Hematuria diagnostic evaluation: Difference between revisions
Adnan Ezici (talk | contribs) No edit summary |
|||
| (19 intermediate revisions by 3 users not shown) | |||
| Line 1: | Line 1: | ||
__NOTOC__ | __NOTOC__ | ||
{{ | {{Hematuria}} | ||
{{CMG}}; {{AE}} {{SCC}} {{Adnan Ezici}} {{VSKP}} | |||
== Overview == | == Overview == | ||
Specifically, among patients with [[Hematuria|gross hematuria]], 50% have been found to have a demonstrable cause, with 20% to 25% found to have a [[urologic]] malignancy, most commonly [[bladder cancer]] and [[Kidney cancer|kidney cance]]<nowiki/>r. Given the increased frequency with which clinically significant findings are associated with gross hematuria, the recommended evaluation in this setting is relatively uniform. That is, patients presenting with gross hematuria in the absence of antecedent trauma or culture-documented [[Urinary tract infection|UTI]] should be evaluated with a urine cytologic examination, [[cystoscopy]], and upper tract imaging, preferably CT urogram'''.''' <ref name="CohenBrown2003" /> | |||
== Diagnosis == | |||
Evaluation of patients with hematuria includes a focused history and physical examination, urinalysis, and various blood tests. Evaluation of hematuria is best performed in stepwise progression, beginning with simple and noninvasive investigations, followed by more aggressive interventions if positive results are obtained. Most importantly the [[Urinary tract|lower urinary tract]] should be visualized using [[cystoscopy]], usually using a flexible scope, and the upper tract imaged by a combination of modalities including plain [[X-ray]], [[ultrasonography]], intravenous urography or [[CT]] urography. | |||
The initial evaluation of patients presenting with gross hematuria is 3-fold:<ref name="pmid27261791">{{cite journal| author=Avellino GJ, Bose S, Wang DS| title=Diagnosis and Management of Hematuria. | journal=Surg Clin North Am | year= 2016 | volume= 96 | issue= 3 | pages= 503-15 | pmid=27261791 | doi=10.1016/j.suc.2016.02.007 | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=27261791 }}</ref> | The initial evaluation of patients presenting with gross hematuria is 3-fold:<ref name="pmid27261791">{{cite journal| author=Avellino GJ, Bose S, Wang DS| title=Diagnosis and Management of Hematuria. | journal=Surg Clin North Am | year= 2016 | volume= 96 | issue= 3 | pages= 503-15 | pmid=27261791 | doi=10.1016/j.suc.2016.02.007 | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=27261791 }}</ref> | ||
* Assess hemodynamic stability | * Assess hemodynamic stability | ||
* Determine the underlying cause of hematuria (same for gross hematuria/ microscopic hematuria/ asymptomatic hematuria).<ref name="Pan20062" /> | * Determine the underlying cause of hematuria (same for gross hematuria/ microscopic hematuria/ asymptomatic hematuria).<ref name="Pan20062" /> | ||
* Ensure urinary drainage. | * Ensure urinary drainage. | ||
===Urine-based tests=== | ===Urine-based tests=== | ||
Urinalysis is a simple and efficient tool to diagnose renal and urological diseases. | |||
====Dipstick test==== | ====Dipstick test==== | ||
A urine dipstick analysis is a highly sensitive measure for detection of blood, but it lacks specificity (sensitivity of 95% and a specificity of 75%). This translates into a large number of false positives, in which case, the urine dipstick is positive, but microscopy reveals fewer than 3RBC/HPF. This particular combination can be seen in the following benign or pathological circumstances:<ref name="AminZaritsky2011">{{cite journal|last1=Amin|first1=Nimisha|last2=Zaritsky|first2=Joshua J.|title=Hematuria|year=2011|pages=258–261|doi=10.1016/B978-0-323-05405-8.00069-3}}</ref> | A urine dipstick analysis is a highly sensitive measure for detection of blood, but it lacks [[Specificity (tests)|specificity]] (sensitivity of 95% and a specificity of 75%). This translates into a large number of false positives, in which case, the urine dipstick is positive, but microscopy reveals fewer than 3RBC/HPF. This particular combination can be seen in the following benign or pathological circumstances:<ref name="AminZaritsky2011">{{cite journal|last1=Amin|first1=Nimisha|last2=Zaritsky|first2=Joshua J.|title=Hematuria|year=2011|pages=258–261|doi=10.1016/B978-0-323-05405-8.00069-3}}</ref><ref name="IngelfingerLongo2021">{{cite journal|last1=Ingelfinger|first1=Julie R.|last2=Longo|first2=Dan L.|title=Hematuria in Adults|journal=New England Journal of Medicine|volume=385|issue=2|year=2021|pages=153–163|issn=0028-4793|doi=10.1056/NEJMra1604481}}</ref> | ||
