome. This however has given rise to the common misconception that Neurofibromatosis and "Elephant Man Disease" are one and the same.
Related disorders
Neurofibromatosis is considered a member of the neurocutaneous syndromes (phakomatoses). In addition to the types of neurofibromatosis, the phakomatoses also include tuberous sclerosis, Sturge-Weber syndrome and von Hippel-Lindau disease. This grouping is an artifact of an earlier time in medicine, before the distinct genetic basis of each of these diseases was understood.
Case Examples
Case #1
Clinical Summary
This 45-year-old divorced white male came to the emergency room with severe hepatic cirrhosis and aspiration pneumonia. Shortly after admission he developed cardiac arrhythmias and died. Significant past history included alcohol abuse, cirrhosis, and neurofibromatosis. He had no family history of neurofibromatosis, but his condition was diagnosed at age 17 when he developed neurofibromas along the lateral chest wall. There was no history of continued follow-up after this initial diagnosis.
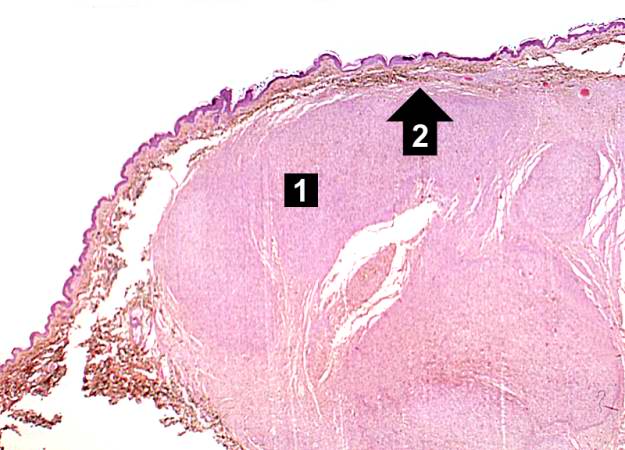
Autopsy Findings
The patient was covered with variably sized subcutaneous nodules ranging from 0.5 to 2.5 cm in diameter. Other significant findings included micronodular hepatic cirrhosis (liver weight: 1760 grams), ascites (500 ml), and splenomegaly (weight: 260 grams).
Histopathological Findings







See also
References
- ↑ http://www.merck.com/mmhe/sec06/ch088/ch088d.html Merck Manual Home Edition, "Neurofibromatosis"
- ↑ Fauci, et al Harrison's Principle of Internal Medicine 16th Ed. p 2453
- ↑ Korf, Bruce E. and Allan E. Rubenstein. 2005. Neurofibromatosis: A Handbook for Patients, Families, and Health Care Professionals.
- ↑ Jennifer R. Kam, Jan. 2007
- ↑ Neurofibromatosis. JAMA patient page, Vol. 300 No. 3, July 16, 2008.
- ↑ Template:WhoNamedIt
External links
- Information page from the National Institute of Neurological Disorders and Stroke (part of the National Institutes of Health in the United States) -- this Wikipedia article is based largely on this NINDS information page
- Vestibular Schwannoma (Acoustic Neuroma) and Neurofibromatosis at National Institute on Deafness and Other Communication Disorders
- Template:DMOZ
- Home Page of the Children's Tumor Foundation (a non-profit organization working towards a cure for Neurofibromatosis in the United States)
- Home page from NF Inc (a non-profit organization working towards Neurofibromatosis patient support in the United States)
- Home Page of the the Reggie Bibbs website (a non-profit organization working providing patient education, awareness and support of Neurofibromatosis in the United States)
Template:SIB Template:Nervous tissue tumors
de:Neurofibromatose it:Neurofibromatosi lt:Neurofibromatozė hu:Neurofibromatózis nl:Neurofibromatose no:Nevrofibromatose sv:Neurofibromatos