Osteoporosis X-ray: Difference between revisions
No edit summary |
No edit summary |
||
| Line 5: | Line 5: | ||
==Overview== | ==Overview== | ||
[[X-rays|X-ray]] may be helpful in the [[diagnosis]] of [[osteoporosis]]. The main finding on [[ | [[X-rays|X-ray]] may be helpful in the [[diagnosis]] of [[osteoporosis]]. The main finding on [[X-ray]] suggestive of [[osteoporosis]] is [[Bone loss|bone mass loss]], identified with decreased bony [[trabecula]] in primary stages and then decreased [[Cortical bone|cortical thickness]]. The most common [[bones]] monitored for [[osteoporosis]] evidences are [[femoral neck]], [[lumbar vertebrae]], and [[calcaneus]]. [[Radiography|Plain radiography]] needs at least 30-50% of [[bone]] loss to demonstrate decreased [[bone density]]; therefore, it is not a very sensitive [[modality]]. | ||
==X-ray== | ==X-ray== | ||
[[X-rays|X-ray]] may be helpful in the [[diagnosis]] of [[osteoporosis]]. The main finding on [[x-ray]] suggestive of [[osteoporosis]] is [[bone]] | [[X-rays|X-ray]] may be helpful in the [[diagnosis]] of [[osteoporosis]]. The main finding on [[x-ray]] suggestive of [[osteoporosis]] is [[Bone loss|bone mass loss]], identified with decreased bony [[trabecula]] in primary stages and then decreased [[Cortical bone|cortical thickness]]. The most common [[bones]] monitored for [[osteoporosis]] evidences are [[femoral neck]], [[lumbar vertebrae]], and [[calcaneus]]. [[Radiography|Plain radiography]] needs at least 30-50% of [[bone]] loss to demonstrate decreased [[bone density]]; therefore, it is not a very sensitive [[modality]]. | ||
{| align="right" | {| align="right" | ||
| Line 17: | Line 17: | ||
=== Indications for imaging === | === Indications for imaging === | ||
Consider vertebral imaging tests for the following individuals: | Consider [[vertebral]] imaging tests for the following individuals: | ||
* All women age 70 and older and all men age 80 and older if [[Bone mineral density|BMD]] T-score at the [[spine]], total [[hip]], or [[femoral neck]] is ≤−1.0 | * All women age 70 and older and all men age 80 and older if [[Bone mineral density|BMD]] T-score at the [[spine]], total [[hip]], or [[femoral neck]] is ≤−1.0 | ||
* Women age 65 to 69 and men age 70 to 79 if [[Bone mineral density|BMD]] T-score at the [[spine]], total [[hip]], or [[femoral neck]] is ≤−1.5 | * Women age 65 to 69 and men age 70 to 79 if [[Bone mineral density|BMD]] T-score at the [[spine]], total [[hip]], or [[femoral neck]] is ≤−1.5 | ||
* [[Postmenopausal]] women and men age 50 and older with specific risk factors, include: | * [[Postmenopausal]] women and men age 50 and older with specific risk factors, include: | ||
** Low-trauma fracture during adulthood (age 50 and older) | ** Low-trauma [[fracture]] during adulthood (age 50 and older) | ||
** Historical height loss of 1.5 in or more (4 cm) | ** Historical height loss of 1.5 in or more (4 cm) | ||
** Prospective height loss of 0.8 in or more (2 cm) | ** Prospective height loss of 0.8 in or more (2 cm) | ||
| Line 29: | Line 29: | ||
* The major findings correlated to [[osteoporosis]] in [[lumbar vertebrae]] are include: | * The major findings correlated to [[osteoporosis]] in [[lumbar vertebrae]] are include: | ||
** [[Wedges|Wedge shape]] of [[vertebrae]] (decreasing anterior aspect of the body) | ** [[Wedges|Wedge shape]] of [[vertebrae]] (decreasing anterior aspect of the body) | ||
** Picture frame vertebrae (decreased [[cortical bone]] in periphery) | ** Picture frame [[vertebrae]] (decreased [[cortical bone]] in periphery) | ||
** Ghost [[vertebrae]] (decreased [[trabecular bone]] in the body) | ** Ghost [[vertebrae]] (decreased [[trabecular bone]] in the body) | ||
** Vertebra plana (severe [[compression fracture]])<ref name="urlOsteoporosis | Radiology Reference Article | Radiopaedia.org">{{cite web |url=https://radiopaedia.org/articles/osteoporosis-3 |title=Osteoporosis | Radiology Reference Article | Radiopaedia.org |format= |work= |accessdate=}}</ref> | ** [[Vertebra]] plana (severe [[compression fracture]])<ref name="urlOsteoporosis | Radiology Reference Article | Radiopaedia.org">{{cite web |url=https://radiopaedia.org/articles/osteoporosis-3 |title=Osteoporosis | Radiology Reference Article | Radiopaedia.org |format= |work= |accessdate=}}</ref> | ||
==== Femoral neck ==== | ==== Femoral neck ==== | ||