#''Presence of certain substances in urine'': Sodium hypochlorite, peroxidases from vegetable or bacterial sources, and semen | |||
#''Ingestion of certain foods'': beets, blackberries, food coloring | #''Ingestion of certain foods'': beets, blackberries, food coloring | ||
#''Ingestion of certain medications'': [[Chloroquine]], [[Ibuprofen]], [[Iron]], [[Sorbitol]], [[Nitrofurantoin]], [[Phenazopyridine]], [[Urate|Urates]] or [[Rifampin]] (which often produces orange urine) | #''Ingestion of certain medications'': [[Chloroquine]], [[Ibuprofen]], [[Iron]], [[Sorbitol]], [[Nitrofurantoin]], [[Phenazopyridine]], [[Urate|Urates]] or [[Rifampin]] (which often produces orange urine) | ||
| Line 22: | Line 21: | ||
#''[[Urinary tract infection]]'': secondary to the action of [[Peroxidase|bacterial peroxidases]] on the dipstick | #''[[Urinary tract infection]]'': secondary to the action of [[Peroxidase|bacterial peroxidases]] on the dipstick | ||
#Delay in reading urine dipstick after submersion in urine | #Delay in reading urine dipstick after submersion in urine | ||
Given the large number of situations in which a positive dipstick may not represent true hematuria, all urine samples that test positive on dipstick analysis must be sent for microscopy to confirm hematuria. | Given the large number of situations in which a positive dipstick may not represent true hematuria, all urine samples that test positive on dipstick analysis must be sent for microscopy to confirm hematuria. | ||
====Microscopy and urine cytology ==== | ====Microscopy and urine cytology<ref name="Surgery (Oxford)">{{cite web |url=http://www.surgeryjournal.co.uk/article/S0263-9319(10)00199-7/abstract |title=www.surgeryjournal.co.uk |format= |work= |accessdate=}}</ref> ==== | ||
{| class="wikitable" | {| class="wikitable" | ||
| Line 34: | Line 32: | ||
'''Advantages''' | '''Advantages''' | ||
* Differentiate glomerular from nonglomerular sources of bleeding | |||
*Useful for detecting [[urinary casts]] (suggesting renal disease) | *Useful for detecting [[urinary casts]] (suggesting renal disease) | ||
*Useful for detecting urinary crystals (suggesting calculous disease) | *Useful for detecting urinary crystals (suggesting calculous disease) | ||
| Line 45: | Line 44: | ||
==== Positive Dipstick Test and Negitive Microscopic Results<ref name="pmid24364522">Sharp VJ, Barnes KT, Erickson BA (2013) [https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&retmode=ref&cmd=prlinks&id=24364522 Assessment of asymptomatic microscopic hematuria in adults.] ''Am Fam Physician'' 88 (11):747-54. PMID: [https://pubmed.gov/24364522 24364522]</ref> ==== | ==== Positive Dipstick Test and Negitive Microscopic Results<ref name="pmid24364522">Sharp VJ, Barnes KT, Erickson BA (2013) [https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&retmode=ref&cmd=prlinks&id=24364522 Assessment of asymptomatic microscopic hematuria in adults.] ''Am Fam Physician'' 88 (11):747-54. PMID: [https://pubmed.gov/24364522 24364522]</ref> ==== | ||
Patients who screen positive for hematuria with a urine dipstick test but have a negative follow-up | Patients who screen positive for hematuria with a urine dipstick test but have a negative follow-up [[Microscopic|microscopi]]<nowiki/>c examination should undergo three additional microscopic tests to rule out hematuria. If one of these repeat test results is positive on microscopic analysis, the patient is considered to have microscopic hematuria. If all three specimens are negative on microscopy, the patient does not require further evaluation for hematuria,6 and other causes of a positive dipstick test result, such as [[hemoglobinuria]] and [[myoglobinuria]], should be considered. | ||
==== Urine Culture ==== | ==== Urine Culture ==== | ||
If a patient has microscopic hematuria in the presence of [[pyuria]] or [[bacteriuria]], a urine culture should be obtained to rule out [[urinary tract infection]]. Culture-directed antibiotics should be administered, and a microscopic urinalysis should be repeated in six weeks to assess for resolution of the hematuria. If the hematuria has resolved after the infection has cleared, no further workup is needed. If hematuria persists, diagnostic evaluation should commence.<ref name="pmid24364522" /> | If a patient has microscopic hematuria in the presence of [[pyuria]] or [[bacteriuria]], a urine culture should be obtained to rule out [[urinary tract infection]]. Culture-directed [[antibiotics]] should be administered, and a microscopic [[urinalysis]] should be repeated in six weeks to assess for resolution of the hematuria. If the hematuria has resolved after the infection has cleared, no further workup is needed. If hematuria persists, diagnostic evaluation should commence.<ref name="pmid24364522" /> | ||
