Lower gastrointestinal bleeding pathophysiology: Difference between revisions
Aditya Ganti (talk | contribs) |
Aditya Ganti (talk | contribs) |
||
| Line 82: | Line 82: | ||
:* '''<u>Ulcerative colitis</u>''' | :* '''<u>Ulcerative colitis</u>''' | ||
:** In ulcerative colitis T cells cytotoxic to the colonic epithelium accumulate in the lamina propria, accompanied by B cells that secrete immunoglobulin G (IgG) and IgE. | :** In ulcerative colitis T cells cytotoxic to the colonic epithelium accumulate in the lamina propria, accompanied by B cells that secrete immunoglobulin G (IgG) and IgE. | ||
:** This results in inflammation of the crypts of Lieberkuhn, with abscesses and pseudopolyps | :** This results in inflammation of the crypts of Lieberkuhn, with abscesses and pseudopolyps along with rupturing of minute blood vessels in mucosa resulting in bleeding. | ||
*'''<u>Neoplasia</u>''' | *'''<u>Neoplasia</u>''' | ||
:*Mutations of multiple genes are required for the formation of adenocarcinoma, including the APC gene, Kras, DCC, and p53. | :*Mutations of multiple genes are required for the formation of adenocarcinoma, including the APC gene, Kras, DCC, and p53. | ||
:*Certain hereditary syndromes are also classified by defects in DNA mismatch repair genes and microsatellite instability. | :*Certain hereditary syndromes are also classified by defects in DNA mismatch repair genes and microsatellite instability. | ||
:* | :*As tumor grows it invades the surrounding tissue disrupting the normal vasculature along with it | ||
:*Therefore tumors tend to bleed slowly, and patients present with hemocult positive stools and microcytic anemia. | |||
*'''<u>AV Malformation/Angiodysplasia</u>''' | *'''<u>AV Malformation/Angiodysplasia</u>''' | ||
:*In AV malformation direct connections between arteries and veins occur in the colonic submucosa. | :*In AV malformation direct connections between arteries and veins occur in the colonic submucosa. | ||
:*The lack of capillary buffers causes high pressure blood to enter directly into the venous system, making these vessels at high risk of rupture into the bowel lumen. | :*The lack of capillary buffers causes high pressure blood to enter directly into the venous system, making these vessels at high risk of rupture into the bowel lumen. | ||
:*In Angiodysplasia over time, previously healthy blood vessels of the cecum and ascending colon degenerate and become prone to bleeding. | :*In Angiodysplasia over time, previously healthy blood vessels of the cecum and ascending colon degenerate and become prone to bleeding. | ||
==Gross and Microscopic Pathology== | ==Gross and Microscopic Pathology== | ||
Revision as of 19:01, 13 December 2017
|
Lower gastrointestinal bleeding Microchapters |
|
Differentiating Lower gastrointestinal bleeding from other Diseases |
|---|
|
Diagnosis |
|
Treatment |
|
Management |
|
Surgery |
|
Case Studies |
|
Lower gastrointestinal bleeding pathophysiology On the Web |
|
American Roentgen Ray Society Images of Lower gastrointestinal bleeding pathophysiology |
|
Risk calculators and risk factors for Lower gastrointestinal bleeding pathophysiology |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]; Associate Editor(s)-in-Chief: Aditya Ganti M.B.B.S. [2]
Overview
Pathophysiology
Blood supply
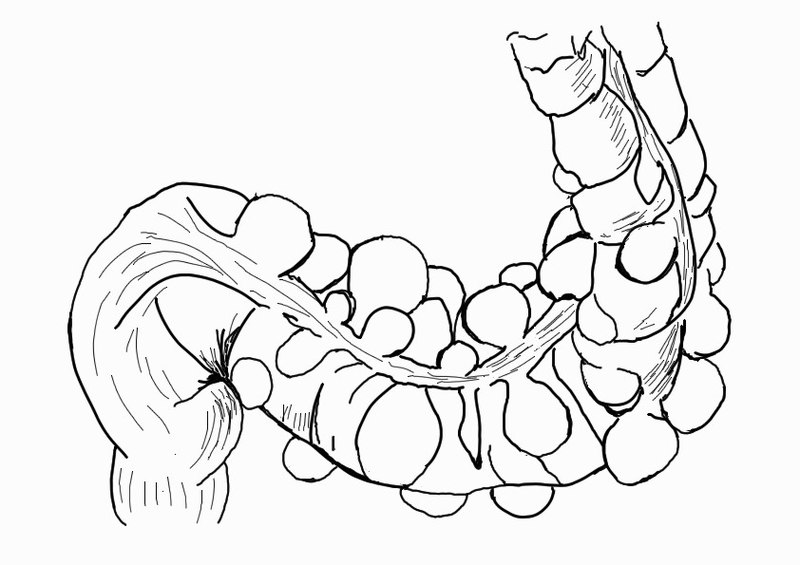
- Superior mesentric artery and inferior mesentric artery are the two major blood vessels that supply lower gastrointestinal tract.
