Clostridium perfringens: Difference between revisions
Shanshan Cen (talk | contribs) |
No edit summary |
||
| Line 1: | Line 1: | ||
{{Taxobox | {{Taxobox | ||
| image = Clostridium_perfringens.jpg | | image = Clostridium_perfringens.jpg | ||
| image_width = 240px | | image_width = 240px | ||
| image_caption = Photomicrograph of gram-positive ''Clostridium | | image_caption = Photomicrograph of gram-positive ''Clostridium perfringens'' bacilli. | ||
| regnum = [[ | | regnum = [[Bacteria]] | ||
| | | phylum = [[Firmicutes]] | ||
| classis = [[Clostridia]] | | classis = [[Clostridia]] | ||
| ordo = [[Clostridia]]les | | ordo = [[Clostridia]]les | ||
| Line 13: | Line 11: | ||
| species = '''''C. perfringens''''' | | species = '''''C. perfringens''''' | ||
| binomial = ''Clostridium perfringens'' | | binomial = ''Clostridium perfringens'' | ||
| binomial_authority = Veillon & Zuber 1898<br>Hauduroy ''et al.'' 1937 | | binomial_authority = Veillon & Zuber 1898<br />Hauduroy ''et al.'' 1937 | ||
}} | }} | ||
'''''Clostridium perfringens''''' (formerly known as ''C. welchii,'' or ''Bacillus welchii'') is a [[Gram-positive]], rod-shaped, [[anaerobic bacterium|anaerobic]], [[Endospore|spore-forming]] [[bacterium]] of the genus ''[[Clostridium]]''.<ref name=Sherris>{{cite book | author = Ryan KJ; Ray CG (editors) | title = Sherris Medical Microbiology | edition = 4th | publisher = McGraw Hill | year = 2004|isbn = 0-8385-8529-9 }}{{Page needed|date=April 2011}}</ref> ''C. perfringens'' is everpresent in nature and can be found as a normal component of decaying vegetation, [[Pelagic sediment|marine sediment]], the [[Gut flora|intestinal tract of humans]] and other [[vertebrate]]s, [[insect]]s, and [[soil]]. It has the shortest reported generation time of any organism at 6.3 minutes in [[thioglycollate broth|thioglycollate]] medium.<ref name=bionumbers>http://bionumbers.hms.harvard.edu//bionumber.aspx?id=105474&ver=1</ref> | |||
''C. perfringens'' is the third most common cause of [[food poisoning]] in the United Kingdom and the United States though it can sometimes be ingested and cause no harm. | |||
'' | Infections due to ''C. perfringens'' show evidence of tissue [[necrosis]], [[bacteremia]], [[emphysema]]tous [[cholecystitis]], and [[gas gangrene]], which is also known as clostridial [[myonecrosis]]. The toxin involved in [[gas gangrene]] is known as [[Clostridium perfringens alpha toxin|α-toxin]], which inserts into the plasma membrane of cells, producing gaps in the membrane that disrupt normal cellular function. ''C. perfringens'' can participate in polymicrobial [[anaerobic infection]]s. ''Clostridium perfringens ''is commonly encountered in [[infection]]s as a component of the normal [[flora (microbiology)|flora]]. In this case, its role in disease is minor. | ||
The action of ''C. perfringens'' on dead bodies is known to [[mortuary]] workers as [[tissue gas]] and can be halted only by [[embalming]]. | |||
The action of ''C. perfringens'' on dead bodies is known to mortuary workers as [[tissue gas]] and can | |||
==Food poisoning== | ==Food poisoning== | ||
In the United Kingdom and United States, ''C. perfringens'' bacteria are the third most common cause of foodborne illness, with poorly prepared meat and poultry, or food properly prepared but left to stand too long, the main culprits in harboring the bacterium.<ref name="O.T.M">{{cite book | author = Warrell | title = Oxford Textbook of Medicine | edition = 4th | publisher = Oxford University Press | year = 2003 | isbn = 0-19-262922-0 |display-authors=etal}}{{Page needed|date=April 2011}}</ref> The [[clostridium perfringens enterotoxin]] (CPE) mediating the disease is heat-labile (inactivated at {{convert|74|C|F}}). It can be detected in contaminated food (if not heated properly), and feces.<ref name=M.D.T>{{cite book | author = Murray | title = Medical Microbiology | edition = 6th | publisher = Mosby Elsevier | year = 2009 | isbn = 978-0-323-05470-6 |display-authors=etal}}{{Page needed|date=April 2011}}</ref> Incubation time is between six and 24 (commonly 10-12) hours after ingestion of contaminated food. | |||