===Blood tests=== | ===Blood tests=== | ||
*Complete blood count (to detect anemia) | *Complete blood count (to detect anemia) | ||
*[[Coagulation studies]] (to detect [[hemoglobinopathies]]) | *[[Coagulation studies]] (to detect [[hemoglobinopathies]]) | ||
*Antibody studies (e.g. [[Antinuclear antibodies|ANA]], [[ANCA]], [[ASO]], anti- glomerular [[basement membrane]] antibodies (to detect [[glomerular]] cause of hematuria) | |||
*Complement levels (to detect [[Nephritic syndrome|nephritic]] cause of hematuria) | *Complement levels (to detect [[Nephritic syndrome|nephritic]] cause of hematuria) | ||
*Serum urea, creatinine and electrolytes (to detect renal impairment) | *Serum [[urea]], [[creatinine]] and electrolytes (to detect renal impairment) | ||
===Investigation of the lower urinary tract=== | ===Investigation of the lower urinary tract=== | ||
| Line 60: | Line 60: | ||
====Cytoscopy==== | ====Cytoscopy==== | ||
It is a key component of the hematuria evaluation because it is the most reliable way to evaluate the bladder for the presence of bladder cancer and provides the opportunity to evaluate the urethra. Cystoscopy should be performed in all adults who meet criteria for hematuria evaluation who are 35 years of age or older and/or have risk factors for malignancy. Flexible cystoscope is useful for the inspection of the urethra and visualization of the bladder mucosa. It is quick, well tolerated and safe procedure. The detection of an abnormality will require subsequent rigid cystoscopy under anesthesia, whereby tissue can be obtained or treatment performed.<ref name="Surgery (Oxford)" /> At the population level, bladder cancer is quite rare (<1 per 100,000) among persons 35 years old or younger, so cystoscopy may be omitted in persons younger than age 35 years without risk factors or clinical suspicion for bladder cancer or urethral pathology. The potential risks include discomfort, injury to the urethra, infection, and the need for additional procedures, such as biopsy.<ref name="Pan20062">{{cite journal|last1=Pan|first1=Cynthia G.|title=Evaluation of Gross Hematuria|journal=Pediatric Clinics of North America|volume=53|issue=3|year=2006|pages=401–412|issn=00313955|doi=10.1016/j.pcl.2006.03.002}}</ref> | It is a key component of the hematuria evaluation because it is the most reliable way to evaluate the [[bladder]] for the presence of [[bladder cancer]] and provides the opportunity to evaluate the [[urethra]]. Cystoscopy should be performed in all adults who meet criteria for hematuria evaluation who are 35 years of age or older and/or have risk factors for malignancy. Flexible [[cystoscope]] is useful for the inspection of the urethra and visualization of the bladder mucosa. It is quick, well tolerated and safe procedure. The detection of an abnormality will require subsequent rigid cystoscopy under anesthesia, whereby tissue can be obtained or treatment performed.<ref name="Surgery (Oxford)">{{cite web |url=http://www.surgeryjournal.co.uk/article/S0263-9319(10)00199-7/abstract |title=www.surgeryjournal.co.uk |format= |work= |accessdate=}}</ref> At the population level, bladder cancer is quite rare (<1 per 100,000) among persons 35 years old or younger, so cystoscopy may be omitted in persons younger than age 35 years without risk factors or clinical suspicion for bladder cancer or urethral pathology. The potential risks include discomfort, injury to the urethra, infection, and the need for additional procedures, such as biopsy.<ref name="Pan20062">{{cite journal|last1=Pan|first1=Cynthia G.|title=Evaluation of Gross Hematuria|journal=Pediatric Clinics of North America|volume=53|issue=3|year=2006|pages=401–412|issn=00313955|doi=10.1016/j.pcl.2006.03.002}}</ref> | ||
===Investigation of the upper urinary tract=== | ===Investigation of the upper urinary tract=== | ||
