Sideroblastic anemia pathophysiology
| Sideroblastic anemia pathophysiology | |
 | |
|---|---|
| Sideroblastic (microcytic) anemia |
|
Sideroblastic anemia Microchapters |
|
Diagnosis |
|---|
|
Treatment |
|
Case Studies |
|
Sideroblastic anemia pathophysiology On the Web |
|
American Roentgen Ray Society Images of Sideroblastic anemia pathophysiology |
|
Risk calculators and risk factors for Sideroblastic anemia pathophysiology |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1] Associate Editor(s)-in-Chief: Nazia Fuad M.D.
Overview
Pathophysiology
Physiology
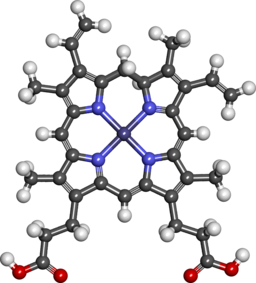 |
Heme is porphyrin containing compound, with an Fe iron ion in the centre,surrounded by heterocyclic organic ring of porphyrin.
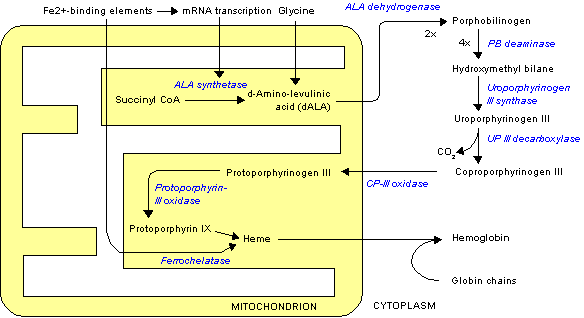
The normal physiology of heme synthesis can be understood as follows:[1]
- Mitochondria in the developing erythroid cells are the cellular site of heme production and iron utilization.
- Glycine combines with succinylcoA to form aminolenolinic acid(ALA)
- This reaction is catalyzed by ALA sunthetase enzyme (ALAS2) in mitochondria
- ALA synthetase requires vit B-6 as a cofactor
- Two molecules of aminolenolinic acid condense in cytosol to form porphobilinogen(PBG)
- This reaction is catalyzed by zinc containing enzyme called ALA dehydratase.
- Multiple enzymatic transformations in cytoplasm produce coproporphyrinogen III (CPG).
- Coproporphyrinogen III (CPG) enters the mitochondrion.
- Additional modifications of CPG in mitochondrion produces protoporphyrin IX.
- The final step is the insertion of iron into the protoporphyrin IX ring producing HEME.
- This final reaction is catalyzed by enzyme ferrochelatase.
Pathogenesis
 |
- It is understood that sideroblastic anemia is the result of defects in the steps of heme biosynthesis that occur within the mitochondrion.[2]
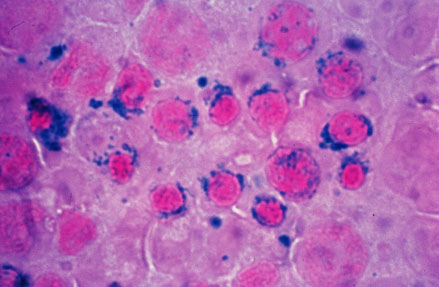
- Sideroblasts are the pathognomic feature of sideroblastic anemia.
- There is deffect in incorporation of iron in to heme.
- As a result the iron accumulates in mitochondria of red cell precursors
- Ring sideroblasts are erythroblasts that have iron-loaded mitochondria.
- The iron granules are arranged around the nucleus in a ring form
- They can be seen with prussian blue staining as blue granules around the nucleus.[3]
- The pathophysiology of sideroblastic anemia depends on the underlying cause.[4]
- The X-linked hereditary sideroblastic anemias result from mutations in the gene encoding ALAS2.