- The superior mesentric artery and inferior mesentric artery are interconnected through a branch of anatomizing branches which are collectively called as marginal artery of Drummond.
- This vascular arcade runs in the mesentery close to the bowel.
| Lower GI Tract | Arterial Supply | Venous Drainage | |
|---|---|---|---|
| Midgut |
|
|
|
| Hindgut |
|
|
|
| ɸ -Except lower rectum, which drains into the systemic circulation. | |||

Source: By Anpol42 (Own work) [CC BY-SA 4.0 (https://creativecommons.org/licenses/by-sa/4.0)], via Wikimedia Commons
Pathogenesis
The pathogenesis of lower gastrointestinal bleeding can be discussed based on the etiology. Diverticulosis is the most common etiology of lower GI bleeding accounting for 30% of all cases, followed by anorectal disease, ischemia, inflammatory bowel disease (IBD), neoplasia and arteriovenous (AV) malformations.
- Diverticulosis
- The colonic wall weakens with age and results in the formation of saclike protrusions known as diverticula.
- These protrusions generally occur at the junction of blood vessel penetrating through the mucosa and circular muscle fibers of the colon resulting in painless bleeding
- Despite the majority of diverticula being on the left side of the colon, diverticular bleeding originates from the right side of the colon in 50% to 90% of instances.
Source:By Anpol42 (Own work) [CC BY-SA 4.0 (https://creativecommons.org/licenses/by-sa/4.0)], via Wikimedia Commons
- Anorectal disease
- Hemorrhoids are engorged vessels in the normal anal cushions. When swollen, this tissue is very friable and susceptible to trauma, which leads to painless, bright red bleeding.
- Anal fissures are defined as a tear in the anal mucosa. With the passage of stool, the mucosa continues to tear and leads to bright red bleeding.
- Mesenteric Ischemia
- Mesenteric ischemia results when there is inadequate blood supply at the level of the small intestine.
- 2 or more vessels (celiac ,SMA, or IMA) must be involved for bleeding to occur.
- Non occlusive mesenetric ischemia affects critically ill patients who are vasopressor-dependent.
- Venous thrombosis of the visceral vessels can also precipitate an acute ischemic event.
- Decreased blood flow leads to transmural infarction with necrosis and perforation.
- Associated mucosal sloughing results in bleeding.
- Ischemic Colitis
- Ischemic colitis is caused by poor perfusion of the colon, which results in the inability of that area of the colon to meet its metabolic demands.
- It can be gangrenous or nongangrenous, acute, transient, or chronic.
- The left colon is predominantly affected, with the splenic flexure having increased susceptibility.
- Intraluminal hemorrhage occurs as the mucosa becomes necrotic, sloughs, and bleeds.
- Damage to the tissue is caused both with the ischemic insult as well as reperfusion injury.
- Inflammatory Bowel Disease
- Crohn's diseas
- In Crohn's disease T cell activation stimulates interleukin (IL)-12 and tumor necrosis factor (TNF)-a, which causes chronic inflammation and tissue injury.
- Initially, inflammation starts focally around the crypts, followed by superficial ulceration of the mucosa.
- The deep mucosal layers are then invaded in a noncontinuous fashion, and noncaseating granulomas form, which can invade through the entire thickness of the bowel and into the mesentery and surrounding structures resulting in bleeding
- Crohn's diseas
- Ulcerative colitis
- In ulcerative colitis T cells cytotoxic to the colonic epithelium accumulate in the lamina propria, accompanied by B cells that secrete immunoglobulin G (IgG) and IgE.
- This results in inflammation of the crypts of Lieberkuhn, with abscesses and pseudopolyps along with rupturing of minute blood vessels in mucosa resulting in bleeding.
- Ulcerative colitis
- Neoplasia
- Mutations of multiple genes are required for the formation of adenocarcinoma, including the APC gene, Kras, DCC, and p53.
- Certain hereditary syndromes are also classified by defects in DNA mismatch repair genes and microsatellite instability.
- As tumor grows it invades the surrounding tissue disrupting the normal vasculature along with it
- Therefore tumors tend to bleed slowly, and patients present with hemocult positive stools and microcytic anemia.
- AV Malformation/Angiodysplasia
- In AV malformation direct connections between arteries and veins occur in the colonic submucosa.
- The lack of capillary buffers causes high pressure blood to enter directly into the venous system, making these vessels at high risk of rupture into the bowel lumen.
- In Angiodysplasia over time, previously healthy blood vessels of the cecum and ascending colon degenerate and become prone to bleeding.
Gross and Microscopic Pathology
| Disease | Gross Pathology | Microscopic Pathology |
|---|---|---|
| Diverticulosis |
|
|
| Angiodysplasia |
|
|
| Hemorrhoids |
|
|
| Mesenteric ischemia |
|
|
| Ischemic colitis |
|
|
| Crohn's disease |
|
|
| Ulcerative colitis |
|
|