Since ''C. perfringens'' forms spores that can withstand cooking temperatures, if cooked food is let stand for long enough, germination can ensue and infective bacterial colonies develop. Symptoms typically include abdominal cramping, diarrhea; vomiting and fever are usual. The whole course usually resolves within 24 hours. Very rare, fatal cases of [[clostridial necrotizing enteritis]] (also known as pigbel) have been known to involve "Type C" strains of the organism, which produce a potently ulcerative [[Clostridium perfringens beta toxin|β-toxin]]. This strain is most frequently encountered in [[Papua New Guinea]]. | |||
Many cases of ''C. perfringens'' food poisoning likely remain [[subclinical]], as [[antibody|antibodies]] to the toxin are common among the population. This has led to the conclusion that most of the population has experienced food poisoning due to ''C. perfringens''. | |||
== | Despite its potential dangers, ''C. perfringens'' is used as the [[leavening agent]] in [[salt rising bread]]. The baking process is thought to reduce the bacterial contamination, precluding negative effects.<ref>{{cite journal|last1=Juckett|first1=Gregory|last2=et al|title=The Microbiology of Salt Rising Bread|journal=West Virginia Medical Journal|date=November 2008|issue=22|url=http://mediad.publicbroadcasting.net/p/wvpn/files/201404/microbiologySRB.pdf|accessdate=22 July 2015}}</ref> | ||
== Infection == | |||
''Clostridium perfringens'' is the most common bacterial agent for [[gas gangrene]], which is necrosis, putrefaction of tissues, and gas production. It is caused primarily by [[Clostridium perfringens alpha toxin]]. The gases form bubbles in muscle (crepitus) and the characteristic smell in decomposing tissue. After rapid and destructive local spread (which can take only hours), systemic spread of bacteria and bacterial toxins may cause death. This is a problem in major trauma and in military contexts. ''C. perfringens'' grows readily on blood agar plate in anaerobic conditions, and often produces a double zone of beta hemolysis. | |||
== | Research published in 2014 suggested that a strain of ''C. perfringens'' might be implicated in [[multiple sclerosis]] (MS). Tests in [[Laboratory mouse|mice]] found that a toxin made by a rare strain of ''C. perfringens'' caused MS-like damage in the brain, and earlier work had identified this strain of ''C. perfringens'' in a human with MS.<ref>{{cite web | url=http://www.bbc.co.uk/news/health-25925658 | title=Multiple sclerosis 'linked to food bug' | publisher=BBC | date=29 January 2014 | accessdate=29 January 2014}}</ref> MS patients were found to be ten times more immune-reactive to the epsilon toxin than healthy people.<ref>http://www.foxnews.com/health/2014/01/29/bacterial-toxin-may-trigger-multiple-sclerosis-research-finds/?intcmp=trending</ref> | ||
== Diagnosis == | |||
''C. perfringens'' can be diagnosed by [[Nagler's reaction]] where the suspect organism is cultured on an egg yolk media plate. One side of the plate contains anti-alpha-toxin, while the other side does not. A streak of suspect organism is placed through both sides. An area of turbidity will form around the side that does not have the anti-alpha-toxin, indicating uninhibited [[lecithinase]] activity. | |||
Other tests/reactions: Catalase: Negative, Spot indole: Positive, Lecithinase: Positive, Lipase: Negative, Litmus Milk: Stormy Fermentation, Reverse CAMP plate: Positive, Gas Liquid Chromatography products: (Acetic, Butyric and Lactic Acids). | |||
== Treatment == | |||
If suspected on clinical grounds, treatment should begin without waiting for lab results. Traumatic wounds should be cleaned. Wounds that cannot be cleaned should not be stitched shut. Penicillin prophylaxis kills many clostridia and is thus useful for dirty wounds and lower leg amputations. A high infectious dose is required; the carrier state persists for several days. | |||
