|
|
| (164 intermediate revisions by 3 users not shown) |
| Line 1: |
Line 1: |
| ===Lab findings=== | | ==Physical examination== |
| | ==References== |
| | {{reflist|2}} |
|
| |
|
| '''Diagnosis of Cirrhosis'''
| | {{WH}} |
| | {{WS}} |
|
| |
|
| '''Laboratory findings''' —
| | ==References== |
| | | {{Reflist|2}} |
| Laboratory abnormalities may be the first indication of cirrhosis.
| |
| | |
| Common abnormalities include:<ref name="pmid22656328">{{cite journal |vauthors=Chalasani N, Younossi Z, Lavine JE, Diehl AM, Brunt EM, Cusi K, Charlton M, Sanyal AJ |title=The diagnosis and management of non-alcoholic fatty liver disease: practice guideline by the American Gastroenterological Association, American Association for the Study of Liver Diseases, and American College of Gastroenterology |journal=Gastroenterology |volume=142 |issue=7 |pages=1592–609 |year=2012 |pmid=22656328 |doi=10.1053/j.gastro.2012.04.001 |url=}}</ref><ref name="pmid22357834">{{cite journal |vauthors=Udell JA, Wang CS, Tinmouth J, FitzGerald JM, Ayas NT, Simel DL, Schulzer M, Mak E, Yoshida EM |title=Does this patient with liver disease have cirrhosis? |journal=JAMA |volume=307 |issue=8 |pages=832–42 |year=2012 |pmid=22357834 |doi=10.1001/jama.2012.186 |url=}}</ref>
| |
| * Increased serum bilirubin levels <ref name="pmid10498635">{{cite journal |vauthors=Krzeski P, Zych W, Kraszewska E, Milewski B, Butruk E, Habior A |title=Is serum bilirubin concentration the only valid prognostic marker in primary biliary cirrhosis? |journal=Hepatology |volume=30 |issue=4 |pages=865–9 |year=1999 |pmid=10498635 |doi=10.1002/hep.510300415 |url=}}</ref>
| |
| * Abnormal aminotransferase levels <ref name="pmid10781624">{{cite journal |vauthors=Pratt DS, Kaplan MM |title=Evaluation of abnormal liver-enzyme results in asymptomatic patients |journal=N. Engl. J. Med. |volume=342 |issue=17 |pages=1266–71 |year=2000 |pmid=10781624 |doi=10.1056/NEJM200004273421707 |url=}}</ref><ref name="pmid27995906">{{cite journal |vauthors=Kwo PY, Cohen SM, Lim JK |title=ACG Clinical Guideline: Evaluation of Abnormal Liver Chemistries |journal=Am. J. Gastroenterol. |volume=112 |issue=1 |pages=18–35 |year=2017 |pmid=27995906 |doi=10.1038/ajg.2016.517 |url=}}</ref><ref name="pmid20060831">{{cite journal |vauthors=Ruhl CE, Everhart JE |title=Trunk fat is associated with increased serum levels of alanine aminotransferase in the United States |journal=Gastroenterology |volume=138 |issue=4 |pages=1346–56, 1356.e1–3 |year=2010 |pmid=20060831 |pmc=2847039 |doi=10.1053/j.gastro.2009.12.053 |url=}}</ref><ref name="pmid12093239">{{cite journal |vauthors=Prati D, Taioli E, Zanella A, Della Torre E, Butelli S, Del Vecchio E, Vianello L, Zanuso F, Mozzi F, Milani S, Conte D, Colombo M, Sirchia G |title=Updated definitions of healthy ranges for serum alanine aminotransferase levels |journal=Ann. Intern. Med. |volume=137 |issue=1 |pages=1–10 |year=2002 |pmid=12093239 |doi= |url=}}</ref><ref name="pmid9581673">{{cite journal |vauthors=Piton A, Poynard T, Imbert-Bismut F, Khalil L, Delattre J, Pelissier E, Sansonetti N, Opolon P |title=Factors associated with serum alanine transaminase activity in healthy subjects: consequences for the definition of normal values, for selection of blood donors, and for patients with chronic hepatitis C. MULTIVIRC Group |journal=Hepatology |volume=27 |issue=5 |pages=1213–9 |year=1998 |pmid=9581673 |doi=10.1002/hep.510270505 |url=}}</ref><ref name="pmid12093245">{{cite journal |vauthors=Kaplan MM |title=Alanine aminotransferase levels: what's normal? |journal=Ann. Intern. Med. |volume=137 |issue=1 |pages=49–51 |year=2002 |pmid=12093245 |doi= |url=}}</ref><ref name="pmid15983331">{{cite journal |vauthors=Nannipieri M, Gonzales C, Baldi S, Posadas R, Williams K, Haffner SM, Stern MP, Ferrannini E |title=Liver enzymes, the metabolic syndrome, and incident diabetes: the Mexico City diabetes study |journal=Diabetes Care |volume=28 |issue=7 |pages=1757–62 |year=2005 |pmid=15983331 |doi= |url=}}</ref><ref name="pmid22764020">{{cite journal |vauthors=Liangpunsakul S, Chalasani N |title=What should we recommend to our patients with NAFLD regarding alcohol use? |journal=Am. J. Gastroenterol. |volume=107 |issue=7 |pages=976–8 |year=2012 |pmid=22764020 |pmc=3766378 |doi=10.1038/ajg.2012.20 |url=}}</ref><ref name="pmid520102">{{cite journal |vauthors=Cohen JA, Kaplan MM |title=The SGOT/SGPT ratio--an indicator of alcoholic liver disease |journal=Dig. Dis. Sci. |volume=24 |issue=11 |pages=835–8 |year=1979 |pmid=520102 |doi= |url=}}</ref>
| |
| * Elevated alkaline phosphatase / gamma-glutamyl transpeptidase <ref name="pmid11853185">{{cite journal |vauthors=Cabrera-Abreu JC, Green A |title=Gamma-glutamyltransferase: value of its measurement in paediatrics |journal=Ann. Clin. Biochem. |volume=39 |issue=Pt 1 |pages=22–5 |year=2002 |pmid=11853185 |doi=10.1258/0004563021901685 |url=}}</ref><ref name="pmid27995906">{{cite journal |vauthors=Kwo PY, Cohen SM, Lim JK |title=ACG Clinical Guideline: Evaluation of Abnormal Liver Chemistries |journal=Am. J. Gastroenterol. |volume=112 |issue=1 |pages=18–35 |year=2017 |pmid=27995906 |doi=10.1038/ajg.2016.517 |url=}}</ref><ref name="pmid2857631">{{cite journal |vauthors=Moussavian SN, Becker RC, Piepmeyer JL, Mezey E, Bozian RC |title=Serum gamma-glutamyl transpeptidase and chronic alcoholism. Influence of alcohol ingestion and liver disease |journal=Dig. Dis. Sci. |volume=30 |issue=3 |pages=211–4 |year=1985 |pmid=2857631 |doi= |url=}}</ref>
| |
| * Prolonged prothrombin time
| |
| * Elevated international normalized ratio (INR)
| |
| * Hyponatremia
| |
| * Thrombocytopenia
| |
| '''Liver function tests'''
| |
| * Aminotransferases :<ref name="pmid9448172">{{cite journal |vauthors=Sheth SG, Flamm SL, Gordon FD, Chopra S |title=AST/ALT ratio predicts cirrhosis in patients with chronic hepatitis C virus infection |journal=Am. J. Gastroenterol. |volume=93 |issue=1 |pages=44–8 |year=1998 |pmid=9448172 |doi=10.1111/j.1572-0241.1998.044_c.x |url=}}</ref><ref name="pmid3135226">{{cite journal |vauthors=Williams AL, Hoofnagle JH |title=Ratio of serum aspartate to alanine aminotransferase in chronic hepatitis. Relationship to cirrhosis |journal=Gastroenterology |volume=95 |issue=3 |pages=734–9 |year=1988 |pmid=3135226 |doi= |url=}}</ref>
| |
| * Aspartate aminotransferase (AST) and alanine aminotransferase (ALT) are usually moderately elevated
| |
| * AST is more often elevated than ALT
| |
| * Levels may be normal
| |
| | |
| * Alkaline phosphatase: <ref name="pmid696683">{{cite journal |vauthors=Ellis G, Goldberg DM, Spooner RJ, Ward AM |title=Serum enzyme tests in diseases of the liver and biliary tree |journal=Am. J. Clin. Pathol. |volume=70 |issue=2 |pages=248–58 |year=1978 |pmid=696683 |doi= |url=}}</ref>
