Castleman's disease: Difference between revisions
| Line 101: | Line 101: | ||
* [[Lymph node]] [[biopsy]] is used as a differentiating tool in the diagnosis of Castleman's disease. It is used to differentiate Castleman's from [[lymphoma]]. | * [[Lymph node]] [[biopsy]] is used as a differentiating tool in the diagnosis of Castleman's disease. It is used to differentiate Castleman's from [[lymphoma]]. | ||
* Variants of Castleman's disease can also be differentiated using biopsy. | * Variants of Castleman's disease can also be differentiated using biopsy. | ||
{| align="center" | |||
! | |||
|-valign="top" | |||
| [[Image:Castleman_disease_-_hyaline_vascular_variant.jpg|thumb|Micrograph of Castleman's disease, hyaline vascular variant, exhibiting the characteristically expanded mantle zone and a radially penetrating sclerotic blood vessel ("lollipop" sign). H&E stain.]] | |||
| [[Image:Castleman_disease_-_Plasma_cell_variant.jpg|thumb|Intermediate magnification micrograph of Castleman disease showing the characteristic expansion of the mantle zone, known as "onion skinning". H&E stain.]] | |||
|} | |||
==Treatment== | ==Treatment== | ||
Revision as of 13:46, 6 August 2012
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]; Associate Editor(s)-in-Chief: Raviteja Guddeti, M.B.B.S. [2]
Synonyms and keywords: Angiofollicular lymph node hyperplasia; lymphoid hamartoma
Overview
Castleman's disease is a rare disorder characterized by non-cancerous growths (tumors) that may develop in the lymph node tissue throughout the body. It involves hyperproliferation of certain B cells that often produce cytokines.
Historical Perspective
In 1954 Dr. Benjamin Castleman, a pathologist described an unusual histopathology of a lymph node in a patient with mediastinal mass.
Classification
2 types of classifications exist for Castleman's disease. They are:
- Clinical and Radiologic classification:
- Unicentric - single lymph node is involved, most commonly in the mediastinum or the mesentery.
- Multicentric - wide spread involvement of lymph nodes and also liver and spleen in some cases
- Histopathologic classification:
- Hyaline vascular
- Plasmacytic
- Mixed cellularity - has features of both hyaline vascular type and plasmacytic type.
Pathophysiology
In all cases, Castleman's disease is likely due to hypersecretion of the cytokine IL-6. In KSHV positive tumors, this is most likely due to expression of the a virus-encoded cytokine, vIL-6, while KSHV negative tumors appear to be the result of over secretion of human IL-6.
Associated Conditions
Castleman's disease is sometimes associated with:
Causes
- About 50% of Multicentric Castleman's disease (MCD) is caused by Kaposi's sarcoma-associated herpesvirus (KSHV), a gammaherpesvirus that is also the cause of Kaposi's sarcoma and primary effusion lymphoma, while the remainder of MCD are of unknown cause.
- The form of MCD most closely associated with KSHV is the plasmacytic form of Castleman's disease while another pathologic form, the hyaline-vascular form, is generally negative for this virus.
Epidemiology and Demographics
Age
- Average age of the patients with unicentric disease is 30 - 40 yrs
- For multicentric disease it is 50 - 60 yrs
Gender
- No gender differentiation is seen in the occurrence of the disease.
Risk Factors
- HIV/AIDS can act as a risk factor for this disease. The course of the disease is worse in these patients.
Natural History, Complications and Prognosis
Complications
- Life threatening infections
- Multi organ failure
- Kaposi sarcoma
- Lymphoma
- Death
Prognosis
- Prior to 1996 MCD carried a poor prognosis of about 2 years, due to autoimmune hemolytic anemia and non-Hodgkin's lymphoma which may arise as a result of proliferation of infected cells. The timing of diagnosis, with particular attention to the difficulty of determining the cause of B symptoms without a CT scan and lymph node biopsy, may impact significantly on the prognosis and risk of death. Left untreated, MCD usually gets worse and becomes increasingly difficult and unresponsive to current treatment regimens.
- HIV patients with multicentric disease have a grave prognosis. They have a less favorable clinical course and tend to develop Kaposi sarcoma and even plasmablastic non-Hodgkin lymphoma.
Diagnosis
Symptoms
The most common 'B symptoms' of MCD are
Physical Examination
Vitals
Skin
Head
Abdomen
Laboratory Findings
- Complete blood count and differential count - low white blood cell counts, which may to be due to the overproduction of interleukin 6.