Evaluation of the upper urinary tract | Evaluation of the [[Urinary tract|upper urinary tract i]]<nowiki/>s more complex, and requires a balance between the low detection rate of pathology and the number or extent of tests required to visualize the urinary organs. No single imaging modality has the desired attributes of a high [[Sensitivity (tests)|sensitivity]] and specificity, safety (low radiation exposure), low cost and applicability to lots of patients.<ref name="Surgery (Oxford)">{{cite web |url=http://www.surgeryjournal.co.uk/article/S0263-9319(10)00199-7/abstract |title=www.surgeryjournal.co.uk |format= |work= |accessdate=}}</ref> | ||
{| class="wikitable" | {| class="wikitable" | ||
|- | |- | ||
| Line 104: | Line 104: | ||
* Contraindicated in patients with specific conditions.( e.g. [[Pacemaker]], Significant renal function compromise (i.e., estimated [[Glomerular filtration rate|GFR]] <30) when the administration of gadolinium risks [[nephrogenic systemic fibrosis]]) | * Contraindicated in patients with specific conditions.( e.g. [[Pacemaker]], Significant renal function compromise (i.e., estimated [[Glomerular filtration rate|GFR]] <30) when the administration of gadolinium risks [[nephrogenic systemic fibrosis]]) | ||
|} | |} | ||
The '''gold standard''' investigation protocol for upper urinary tract would combine USS and IVU to evaluate the upper urinary tract. However, an IVU has a large radiation dosage with a small risk of reaction to contrast medium and detects upper tract UCC which are rare (less than 1% of all tumors presenting with hematuria). If looking for stone disease USS and a plain radiograph of the abdomen is recommended and IVU is reserved for equivocal cases, patients with persistent hematuria or patients with a high risk of UCC (elderly, smokers, occupational exposure). | The '''[[Gold standard (test)|gold standard]]''' investigation protocol for upper urinary tract would combine USS and IVU to evaluate the upper urinary tract. However, an IVU has a large radiation dosage with a small risk of reaction to contrast medium and detects upper tract UCC which are rare (less than 1% of all tumors presenting with hematuria). If looking for stone disease USS and a plain radiograph of the [[abdomen]] is recommended and IVU is reserved for equivocal cases, patients with persistent hematuria or patients with a high risk of UCC (elderly, smokers, occupational exposure). | ||
===Investigation of the glomerular cause of hematuria=== | ===Investigation of the glomerular cause of hematuria=== | ||
*24-hours urine collection should also be obtained to assess kidney function (e.g. [[Creatinine clearance|Creatinine clearance/glomerular filtration rate]], [[urine osmolality]], sodium and albumin concentrations). | *24-hours urine collection should also be obtained to assess kidney function (e.g. [[Creatinine clearance|Creatinine clearance/glomerular filtration rate]], [[urine osmolality]], [[sodium]] and [[albumin]] concentrations). | ||
*Renal biopsy | *Renal [[biopsy]] | ||
Evaluation of patients with haematuria includes a focussed history and physical examination, urinalysis and various blood tests.Most importantly the lower urinary tract should be visualized using cystoscopy, usually using a flexible scope, and the upper tract imaged by a combination of modalities including plain X-ray, ultrasonography, intravenous urography or computed tomography urography. | Evaluation of patients with haematuria includes a focussed history and physical examination, [[urinalysis]] and various blood tests.Most importantly the lower urinary tract should be visualized using cystoscopy, usually using a flexible scope, and the upper tract imaged by a combination of modalities including plain [[X-ray]], [[ultrasonography]], intravenous urography or [[computed tomography]] urography. | ||
The treatment options for haematuria depend on the underlying cause. | The treatment options for haematuria depend on the underlying cause. | ||
=== Algorithm for the Evaluation of Microscopic Hematuria <ref name="pmid24364522">Sharp VJ, Barnes KT, Erickson BA (2013) [https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&retmode=ref&cmd=prlinks&id=24364522 Assessment of asymptomatic microscopic hematuria in adults.] ''Am Fam Physician'' 88 (11):747-54. PMID: [https://pubmed.gov/24364522 24364522]</ref><ref name="CohenBrown2003">{{cite journal|last1=Cohen|first1=Robert A.|last2=Brown|first2=Robert S.|title=Microscopic Hematuria|journal=New England Journal of Medicine|volume=348|issue=23|year=2003|pages=2330–2338|issn=0028-4793|doi=10.1056/NEJMcp012694}}</ref> === | === Algorithm for the Evaluation of Microscopic Hematuria <ref name="pmid24364522">Sharp VJ, Barnes KT, Erickson BA (2013) [https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&retmode=ref&cmd=prlinks&id=24364522 Assessment of asymptomatic microscopic hematuria in adults.] ''Am Fam Physician'' 88 (11):747-54. PMID: [https://pubmed.gov/24364522 24364522]</ref><ref name="CohenBrown2003">{{cite journal|last1=Cohen|first1=Robert A.|last2=Brown|first2=Robert S.|title=Microscopic Hematuria|journal=New England Journal of Medicine|volume=348|issue=23|year=2003|pages=2330–2338|issn=0028-4793|doi=10.1056/NEJMcp012694}}</ref> === | ||