| |
| | |
| * Alkaline phosphatase is usually elevated
| |
| | |
| * High levels may be seen in patients with underlying cholestatic liver disease such as:
| |
| ** Primary sclerosing cholangitis
| |
| ** Primary biliary cirrhosis
| |
| | |
| * Gamma-glutamyl transpeptidase: <ref name="pmid696683">{{cite journal |vauthors=Ellis G, Goldberg DM, Spooner RJ, Ward AM |title=Serum enzyme tests in diseases of the liver and biliary tree |journal=Am. J. Clin. Pathol. |volume=70 |issue=2 |pages=248–58 |year=1978 |pmid=696683 |doi= |url=}}</ref><ref name="pmid6104563">{{cite journal |vauthors=Goldberg DM |title=Structural, functional, and clinical aspects of gamma-glutamyltransferase |journal=CRC Crit Rev Clin Lab Sci |volume=12 |issue=1 |pages=1–58 |year=1980 |pmid=6104563 |doi= |url=}}</ref><ref name="pmid6132864">{{cite journal |vauthors=Barouki R, Chobert MN, Finidori J, Aggerbeck M, Nalpas B, Hanoune J |title=Ethanol effects in a rat hepatoma cell line: induction of gamma-glutamyltransferase |journal=Hepatology |volume=3 |issue=3 |pages=323–9 |year=1983 |pmid=6132864 |doi= |url=}}</ref>
| |
| ** Non specific
| |
| ** Correlates with ALP levels
| |
| | |
| * Higher in CLD due to alcohol use:
| |
| ** Alcohol causes GGT release from hepatocytes
| |
| ** Alcohol induces microsomal GGT in liver
| |
| | |
| * Bilirubin: Bilirubin levels may be normal or raised
| |
| | |
| * Albumin: Albumin levels reflect synthetic function of the liver
| |
| * Serum albumin levels helps grade the severity of cirrhosis
| |
| * Hypoalbuminemia is non specific for liver disease: heart failure, nephrotic syndrome, protein losing enteropathy, or malnutrition.
| |
| | |
| * Prothrombin time – Prothrombin time reflects the degree of hepatic synthetic function.
| |
| * Worsening coagulopathy correlates with the severity of hepatic dysfunction.
| |
| '''Serum chemistries''' :
| |
| * Hyponatremia is common in patients with cirrhosis and ascites and is related to an inability to excrete free water. <ref name="pmid2217672">{{cite journal |vauthors=Papadakis MA, Fraser CL, Arieff AI |title=Hyponatraemia in patients with cirrhosis |journal=Q. J. Med. |volume=76 |issue=279 |pages=675–88 |year=1990 |pmid=2217672 |doi= |url=}}</ref>
| |
| ** Due to ADH elevation
| |
| ** Reflects poor prognosis
| |
| | |
| * Progressive rise in serum creatinine: hepatorenal syndrome
| |
| '''Hematologic abnormalities:''' <ref name="pmid19281860">{{cite journal |vauthors=Qamar AA, Grace ND, Groszmann RJ, Garcia-Tsao G, Bosch J, Burroughs AK, Ripoll C, Maurer R, Planas R, Escorsell A, Garcia-Pagan JC, Patch D, Matloff DS, Makuch R, Rendon G |title=Incidence, prevalence, and clinical significance of abnormal hematologic indices in compensated cirrhosis |journal=Clin. Gastroenterol. Hepatol. |volume=7 |issue=6 |pages=689–95 |year=2009 |pmid=19281860 |pmc=4545534 |doi=10.1016/j.cgh.2009.02.021 |url=}}</ref>
| |
| * Thrombocytopenia: most common
| |
| * Mechanism of thrombocytopenia:
| |
| ** caused by portal hypertension with congestive splenomegaly: sequesters circulating platelets
| |
| ** decreased thrombopoietin levels
| |
| | |
| * Leukopenia/neutropenia: due to hypersplenism with splenic margination.