- Isoniazide, produces sideroblastic anemia in people who dont use pyridoxine prophylaxis,
- Pyridoxine is a cofactor for ALAS2 enzyme.
- Its deficiency directly impairs ALAS2 function
- Mitochondrial cytopathies
- Result from deletions of portions of the mitochondrial genome .
- The consequent marked mitochondrial dysfunction causes sideroblastic anemia in these disorders.
- Ethanol is the most common cause of toxin-induced sideroblastic anemia.
- Ethanol causes sideroblastic anemia by two mechanisms
- Direct antagonism to pyridoxal phosphate
- Dietary deficiency of this compound.
- The bone marrow shows sideroblasts and vacuoles in the normoblasts in ethanol toxicity.
- Lead intoxication causes sideroblastic anemia by inhibiting two enzymes in heme pathway:
- ALA dehaydratase
- Ferrochelatase
- Penicillamine or triethylene tetramine dihydrochloride (Trientene or TTH) used in treatment of Wilsonís disease can produce sideroblastic anemia.
- Excessive chelation produces copper deficiency.
- Copper catalyzes the last step in heme biosynthesis, insertion of iron into protoporphyrin IX.
- Zinc intoxication causes sideroblastic anemia in patients using large amount of zinc supplements.
- Excessive zinc reduces serum copper levels.
Mechanism of iron overload
Despite the abnormalities in iron utilization in sideroblastic anemia, iron transport to erythroblasts continues since the body senses anemia. Intestinal iron absorption increases which eventually causes both iron accumulation in mitochondria of erythroblasts and possible systemic iron accumulation. It is interesting to note that systemic iron overload occurs only in some forms of sideroblastic anemia, usually when the defects in iron metabolisms involve earlier stages of erythroid pathways
Genetics
The development of sideroblastic anemia is the result of multiple genetic mutations in several genes involved in heme synthesis resulting in autosomal recessive congenital sideroblastic anemia (ARCSA)
- SLC25A38 –SLC25A38 mutations is the most common. SLC25A38 encodes an erythroid-specific mitochondrial amino acid carrier that transports glycine into mitochondria for the first step in heme synthesis.
- GLRX5 – GLRX5 encodes protein used in the synthesis of iron-sulfur (Fe-S) clusters.
- HSPA9 – HSPA9 encodes the mitochondrial HSP70 homologue HSPA9, which is also involved in Fe-S cluster formation.
- FECH – FECH encodes ferrochelatase, the final enzyme in the heme synthetic pathway, which inserts an iron atom into protoporphyrin IX
- X-linked sideroblastic anemia with ataxia (ABCB7 mutation)
- Pearson syndrome ( mitochondrial DNA deletion)
- Pearson syndrome is a congenital condition
- It affects multiple systems,
- Results in severe sideroblastic anemia, thrombocytopenia,neutropenia.
- Pancreatic insufficiency, lactic acidosis, and growth retardation are other common features.
References
- ↑ Layer G, Reichelt J, Jahn D, Heinz DW (June 2010). "Structure and function of enzymes in heme biosynthesis". Protein Sci. 19 (6): 1137–61. doi:10.1002/pro.405. PMC 2895239. PMID 20506125.
- ↑ Fleming MD (2011). "Congenital sideroblastic anemias: iron and heme lost in mitochondrial translation". Hematology Am Soc Hematol Educ Program. 2011: 525–31. doi:10.1182/asheducation-2011.1.525. PMID 22160084.
- ↑ Cazzola M, Invernizzi R (June 2011). "Ring sideroblasts and sideroblastic anemias". Haematologica. 96 (6): 789–92. doi:10.3324/haematol.2011.044628. PMC 3105636. PMID 21632840.
- ↑ Fujiwara T, Harigae H (December 2013). "Pathophysiology and genetic mutations in congenital sideroblastic anemia". Pediatr Int. 55 (6): 675–9. doi:10.1111/ped.12217. PMID 24003969.