[[Image:Evaluation of Microscopic Hematuria Algorithm.jpg]] | <figure-inline class="mw-default-size"><figure-inline><figure-inline><figure-inline>[[Image:Evaluation of Microscopic Hematuria Algorithm.jpg|1223x1223px]]</figure-inline></figure-inline></figure-inline></figure-inline> | ||
== Hematuria ' One-Stop ' Clinic == | == Hematuria ' One-Stop ' Clinic == | ||
In recent years the ‘one-stop’ hematuria clinic has become popular for the investigation of hematuria as this enables synchronous urological and | In recent years the ‘one-stop’ hematuria clinic has become popular for the investigation of hematuria as this enables synchronous [[urological]] and [[Radiological|radiologica]]<nowiki/>l evaluation of the patient, resulting in rapid diagnosis and treatment.This clinic has been set up to save you having repeated visits to the hospital. For most patients, in the course of one visit, all the tests needed to diagnose the cause of the blood in the urine will be undertaken. Occasionally some further tests will be necessary as a result of the findings at the first visit. In the morning you will have either an [[x-ray]] or a scan (KUB or Ultrasound) depending on the type of bleeding you have experienced. Early in the afternoon you will be seen by the consultant urologist or one of his team. You will then be examined and finally an internal inspection of your bladder will be performed. By the end of your visit you should know the outcome of all your tests and whether anything further needs to be done.<ref name="pmid22085132">Ooi WL, Lee F, Wallace DM, Hayne D (2011) [https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&retmode=ref&cmd=prlinks&id=22085132 'One stop' haematuria clinic in Fremantle Hospital, Western Australia: a report of the first 500 patients.] ''BJU Int'' 108 Suppl 2 ():62-6. [http://dx.doi.org/10.1111/j.1464-410X.2011.10711.x DOI:10.1111/j.1464-410X.2011.10711.x] PMID: [https://pubmed.gov/22085132 22085132]</ref> | ||
== References == | == References == | ||
<references /> | |||
Latest revision as of 13:52, 27 July 2021
|
Hematuria Microchapters |
|
Diagnosis |
|---|
|
Treatment |
|
Case Studies |
|
Hematuria diagnostic evaluation On the Web |
|
American Roentgen Ray Society Images of Hematuria diagnostic evaluation |
|
Risk calculators and risk factors for Hematuria diagnostic evaluation |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]; Associate Editor(s)-in-Chief: Steven C. Campbell, M.D., Ph.D. Adnan Ezici, M.D[2] Venkata Sivakrishna Kumar Pulivarthi M.B.B.S [3]
Overview
Specifically, among patients with gross hematuria, 50% have been found to have a demonstrable cause, with 20% to 25% found to have a urologic malignancy, most commonly bladder cancer and kidney cancer. Given the increased frequency with which clinically significant findings are associated with gross hematuria, the recommended evaluation in this setting is relatively uniform. That is, patients presenting with gross hematuria in the absence of antecedent trauma or culture-documented UTI should be evaluated with a urine cytologic examination, cystoscopy, and upper tract imaging, preferably CT urogram. [1]
Diagnosis
Evaluation of patients with hematuria includes a focused history and physical examination, urinalysis, and various blood tests. Evaluation of hematuria is best performed in stepwise progression, beginning with simple and noninvasive investigations, followed by more aggressive interventions if positive results are obtained. Most importantly the lower urinary tract should be visualized using cystoscopy, usually using a flexible scope, and the upper tract imaged by a combination of modalities including plain X-ray, ultrasonography, intravenous urography or CT urography. The initial evaluation of patients presenting with gross hematuria is 3-fold:[2]
- Assess hemodynamic stability
- Determine the underlying cause of hematuria (same for gross hematuria/ microscopic hematuria/ asymptomatic hematuria).[3]
- Ensure urinary drainage.