| |
| * Anemia
| |
| ** Mechanism of anemia:
| |
| ** Acute and chronic gastrointestinal blood loss
| |
| ** Folate deficiency
| |
| ** Direct toxicity due to alcohol
| |
| ** Hypersplenism
| |
| ** Bone marrow suppression ( hepatitis-associated aplastic anemia)
| |
| ** Anemia of chronic disease (inflammation)
| |
| ** Hemolysis
| |
| | |
| * '''Other abnormalities''' — Globulins tend to be increased <ref name="pmid4123153">{{cite journal |vauthors=Triger DR, Wright R |title=Hyperglobulinaemia in liver disease |journal=Lancet |volume=1 |issue=7818 |pages=1494–6 |year=1973 |pmid=4123153 |doi= |url=}}</ref>
| |
| * Disseminated intravascular coagulation
| |
| * Fibrinolysis
| |
| * Vitamin K deficiency
| |
| * Dysfibrinogenemia
| |
| * Insulin resistance: nonalcoholic fatty liver disease
| |
| * Diabetes: seen in patients with hemochromatosis <ref name="pmid8020880">{{cite journal |vauthors=Bianchi G, Marchesini G, Zoli M, Bugianesi E, Fabbri A, Pisi E |title=Prognostic significance of diabetes in patients with cirrhosis |journal=Hepatology |volume=20 |issue=1 Pt 1 |pages=119–25 |year=1994 |pmid=8020880 |doi= |url=}}</ref><ref name="pmid8119686">{{cite journal |vauthors=Petrides AS, Vogt C, Schulze-Berge D, Matthews D, Strohmeyer G |title=Pathogenesis of glucose intolerance and diabetes mellitus in cirrhosis |journal=Hepatology |volume=19 |issue=3 |pages=616–27 |year=1994 |pmid=8119686 |doi= |url=}}</ref>
| |
| '''Radiologic findings:'''
| |
| * Radiologic studies include:<ref name="pmid22357834">{{cite journal |vauthors=Udell JA, Wang CS, Tinmouth J, FitzGerald JM, Ayas NT, Simel DL, Schulzer M, Mak E, Yoshida EM |title=Does this patient with liver disease have cirrhosis? |journal=JAMA |volume=307 |issue=8 |pages=832–42 |year=2012 |pmid=22357834 |doi=10.1001/jama.2012.186 |url=}}</ref>
| |
| ** Abdominal ultrasound
| |
| ** Computed tomography scan
| |
| ** Magnetic resonance imaging
| |
| | |
| * Findings may include:<ref name="pmid3533689">{{cite journal |vauthors=Becker CD, Scheidegger J, Marincek B |title=Hepatic vein occlusion: morphologic features on computed tomography and ultrasonography |journal=Gastrointest Radiol |volume=11 |issue=4 |pages=305–11 |year=1986 |pmid=3533689 |doi= |url=}}</ref><ref name="pmid3533689">{{cite journal |vauthors=Becker CD, Scheidegger J, Marincek B |title=Hepatic vein occlusion: morphologic features on computed tomography and ultrasonography |journal=Gastrointest Radiol |volume=11 |issue=4 |pages=305–11 |year=1986 |pmid=3533689 |doi= |url=}}</ref><ref name="pmid2526349">{{cite journal |vauthors=Di Lelio A, Cestari C, Lomazzi A, Beretta L |title=Cirrhosis: diagnosis with sonographic study of the liver surface |journal=Radiology |volume=172 |issue=2 |pages=389–92 |year=1989 |pmid=2526349 |doi=10.1148/radiology.172.2.2526349 |url=}}</ref><ref name="pmid3891495">{{cite journal |vauthors=Sanford NL, Walsh P, Matis C, Baddeley H, Powell LW |title=Is ultrasonography useful in the assessment of diffuse parenchymal liver disease? |journal=Gastroenterology |volume=89 |issue=1 |pages=186–91 |year=1985 |pmid=3891495 |doi= |url=}}</ref><ref name="pmid3532188">{{cite journal |vauthors=Giorgio A, Amoroso P, Lettieri G, Fico P, de Stefano G, Finelli L, Scala V, Tarantino L, Pierri P, Pesce G |title=Cirrhosis: value of caudate to right lobe ratio in diagnosis with US |journal=Radiology |volume=161 |issue=2 |pages=443–5 |year=1986 |pmid=3532188 |doi=10.1148/radiology.161.2.3532188 |url=}}</ref><ref name="pmid10341686">{{cite journal |vauthors=Simonovský V |title=The diagnosis of cirrhosis by high resolution ultrasound of the liver surface |journal=Br J Radiol |volume=72 |issue=853 |pages=29–34 |year=1999 |pmid=10341686 |doi=10.1259/bjr.72.853.10341686 |url=}}</ref>
| |
| ** A liver that appears shrunken, irregular, and nodular.
| |
| | |
| * Evidence of Portal HTN:
| |
| ** varices
| |
| ** Ascites
| |
| '''DIAGNOSIS''' —
| |
| * Abdominal imaging (typically ultrasound) helps:
| |
| ** Evaluate the liver parenchyma
| |
| ** Detects extrahepatic manifestations of cirrhosis
| |
| '''Laboratory tests:'''
| |
| * AST to platelet ratio index
| |
| * FibroTest/FibroSure
| |
| '''Imaging studies:'''
| |
| * Findings on abdominal imaging are viewed in light of other signs of cirrhosis, such as physical examination or laboratory test findings.
| |
| * In addition to evaluating the liver, abdominal imaging may reveal:
| |
| ** Hepatocellular carcinoma
| |
| ** Extrahepatic findings suggestive of cirrhosis:
| |
| *** Ascites
| |
| *** Varices
| |
| *** Splenomegaly
| |
| *** Hepatic or portal vein thrombosis
| |
| | |
| * Imaging may indicate etiology of cirrhosis:
| |
| '''CT'''
| |
| * Computed tomography (CT) scanning complements ultrasound imaging.
| |
| * Classical appearances in some diseases:
| |
| ** Haemochromatosis: where the excess iron deposition causes a dramatic increase in hepatic density.
| |
| * A hypertrophied caudate lobe discovered on computed tomographic (CT) scanning, for example, suggests Budd-Chiari syndrome.