==Food poisoning incidents== | |||
On May 7, 2010, 42 residents and 12 staff members at a Louisiana state psychiatric hospital experienced vomiting, abdominal cramps, and diarrhea. Within 24 hours, three patients had died. The outbreak was linked to chicken which was cooked a day prior to being served and was not cooled down according to hospital guidelines. The outbreak affected 31% of the residents of the hospital and 69% of the staff who ate the chicken. It is unknown how many of the affected residents ate the chicken.<ref>{{cite web|title=Fatal Foodborne Clostridium perfringens Illness at a State Psychiatric Hospital — Louisiana, 2010|url=http://www.cdc.gov/mmwr/preview/mmwrhtml/mm6132a1.htm|work=Centers for Disease Control and Prevention|accessdate=16 November 2013}}</ref> | |||
In May 2011, a man died after allegedly eating food contaminated with the bacteria on a [[Transatlantic flight|transatlantic]] [[American Airlines]] flight. The man's wife and daughter are suing American and [[LSG Sky Chefs]], the German company that prepared the inflight food.<ref>{{cite web|last=Mohn |first=Tanya |url=http://overheadbin.msnbc.msn.com/_news/2011/12/01/9146822-passenger-dies-in-flight-family-says-airline-to-blame |title=Overhead Bin - Passenger dies in-flight, family says airline to blame |publisher=Overheadbin.msnbc.msn.com |date= |accessdate=2012-02-13}}</ref> | |||
In December 2012, a 46-year-old woman died two days after eating a Christmas Day meal at a pub in [[Hornchurch]], [[Essex]], [[England]]. She was among about 30 people to fall ill after eating the meal. Samples taken from the victims contained ''C.perfringens''. The hotel manager and the cook were jailed for offences arising from the incident.<ref>{{cite news|title=Pub chef and manager jailed over Christmas dinner that left a diner dead|url=http://www.theguardian.com/uk-news/2015/jan/23/pub-chef-manager-jailed-christmas-dinner-diner-dead|accessdate=3 August 2015|work=[[The Guardian]]|date=23 January 2015}}</ref> | |||
In December 2014, 87 year old Bessie Scott died three days after eating a church potluck supper in [[Nackawic]], [[New Brunswick]], [[Canada]]. Over 30 other people reported signs of gastrointestinal illness, diarrhea and abdominal pain. The province's acting chief medical officer says ''Clostridium perfringens'' is the bacteria that most likely caused the woman’s death.<ref>{{cite news|url=http://www.cbc.ca/news/canada/new-brunswick/woman-s-death-likely-caused-by-bacteria-from-christmas-supper-1.2870869|title=Woman's death likely caused by bacteria from Christmas supper|publisher=''[[Canadian Broadcasting Corporation|CBC]]''|date=12 December 2014}}</ref> | |||
==References== | ==References== | ||
{{ | {{reflist|2}} | ||
==External links== | ==External links== | ||
* [http://patricbrc.org/portal/portal/patric/Taxon?cType=taxon&cId=1502 Clostridium perfringens] genomes and related information at [http://patricbrc.org/ PATRIC], a Bioinformatics Resource Center funded by [http://www.niaid.nih.gov/ NIAID] | |||
* [http://pathema.jcvi.org/cgi-bin/Clostridium/PathemaHomePage.cgi Pathema-''Clostridium'' Resource] | |||
{{Gram-positive firmicutes diseases}} | |||
{{Toxins}} | |||
{{Consumer Food Safety}} | |||
{{Authority control}} | |||
{{DEFAULTSORT:Clostridium Perfringens}} | |||
[[Category:Clostridiaceae]] | [[Category:Clostridiaceae]] | ||
[[Category: | [[Category:Gas gangrene]] | ||
[[Category: | [[Category:Gram-positive bacteria]] | ||
[[Category:Bacteria with sequenced genomes]] | |||
[[ | |||
Revision as of 17:07, 6 August 2015
| style="background:#Template:Taxobox colour;"|Template:Taxobox name | ||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
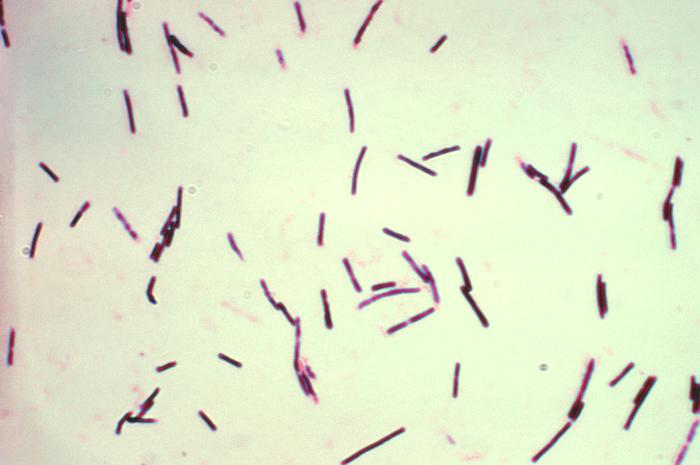 Photomicrograph of gram-positive Clostridium perfringens bacilli.