Revision as of 16:51, 17 August 2017
|
Osteoporosis Microchapters |
|
Diagnosis |
|---|
|
Treatment |
|
Medical Therapy |
|
Case Studies |
|
Osteoporosis X-ray On the Web |
|
American Roentgen Ray Society Images of Osteoporosis X-ray |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]; Associate Editor(s)-in-Chief: Eiman Ghaffarpasand, M.D. [2]
Overview
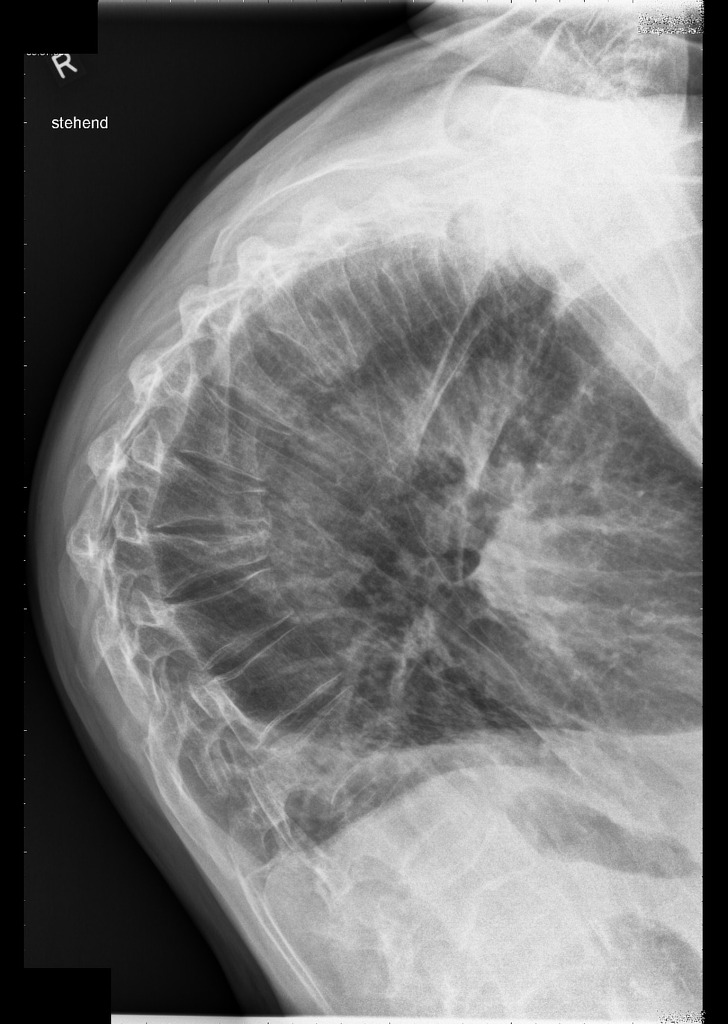
X-ray may be helpful in the diagnosis of osteoporosis. The main finding on X-ray suggestive of osteoporosis is bone mass loss, identified with decreased bony trabecula in primary stages and then decreased cortical thickness. The most common bones monitored for osteoporosis evidences are femoral neck, lumbar vertebrae, and calcaneus. Plain radiography needs at least 30-50% of bone loss to demonstrate decreased bone density; therefore, it is not a very sensitive modality.
X-ray
X-ray may be helpful in the diagnosis of osteoporosis. The main finding on x-ray suggestive of osteoporosis is bone mass loss, identified with decreased bony trabecula in primary stages and then decreased cortical thickness. The most common bones monitored for osteoporosis evidences are femoral neck, lumbar vertebrae, and calcaneus. Plain radiography needs at least 30-50% of bone loss to demonstrate decreased bone density; therefore, it is not a very sensitive modality.
 |
Indications for imaging
Consider vertebral imaging tests for the following individuals:
- All women age 70 and older and all men age 80 and older if BMD T-score at the spine, total hip, or femoral neck is ≤−1.0
- Women age 65 to 69 and men age 70 to 79 if BMD T-score at the spine, total hip, or femoral neck is ≤−1.5
- Postmenopausal women and men age 50 and older with specific risk factors, include:
- Low-trauma fracture during adulthood (age 50 and older)
- Historical height loss of 1.5 in or more (4 cm)
- Prospective height loss of 0.8 in or more (2 cm)
- Recent or ongoing long-term glucocorticoid treatment[1]
Lumbar vertebrae
- The major findings correlated to osteoporosis in lumbar vertebrae are include:
- Wedge shape of vertebrae (decreasing anterior aspect of the body)
- Picture frame vertebrae (decreased cortical bone in periphery)
- Ghost vertebrae (decreased trabecular bone in the body)
- Vertebra plana (severe compression fracture)[2]
Femoral neck
- Singh's index: Categorization of femoral neck bone mineral density upon visual scale of the trabecular bone existence on x-ray.
- The Singh's categories include:
- Grade 1: Thin principle compression trabeculae
- Grade 2: Principle compression trabeculae
- Grade 3: Thin principle tensile trabeculae, with discontinuity
- Grade 4: Thin principle tensile trabeculae, with continuity
- Grade 5: Thin principle tensile and compression trabeculae
- Grade 6: Normal appearance
- Reduced density of trabecular bone in the area, which is described by means of Singh's index (grades 3, 2, and 1), could reflect the diagnosis of osteoporosis[3]
Tubular bones
- Osteoporosis in these bones, especially metacarpals and metatarsals, appeared as loss of cortical thickness. However, cortical thickness of less than 25% of entire bone demonstrate osteoporosis.[2]
-
Pathological fracture in T12 and L1 (saggital view); Case courtesy of Dr Roberto Schubert, Radiopaedia.org, rID: 17333
-
Pathological fracture in T12 and L1 (axial view); Case courtesy of Dr Roberto Schubert, Radiopaedia.org, rID: 17333
-
Dowager's hump; Case courtesy of Dr Roberto Schubert, Radiopaedia.org, rID: 18147
References
- ↑ Cosman F, de Beur SJ, LeBoff MS, Lewiecki EM, Tanner B, Randall S; et al. (2014). "Clinician's Guide to Prevention and Treatment of Osteoporosis". Osteoporos Int. 25 (10): 2359–81. doi:10.1007/s00198-014-2794-2. PMC 4176573. PMID 25182228.
- ↑ 2.0 2.1 "Osteoporosis | Radiology Reference Article | Radiopaedia.org".
- ↑ "Singh index | Radiology Reference Article | Radiopaedia.org".