Osteoporosis other imaging findings: Difference between revisions
No edit summary |
No edit summary |
||
| Line 1: | Line 1: | ||
__NOTOC__ | __NOTOC__ | ||
{{Osteoporosis}} | {{Osteoporosis}} | ||
{{CMG}} | {{CMG}}; {{EG}} | ||
==Overview== | ==Overview== | ||
Revision as of 22:30, 14 August 2017
|
Osteoporosis Microchapters |
|
Diagnosis |
|---|
|
Treatment |
|
Medical Therapy |
|
Case Studies |
|
Osteoporosis other imaging findings On the Web |
|
American Roentgen Ray Society Images of Osteoporosis other imaging findings |
|
Risk calculators and risk factors for Osteoporosis other imaging findings |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]; Eiman Ghaffarpasand, M.D. [2]
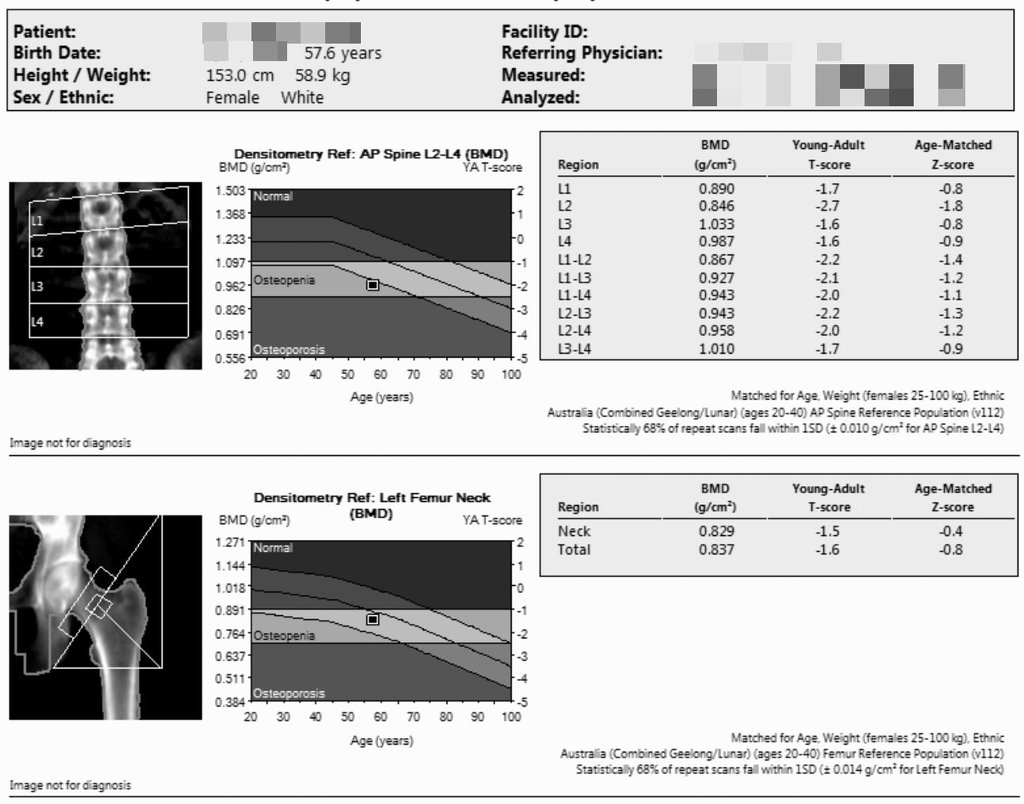
Overview
The most important modality for measuring bone mineral density (BMD), that every osteoporosis diagnostic and therapeutic decision are based on, is dual energy X-ray absorptiometry (DEXA). DEXA is a 2-dimensional image of a 3-demensional subject, mainly depends on size of the bone which is studied. Regarding the vast advantages of DEXA, it seems that DEXA will remain the masterpiece of fracture risk assessment and also osteoporosis diagnosis in the future.
Finite element modeling (FEM) is basically an engineering computer-based simulation software. FEM typically simulate the physical loading effects on materials. The effects may be strain or compression, while the subject determined as net-like elements connected to each other.