| ||||||||||||||
| style="background:#Template:Taxobox colour;" | Scientific classification | ||||||||||||||
| ||||||||||||||
| Binomial name | ||||||||||||||
| Clostridium perfringens Veillon & Zuber 1898 Hauduroy et al. 1937 |
Clostridium perfringens (formerly known as C. welchii, or Bacillus welchii) is a Gram-positive, rod-shaped, anaerobic, spore-forming bacterium of the genus Clostridium.[1] C. perfringens is everpresent in nature and can be found as a normal component of decaying vegetation, marine sediment, the intestinal tract of humans and other vertebrates, insects, and soil. It has the shortest reported generation time of any organism at 6.3 minutes in thioglycollate medium.[2]
C. perfringens is the third most common cause of food poisoning in the United Kingdom and the United States though it can sometimes be ingested and cause no harm.
Infections due to C. perfringens show evidence of tissue necrosis, bacteremia, emphysematous cholecystitis, and gas gangrene, which is also known as clostridial myonecrosis. The toxin involved in gas gangrene is known as α-toxin, which inserts into the plasma membrane of cells, producing gaps in the membrane that disrupt normal cellular function. C. perfringens can participate in polymicrobial anaerobic infections. Clostridium perfringens is commonly encountered in infections as a component of the normal flora. In this case, its role in disease is minor.
The action of C. perfringens on dead bodies is known to mortuary workers as tissue gas and can be halted only by embalming.
Food poisoning
In the United Kingdom and United States, C. perfringens bacteria are the third most common cause of foodborne illness, with poorly prepared meat and poultry, or food properly prepared but left to stand too long, the main culprits in harboring the bacterium.[3] The clostridium perfringens enterotoxin (CPE) mediating the disease is heat-labile (inactivated at 74 °C (165.2 °F)). It can be detected in contaminated food (if not heated properly), and feces.[4] Incubation time is between six and 24 (commonly 10-12) hours after ingestion of contaminated food.
Since C. perfringens forms spores that can withstand cooking temperatures, if cooked food is let stand for long enough, germination can ensue and infective bacterial colonies develop. Symptoms typically include abdominal cramping, diarrhea; vomiting and fever are usual. The whole course usually resolves within 24 hours. Very rare, fatal cases of clostridial necrotizing enteritis (also known as pigbel) have been known to involve "Type C" strains of the organism, which produce a potently ulcerative β-toxin. This strain is most frequently encountered in Papua New Guinea.
Many cases of C. perfringens food poisoning likely remain subclinical, as antibodies to the toxin are common among the population. This has led to the conclusion that most of the population has experienced food poisoning due to C. perfringens.
Despite its potential dangers, C. perfringens is used as the leavening agent in salt rising bread. The baking process is thought to reduce the bacterial contamination, precluding negative effects.[5]
Infection
Clostridium perfringens is the most common bacterial agent for gas gangrene, which is necrosis, putrefaction of tissues, and gas production. It is caused primarily by Clostridium perfringens alpha toxin. The gases form bubbles in muscle (crepitus) and the characteristic smell in decomposing tissue. After rapid and destructive local spread (which can take only hours), systemic spread of bacteria and bacterial toxins may cause death. This is a problem in major trauma and in military contexts. C. perfringens grows readily on blood agar plate in anaerobic conditions, and often produces a double zone of beta hemolysis.