- Erythrocyte sedimentation rate - elevated in 80% cases.
Imaging
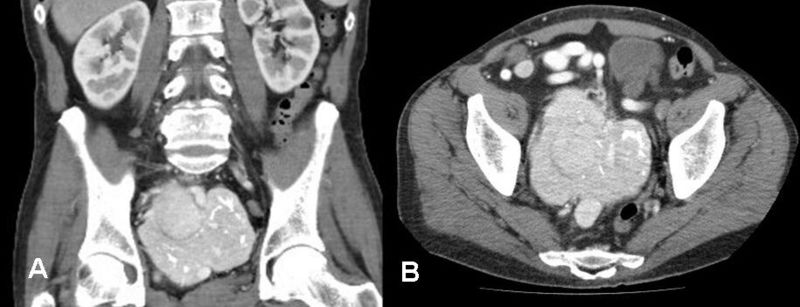
CT
- To detect the enlarged lymph nodes in the chest, neck, abdomen, groin.
- Enlargement of liver and spleen can also be detected.
- Findings include:
- Contrast enhancement
- Homogenous
PET Scan
- To diagnose the extent of involvement of the disease and to assess the effect of treatment.
Biopsy
- Lymph node biopsy is used as a differentiating tool in the diagnosis of Castleman's disease. It is used to differentiate Castleman's from lymphoma.
- Variants of Castleman's disease can also be differentiated using biopsy.
Treatment
Unicentric
In the Unicentric form of the disease, surgical resection is often curative,[1] [2] and the prognosis is excellent.
Multicentric
There is no standard therapy for MCD at the moment.
It is important to distinguish AIDS-related Multicentric Castleman’s disease from other forms of Multicentric Castleman’s disease. Treatment for the former can be focused upon the same protocols used for treating the underlying AIDS.[3]
Recent work with HIV-positive patients with KSHV-related MCD suggests that treatment with the antiherpesvirus drug ganciclovir or the antiCD20 B cell monoclonal antibody, rituximab, may markedly improve outcome. These drugs target and kill B cells via the B cell specific CD20 marker. Since B cells are required for the production of antibodies, the body's immune response is weakened whilst on treatment and the risk of further viral or bacterial infection is increased. Due to the uncommon nature of the condition there are not many large scale research studies from which standardized approaches to therapy may be drawn, and the extant case studies of individuals or small cohorts should be read with caution. As with many diseases, the patient's age, physical state and previous medical history with respect to infections may impact on the disease progression and outcome.
Use of tocilizumab has been proposed.[4]
Siltuximab, a monoclonal antibody that binds interleukin-6, is currently being investigated in a Phase II clinical trial.[5]
Other treatments for multicentric castleman disease include the following:
References
- ↑ name=pmid21934347
- ↑ Talarico F, Negri L, Iusco D, Corazza GG (2008). "Unicentric Castleman's disease in peripancreatic tissue: case report and review of the literature". G Chir. 29 (4): 141–4. PMID 18419976. Unknown parameter
|month=ignored (help) - ↑ Sprinz E, Jeffman M, Liedke P, Putten A, Schwartsmann G (2004). "Successful treatment of AIDS-related Castleman's disease following the administration of highly active antiretroviral therapy (HAART)". Ann. Oncol. 15 (2): 356–8. doi:10.1093/annonc/mdh066. PMID 14760135. Unknown parameter
|month=ignored (help) - ↑ Matsuyama M, Suzuki T, Tsuboi H; et al. (2007). "Anti-interleukin-6 receptor antibody (tocilizumab) treatment of multicentric Castleman's disease" (– Scholar search). Intern. Med. 46 (11): 771–4. doi:10.2169/internalmedicine.46.6262. PMID 17541233.[dead link]
- ↑ A Study to Evaluate the Safety of Long-term Treatment With Siltuximab in Patients With Multicentric Castleman's Disease ClinalTrails.gov.
- ↑ http://www.mayoclinic.com/health/castleman-disease/DS01000/DSECTION=treatments-and-drugs
- Aoki Y, Yarchoan R, Wyvill K, Okamoto S, Little RF, Tosato G. Detection of viral interleukin-6 in Kaposi sarcoma-associated herpesvirus-linked disorders. Blood 2001;97(7):2173-6.
- Yarchoan R, Little RF. Immunosuppression-related malignancies. In: DeVita Jr. VT, Hellman S, Rosenberg SA, eds. Cancer, Principles and Practice of Oncology 6th Edition. Philadelphia: Lippincott Williams and Wilkins; 2001:2575-97.