| |
| '''MRI'''<ref name="pmid9129412">{{cite journal |vauthors=Ernst O, Sergent G, Bonvarlet P, Canva-Delcambre V, Paris JC, L'Herminé C |title=Hepatic iron overload: diagnosis and quantification with MR imaging |journal=AJR Am J Roentgenol |volume=168 |issue=5 |pages=1205–8 |year=1997 |pmid=9129412 |doi=10.2214/ajr.168.5.9129412 |url=}}</ref><ref name="pmid10405746">{{cite journal |vauthors=Bonkovsky HL, Rubin RB, Cable EE, Davidoff A, Rijcken TH, Stark DD |title=Hepatic iron concentration: noninvasive estimation by means of MR imaging techniques |journal=Radiology |volume=212 |issue=1 |pages=227–34 |year=1999 |pmid=10405746 |doi=10.1148/radiology.212.1.r99jl35227 |url=}}</ref><ref name="pmid7972774">{{cite journal |vauthors=Gandon Y, Guyader D, Heautot JF, Reda MI, Yaouanq J, Buhé T, Brissot P, Carsin M, Deugnier Y |title=Hemochromatosis: diagnosis and quantification of liver iron with gradient-echo MR imaging |journal=Radiology |volume=193 |issue=2 |pages=533–8 |year=1994 |pmid=7972774 |doi=10.1148/radiology.193.2.7972774 |url=}}</ref><ref name="pmid10470885">{{cite journal |vauthors=Ito K, Mitchell DG, Hann HW, Kim Y, Fujita T, Okazaki H, Honjo K, Matsunaga N |title=Viral-induced cirrhosis: grading of severity using MR imaging |journal=AJR Am J Roentgenol |volume=173 |issue=3 |pages=591–6 |year=1999 |pmid=10470885 |doi=10.2214/ajr.173.3.10470885 |url=}}</ref><ref name="pmid10352597">{{cite journal |vauthors=Ito K, Mitchell DG, Gabata T, Hussain SM |title=Expanded gallbladder fossa: simple MR imaging sign of cirrhosis |journal=Radiology |volume=211 |issue=3 |pages=723–6 |year=1999 |pmid=10352597 |doi=10.1148/radiology.211.3.r99ma31723 |url=}}</ref><ref name="pmid9609897">{{cite journal |vauthors=Ito K, Mitchell DG, Hann HW, Outwater EK, Kim Y, Fujita T, Okazaki H, Honjo K, Matsunaga N |title=Progressive viral-induced cirrhosis: serial MR imaging findings and clinical correlation |journal=Radiology |volume=207 |issue=3 |pages=729–35 |year=1998 |pmid=9609897 |doi=10.1148/radiology.207.3.9609897 |url=}}</ref><ref name="pmid10470885">{{cite journal |vauthors=Ito K, Mitchell DG, Hann HW, Kim Y, Fujita T, Okazaki H, Honjo K, Matsunaga N |title=Viral-induced cirrhosis: grading of severity using MR imaging |journal=AJR Am J Roentgenol |volume=173 |issue=3 |pages=591–6 |year=1999 |pmid=10470885 |doi=10.2214/ajr.173.3.10470885 |url=}}</ref><ref name="pmid8273643">{{cite journal |vauthors=Finn JP, Kane RA, Edelman RR, Jenkins RL, Lewis WD, Muller M, Longmaid HE |title=Imaging of the portal venous system in patients with cirrhosis: MR angiography vs duplex Doppler sonography |journal=AJR Am J Roentgenol |volume=161 |issue=5 |pages=989–94 |year=1993 |pmid=8273643 |doi=10.2214/ajr.161.5.8273643 |url=}}</ref>
| |
| * Magnetic resonance imaging (MRI):
| |
| ** determines the nature of focal lesions such as hepatic metastases
| |
| ** nodular regeneration
| |
| * Decreased signal intensity on magnetic resonance imaging may indicate iron overload from hereditary hemochromatosis.
| |
| '''Ultrasonography:''' routinely used during the evaluation of cirrhosis
| |
| * First-line investigation of choice.
| |
| * The first radiologic study obtained due to easy availability.
| |
| | |
| * Provides information about :
| |
| ** appearance of the liver
| |
| ** blood flow within the portal circulation
| |
| | |
| * less expensive than other imaging modalities
| |
| | |
| * No exposure to intravenous contrast or radiation
| |
| | |
| * Noninvasive
| |
| * cheap
| |
| * safe
| |
| | |
| * well tolerated
| |
| | |
| * widely available
| |
| * Ultrasound, particularly with colour Doppler imaging :
| |
| ** measures changes in blood flow in the presence of portal hypertension
| |
| ** excludes biliary obstruction in patients who present with jaundice
| |
| | |
| * Early signs of cirrhosis in B-ultrasonography include:
| |
| ** inhomogeneity of the hepatic tissue
| |
| ** Irregularity of the hepatic surface
| |
| ** enlargement of the caudate lobe
| |
| ** Splenomegaly due to portal HTN
| |
| | |
| * The diagnostic evaluation of cirrhosis with ultrasonography is based on the direct relation between the extent of fibrosis and the ultrasonographically determined degree of liver stiffness.