Urine-based tests
Urinalysis is a simple and efficient tool to diagnose renal and urological diseases.
Dipstick test
A urine dipstick analysis is a highly sensitive measure for detection of blood, but it lacks specificity (sensitivity of 95% and a specificity of 75%). This translates into a large number of false positives, in which case, the urine dipstick is positive, but microscopy reveals fewer than 3RBC/HPF. This particular combination can be seen in the following benign or pathological circumstances:[4][5]
- Presence of certain substances in urine: Sodium hypochlorite, peroxidases from vegetable or bacterial sources, and semen
- Ingestion of certain foods: beets, blackberries, food coloring
- Ingestion of certain medications: Chloroquine, Ibuprofen, Iron, Sorbitol, Nitrofurantoin, Phenazopyridine, Urates or Rifampin (which often produces orange urine)
- Hemoglobinuria: often in the setting of hemolytic anemia
- Myoglobinuria: related to muscle damage (rhabdomyolysis), often after vigorous exercise or trauma
- Urinary tract infection: secondary to the action of bacterial peroxidases on the dipstick
- Delay in reading urine dipstick after submersion in urine
Given the large number of situations in which a positive dipstick may not represent true hematuria, all urine samples that test positive on dipstick analysis must be sent for microscopy to confirm hematuria.
Microscopy and urine cytology[6]
| Microscopy | Urine cytology |
|---|---|
| Microscopy is performed on urinary sediment (following centrifuging a fresh urine sample) and can quantify the number of erythrocytes.
Advantages
|
Urine cytology is the ‘gold standard’ urine-based test for detecting cancer.
Advantages
|
Positive Dipstick Test and Negitive Microscopic Results[7]
Patients who screen positive for hematuria with a urine dipstick test but have a negative follow-up microscopic examination should undergo three additional microscopic tests to rule out hematuria. If one of these repeat test results is positive on microscopic analysis, the patient is considered to have microscopic hematuria. If all three specimens are negative on microscopy, the patient does not require further evaluation for hematuria,6 and other causes of a positive dipstick test result, such as hemoglobinuria and myoglobinuria, should be considered.
Urine Culture
If a patient has microscopic hematuria in the presence of pyuria or bacteriuria, a urine culture should be obtained to rule out urinary tract infection. Culture-directed antibiotics should be administered, and a microscopic urinalysis should be repeated in six weeks to assess for resolution of the hematuria. If the hematuria has resolved after the infection has cleared, no further workup is needed. If hematuria persists, diagnostic evaluation should commence.[7]
Blood tests
- Complete blood count (to detect anemia)
- Coagulation studies (to detect hemoglobinopathies)