BMD is focused on density and does not imply for microstructure or architecture of bones. One of the most powerful methods to determine the microstructure is trabecular bone score (TBS) as a complementary method for DEXA.
Osteoporosis other imaging findings
Dual energy X-ray absorptiometery (DEXA, DXA)
- The most important modality for measuring bone mineral density (BMD), that every osteoporosis diagnostic and therapeutic decision are based on, is dual energy X-ray absorptiometry (DEXA).[1] DEXA is a 2-dimensional image of a 3-demensional subject, mainly depends on size of the bone which is studied; therefore, it would explain the variety of BMD upon sex, body weight, and also ethnicity.[2]
- Considering the effect of bone size on 2-dimensional image of DEXA, the measured BMD is not reflecting the exact BMD; however, the DEXA fracture prediction would be better than 3-dimansional images, because small bones fractured easily than large bones.[3]
- DEXA is the choice modality because of the following factors:
- There are many factors influencing the osteoporosis diagnosis, such as trabecular bone architecture; however, DEXA is the best predictor of osteoporosis and osteoporotic fractures by means of central BMD surveys.[5]
- For adults, it has to be always two sites of BMD measurement, lumbar spine and femoral neck; in case each of them is impossible to evaluate, forearm will be substituted.[6]
- For children (less than 20 years old), femoral maturity level may be different among population, leading to lack of unique reference measure; thus, just one site of measurement (i.e., lumbar spine) is considered.[7]
- Upon the world health organization (WHO) report in 1994, using T-score (standard deviations (SD) below or above the average of young Caucasian women), BMD measures are divided into three groups, include:
- T-score greater than -1.0 SD assumed as normal BMD
- T-score between -1.0 and -2.5 SD assumed as osteopenia
- T-score less than -2.5 SD assumed as osteoporosis[8]
- Z-score is same as the T-score, but the target population is matched for age, sex, race, and also in some studies, weight.
- Using DEXA in men, almost always show higher BMD levels. But regarding the effect of bone size on DEXA measured BMD levels, it seems that higher BMD levels may be due to larger bones in men. Surprisingly, after matching the BMD levels, it is concluded that volumetric BMD is even lower in men. However, their fracture risk is same as women's risk; thus, the women's reference range of BMD is assumed for men, too.[9]
- Regarding the vast advantages of DEXA (low radiation exposure, high availability, and tremendous information related to fracture risk), it seems that DEXA will remain the masterpiece of fracture risk assessment and also osteoporosis diagnosis.[10]
Finite element modelling (FEM)
- Finite element modeling (FEM) is basically an engineering computer-based simulation software. FEM typically simulate the physical loading effects on materials. The effects may be strain or compression, while the subject determined as net-like elements connected to each other.
- Currently, basic models for FEM is provided through vQCT scanners, and then elastic properties of bone been measured by use of bone mineral density (BMD) of the position. Finally, all of the anisotropic, inhomogeneous, and complex geometry of the bone are presented.
- Studies have shown that however osteoporotic vertebrae are capable of bearing daily stresses as same as normal bones, but the stress that is encountered the osteoporotic bone during forward bending may be more severe.[11]
Trabecular bone score (TBS)
- Fracture risk assessment is very important in osteoporosis. It is based on couple of factors, include age, body weight, and some past medical histories (e.g., smoking or alcohol use); and is measured by means of BMD assessment through DEXA scans.
- The main limitation of using BMD as identifier of osteoporosis is that the BMD is focused on density and does not imply for microstructure or architecture of bones, at all. One of the most powerful methods to determine the microstructure is trabecular bone score (TBS) as a complementary method for DEXA.
- TBS is a texture identifier of bones, measured and extracted from DEXA scan findings. TBS findings are including:
- The literature support the use of TBS along with BMD to predict the fracture risk more precisely.[12]
- The major characteristics of TBS are as follow:
- TBS is reduced in postmenopausal women
- TBS is reduced in men with previous osteoporotic fractures
- TBS is complementary for lumbar spine DEXA
- TBS is reduced in women who experienced osteoporotic fractures (in whom DEXA was normal)
- TBS is the same as lumbar spine BMD in predicting fracture risk in postmenopausal women
- TBS is associated with fractures induced by bone mass loss[13]
References
- ↑ Messina C, Monaco CG, Ulivieri FM, Sardanelli F, Sconfienza LM (2016). "Dual-energy X-ray absorptiometry body composition in patients with secondary osteoporosis". Eur J Radiol. 85 (8): 1493–8. doi:10.1016/j.ejrad.2016.03.018. PMID 27048946.