Research published in 2014 suggested that a strain of C. perfringens might be implicated in multiple sclerosis (MS). Tests in mice found that a toxin made by a rare strain of C. perfringens caused MS-like damage in the brain, and earlier work had identified this strain of C. perfringens in a human with MS.[6] MS patients were found to be ten times more immune-reactive to the epsilon toxin than healthy people.[7]
Diagnosis
C. perfringens can be diagnosed by Nagler's reaction where the suspect organism is cultured on an egg yolk media plate. One side of the plate contains anti-alpha-toxin, while the other side does not. A streak of suspect organism is placed through both sides. An area of turbidity will form around the side that does not have the anti-alpha-toxin, indicating uninhibited lecithinase activity. Other tests/reactions: Catalase: Negative, Spot indole: Positive, Lecithinase: Positive, Lipase: Negative, Litmus Milk: Stormy Fermentation, Reverse CAMP plate: Positive, Gas Liquid Chromatography products: (Acetic, Butyric and Lactic Acids).
Treatment
If suspected on clinical grounds, treatment should begin without waiting for lab results. Traumatic wounds should be cleaned. Wounds that cannot be cleaned should not be stitched shut. Penicillin prophylaxis kills many clostridia and is thus useful for dirty wounds and lower leg amputations. A high infectious dose is required; the carrier state persists for several days.
Food poisoning incidents
On May 7, 2010, 42 residents and 12 staff members at a Louisiana state psychiatric hospital experienced vomiting, abdominal cramps, and diarrhea. Within 24 hours, three patients had died. The outbreak was linked to chicken which was cooked a day prior to being served and was not cooled down according to hospital guidelines. The outbreak affected 31% of the residents of the hospital and 69% of the staff who ate the chicken. It is unknown how many of the affected residents ate the chicken.[8]
In May 2011, a man died after allegedly eating food contaminated with the bacteria on a transatlantic American Airlines flight. The man's wife and daughter are suing American and LSG Sky Chefs, the German company that prepared the inflight food.[9]
In December 2012, a 46-year-old woman died two days after eating a Christmas Day meal at a pub in Hornchurch, Essex, England. She was among about 30 people to fall ill after eating the meal. Samples taken from the victims contained C.perfringens. The hotel manager and the cook were jailed for offences arising from the incident.[10]
In December 2014, 87 year old Bessie Scott died three days after eating a church potluck supper in Nackawic, New Brunswick, Canada. Over 30 other people reported signs of gastrointestinal illness, diarrhea and abdominal pain. The province's acting chief medical officer says Clostridium perfringens is the bacteria that most likely caused the woman’s death.[11]
References
- ↑ Ryan KJ; Ray CG (editors) (2004). Sherris Medical Microbiology (4th ed.). McGraw Hill. ISBN 0-8385-8529-9.[page needed]
- ↑ http://bionumbers.hms.harvard.edu//bionumber.aspx?id=105474&ver=1
- ↑ Warrell; et al. (2003). Oxford Textbook of Medicine (4th ed.). Oxford University Press. ISBN 0-19-262922-0.[page needed]
- ↑ Murray; et al. (2009). Medical Microbiology (6th ed.). Mosby Elsevier. ISBN 978-0-323-05470-6.[page needed]
- ↑ Juckett, Gregory; et al. (November 2008). "The Microbiology of Salt Rising Bread" (PDF). West Virginia Medical Journal (22). Retrieved 22 July 2015.
- ↑ "Multiple sclerosis 'linked to food bug'". BBC. 29 January 2014. Retrieved 29 January 2014.
- ↑ http://www.foxnews.com/health/2014/01/29/bacterial-toxin-may-trigger-multiple-sclerosis-research-finds/?intcmp=trending
- ↑ "Fatal Foodborne Clostridium perfringens Illness at a State Psychiatric Hospital — Louisiana, 2010". Centers for Disease Control and Prevention. Retrieved 16 November 2013.
- ↑ Mohn, Tanya. "Overhead Bin - Passenger dies in-flight, family says airline to blame". Overheadbin.msnbc.msn.com. Retrieved 2012-02-13.
- ↑ "Pub chef and manager jailed over Christmas dinner that left a diner dead". The Guardian. 23 January 2015. Retrieved 3 August 2015.
- ↑ "Woman's death likely caused by bacteria from Christmas supper". CBC. 12 December 2014.
External links
- Clostridium perfringens genomes and related information at PATRIC, a Bioinformatics Resource Center funded by NIAID
- Pathema-Clostridium Resource
Template:Gram-positive firmicutes diseases
Lua error in Module:Authority_control at line 788: attempt to index field 'wikibase' (a nil value).