- Antibody studies (e.g. ANA, ANCA, ASO, anti- glomerular basement membrane antibodies (to detect glomerular cause of hematuria)
- Complement levels (to detect nephritic cause of hematuria)
- Serum urea, creatinine and electrolytes (to detect renal impairment)
Investigation of the lower urinary tract
Cytoscopy
It is a key component of the hematuria evaluation because it is the most reliable way to evaluate the bladder for the presence of bladder cancer and provides the opportunity to evaluate the urethra. Cystoscopy should be performed in all adults who meet criteria for hematuria evaluation who are 35 years of age or older and/or have risk factors for malignancy. Flexible cystoscope is useful for the inspection of the urethra and visualization of the bladder mucosa. It is quick, well tolerated and safe procedure. The detection of an abnormality will require subsequent rigid cystoscopy under anesthesia, whereby tissue can be obtained or treatment performed.[6] At the population level, bladder cancer is quite rare (<1 per 100,000) among persons 35 years old or younger, so cystoscopy may be omitted in persons younger than age 35 years without risk factors or clinical suspicion for bladder cancer or urethral pathology. The potential risks include discomfort, injury to the urethra, infection, and the need for additional procedures, such as biopsy.[3]
Investigation of the upper urinary tract
Evaluation of the upper urinary tract is more complex, and requires a balance between the low detection rate of pathology and the number or extent of tests required to visualize the urinary organs. No single imaging modality has the desired attributes of a high sensitivity and specificity, safety (low radiation exposure), low cost and applicability to lots of patients.[6]
| Ultrasound (US) | Intravenous urography (IVU) | Computed tomography (CT) | Endoscopy/Fluoroscopy | MRI |
|---|---|---|---|---|
Advantages
Disadvantages
|
Advantages
Disadvantages
|
Advantages
Disadvantages
|
Advantages
Disadvantages
|
Advantages
Disadvantages
|
The gold standard investigation protocol for upper urinary tract would combine USS and IVU to evaluate the upper urinary tract. However, an IVU has a large radiation dosage with a small risk of reaction to contrast medium and detects upper tract UCC which are rare (less than 1% of all tumors presenting with hematuria). If looking for stone disease USS and a plain radiograph of the abdomen is recommended and IVU is reserved for equivocal cases, patients with persistent hematuria or patients with a high risk of UCC (elderly, smokers, occupational exposure).
Investigation of the glomerular cause of hematuria
- 24-hours urine collection should also be obtained to assess kidney function (e.g. Creatinine clearance/glomerular filtration rate, urine osmolality, sodium and albumin concentrations).
- Renal biopsy