- ↑ Seeman E (1998). "Growth in bone mass and size--are racial and gender differences in bone mineral density more apparent than real?". J. Clin. Endocrinol. Metab. 83 (5): 1414–9. doi:10.1210/jcem.83.5.4844. PMID 9589631.
- ↑ Black DM, Bouxsein ML, Marshall LM, Cummings SR, Lang TF, Cauley JA, Ensrud KE, Nielson CM, Orwoll ES (2008). "Proximal femoral structure and the prediction of hip fracture in men: a large prospective study using QCT". J. Bone Miner. Res. 23 (8): 1326–33. doi:10.1359/jbmr.080316. PMC 2680175. PMID 18348697.
- ↑ Cummings SR, Bates D, Black DM (2002). "Clinical use of bone densitometry: scientific review". JAMA. 288 (15): 1889–97. PMID 12377088.
- ↑ Lorente-Ramos R, Azpeitia-Armán J, Muñoz-Hernández A, García-Gómez JM, Díez-Martínez P, Grande-Bárez M (2011). "Dual-energy x-ray absorptiometry in the diagnosis of osteoporosis: a practical guide". AJR Am J Roentgenol. 196 (4): 897–904. doi:10.2214/AJR.10.5416. PMID 21427343.
- ↑ Baim S, Binkley N, Bilezikian JP, Kendler DL, Hans DB, Lewiecki EM, Silverman S (2008). "Official Positions of the International Society for Clinical Densitometry and executive summary of the 2007 ISCD Position Development Conference". J Clin Densitom. 11 (1): 75–91. doi:10.1016/j.jocd.2007.12.007. PMID 18442754.
- ↑ Baim S, Leonard MB, Bianchi ML, Hans DB, Kalkwarf HJ, Langman CB, Rauch F (2008). "Official Positions of the International Society for Clinical Densitometry and executive summary of the 2007 ISCD Pediatric Position Development Conference". J Clin Densitom. 11 (1): 6–21. doi:10.1016/j.jocd.2007.12.002. PMID 18442749.
- ↑ "WHO IRIS: Assessment of fracture risk and its application to screening for postmenopausal osteoporosis : report of a WHO study group [meeting held in Rome from 22 to 25 June 1992]".
- ↑ Srinivasan B, Kopperdahl DL, Amin S, Atkinson EJ, Camp J, Robb RA, Riggs BL, Orwoll ES, Melton LJ, Keaveny TM, Khosla S (2012). "Relationship of femoral neck areal bone mineral density to volumetric bone mineral density, bone size, and femoral strength in men and women". Osteoporos Int. 23 (1): 155–62. doi:10.1007/s00198-011-1822-8. PMC 3640410. PMID 22057550.
- ↑ Jain RK, Vokes T (2017). "Dual-energy X-ray Absorptiometry". J Clin Densitom. doi:10.1016/j.jocd.2017.06.014. PMID 28716497.
- ↑ Genant HK, Engelke K, Prevrhal S (2008). "Advanced CT bone imaging in osteoporosis". Rheumatology (Oxford). 47 Suppl 4: iv9–16. doi:10.1093/rheumatology/ken180. PMC 2427166. PMID 18556648.
- ↑ Shevroja E, Lamy O, Kohlmeier L, Koromani F, Rivadeneira F, Hans D (2017). "Use of Trabecular Bone Score (TBS) as a Complementary Approach to Dual-energy X-ray Absorptiometry (DXA) for Fracture Risk Assessment in Clinical Practice". J Clin Densitom. doi:10.1016/j.jocd.2017.06.019. PMID 28734710.
- ↑ Silva BC, Leslie WD, Resch H, Lamy O, Lesnyak O, Binkley N, McCloskey EV, Kanis JA, Bilezikian JP (2014). "Trabecular bone score: a noninvasive analytical method based upon the DXA image". J. Bone Miner. Res. 29 (3): 518–30. doi:10.1002/jbmr.2176. PMID 24443324.