Evaluation of patients with haematuria includes a focussed history and physical examination, urinalysis and various blood tests.Most importantly the lower urinary tract should be visualized using cystoscopy, usually using a flexible scope, and the upper tract imaged by a combination of modalities including plain X-ray, ultrasonography, intravenous urography or computed tomography urography.
The treatment options for haematuria depend on the underlying cause.
Algorithm for the Evaluation of Microscopic Hematuria [7][1]
<figure-inline class="mw-default-size"><figure-inline><figure-inline><figure-inline>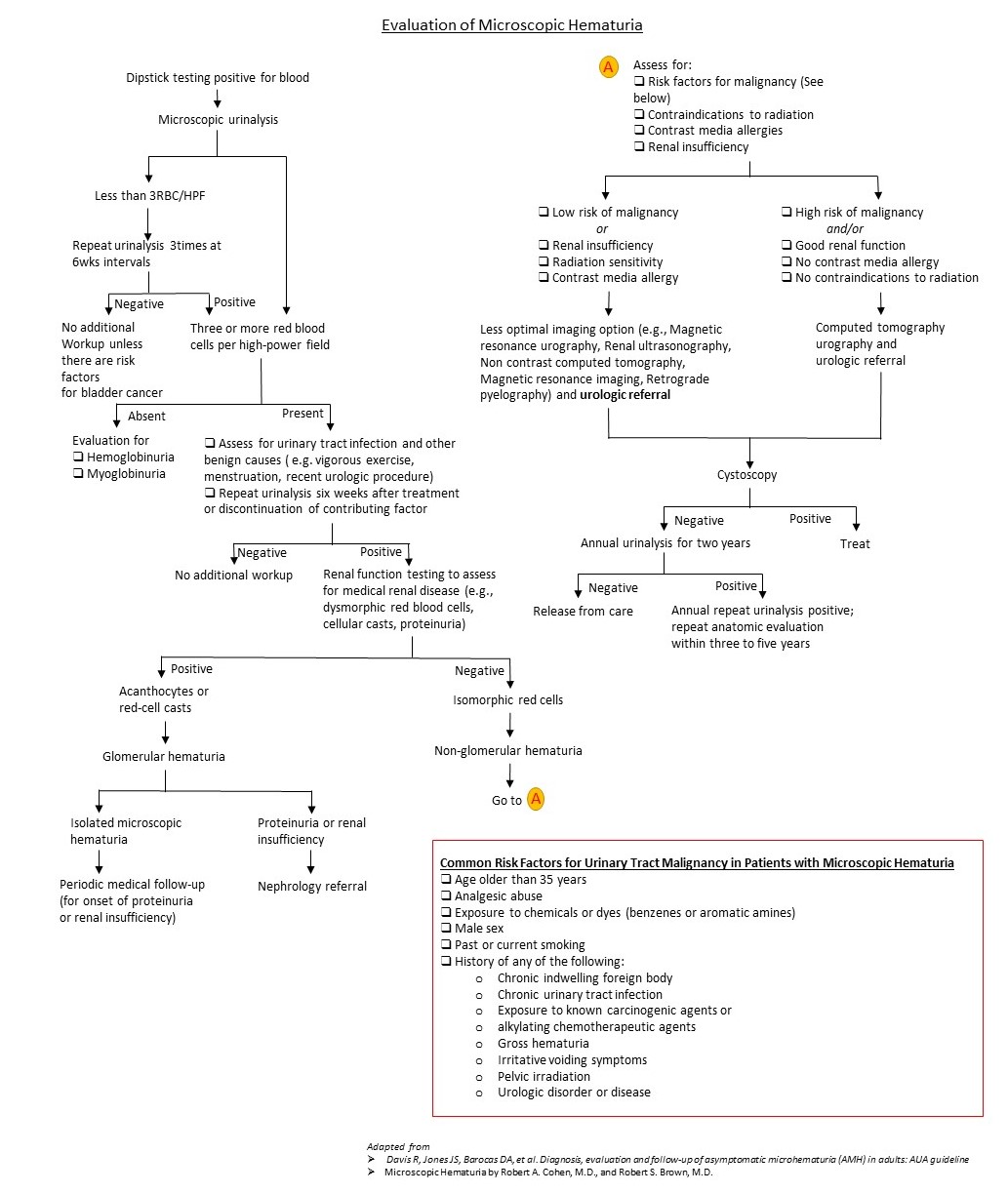 </figure-inline></figure-inline></figure-inline></figure-inline>
</figure-inline></figure-inline></figure-inline></figure-inline>
Hematuria ' One-Stop ' Clinic
In recent years the ‘one-stop’ hematuria clinic has become popular for the investigation of hematuria as this enables synchronous urological and radiological evaluation of the patient, resulting in rapid diagnosis and treatment.This clinic has been set up to save you having repeated visits to the hospital. For most patients, in the course of one visit, all the tests needed to diagnose the cause of the blood in the urine will be undertaken. Occasionally some further tests will be necessary as a result of the findings at the first visit. In the morning you will have either an x-ray or a scan (KUB or Ultrasound) depending on the type of bleeding you have experienced. Early in the afternoon you will be seen by the consultant urologist or one of his team. You will then be examined and finally an internal inspection of your bladder will be performed. By the end of your visit you should know the outcome of all your tests and whether anything further needs to be done.[8]
References
- ↑ 1.0 1.1 Cohen, Robert A.; Brown, Robert S. (2003). "Microscopic Hematuria". New England Journal of Medicine. 348 (23): 2330–2338. doi:10.1056/NEJMcp012694. ISSN 0028-4793.
- ↑ Avellino GJ, Bose S, Wang DS (2016). "Diagnosis and Management of Hematuria". Surg Clin North Am. 96 (3): 503–15. doi:10.1016/j.suc.2016.02.007. PMID 27261791.
- ↑ 3.0 3.1 Pan, Cynthia G. (2006). "Evaluation of Gross Hematuria". Pediatric Clinics of North America. 53 (3): 401–412. doi:10.1016/j.pcl.2006.03.002. ISSN 0031-3955.
- ↑ Amin, Nimisha; Zaritsky, Joshua J. (2011). "Hematuria": 258–261. doi:10.1016/B978-0-323-05405-8.00069-3.
- ↑ Ingelfinger, Julie R.; Longo, Dan L. (2021). "Hematuria in Adults". New England Journal of Medicine. 385 (2): 153–163. doi:10.1056/NEJMra1604481. ISSN 0028-4793.
- ↑ 6.0 6.1 6.2 "www.surgeryjournal.co.uk".
- ↑ 7.0 7.1 7.2 Sharp VJ, Barnes KT, Erickson BA (2013) Assessment of asymptomatic microscopic hematuria in adults. Am Fam Physician 88 (11):747-54. PMID: 24364522
- ↑ Ooi WL, Lee F, Wallace DM, Hayne D (2011) 'One stop' haematuria clinic in Fremantle Hospital, Western Australia: a report of the first 500 patients. BJU Int 108 Suppl 2 ():62-6. DOI:10.1111/j.1464-410X.2011.10711.x PMID: 22085132