| |
| | |
| * ultrasonography can rule cirrhosis in or out in over 90% of cases , its findings are less than 100% specific because of occasional in -correct measurements and false-positive findings
| |
| | |
| * Findings:
| |
| ** Advanced cirrhosis: liver may appear small and nodular
| |
| ** Surface nodularity and increased echogenicity with irregular appearing areas are consistent with cirrhosis
| |
| ** Usually atrophy of the right lobe and hypertrophy of the caudate or left lobes.
| |
| | |
| * Ultrasonography may also be used as a screening test for hepatocellular carcinoma :nodules on ultrasonography warrants further evaluation
| |
| * Findings of portal hypertension:
| |
| ** increased diameter of the portal vein
| |
| ** presence of collateral veins
| |
| ** decreased flow within the portal circulation on Doppler imaging
| |
| * Ultrasonography is also useful for detecting splenomegaly, ascites, and portal vein thrombosis.
| |
| '''Computed tomography '''– not routinely used in the diagnosis of cirrhosis
| |
| * It provides similar information to ultrasonography, but at the expense of radiation and contrast exposure.
| |
| | |
| * CT findings:
| |
| ** Hepatic nodularity
| |
| ** Atrophy of the right lobe
| |
| ** Hypertrophy of the caudate or left lobes
| |
| ** Ascites
| |
| ** Varices
| |
| * CT portal phase imaging:
| |
| ** Patency of the portal vein can be demonstrated
| |
| '''Magnetic resonance imaging:'''
| |
| * The role of magnetic resonance imaging (MRI) in the diagnosis of cirrhosis is unclear.
| |
| * Use is limited by expense
| |
| * Poor tolerance of the examination
| |
| * Ability to obtain information provided by MRI through other means
| |
| * reveal iron overload and provide an estimate of the hepatic iron concentration
| |
| * Magnetic resonance angiography (MRA) is more sensitive than ultrasonography for diagnosing complications of cirrhosis:
| |
| * portal vein thrombosis
| |
| * CT portal phase imaging, MRA can determine the volume and direction of blood flow in the portal vein.
| |
| '''Elastography:'''
| |
| * Increasing scarring of the liver is associated with increasing "stiffness" of the tissue.
| |
| '''Nuclear studies:'''
| |
| * Radionuclide testing can be useful in suggesting the diagnosis of cirrhosis:<ref name="pmid3995244">{{cite journal |vauthors=McLaren MI, Fleming JS, Walmsley BH, Ackery DM, Taylor I, Karran SJ |title=Dynamic liver scanning in cirrhosis |journal=Br J Surg |volume=72 |issue=5 |pages=394–6 |year=1985 |pmid=3995244 |doi= |url=}}</ref>
| |
| ** 99mTc sulfur colloid is normally taken up by cells of the reticuloendothelial system
| |
| ** Cirrhosis: heterogeneity in the uptake of 99mTc sulfur colloid by the liver and increased uptake by the spleen and bone marrow
| |
| | |
| ==== Endoscopic retrograde cholangiopancreatography ====
| |
| * diagnosis of sclerosing cholangitis
| |
| '''Liver biopsy:''' <ref name="pmid9683971">{{cite journal |vauthors=Williams EJ, Iredale JP |title=Liver cirrhosis |journal=Postgrad Med J |volume=74 |issue=870 |pages=193–202 |year=1998 |pmid=9683971 |pmc=2360862 |doi= |url=}}</ref>
| |
| * Cirrhosis is primarily a histological diagnosis.
| |
| * Percutaneous liver biopsy remains the cornerstone of diagnosis.
| |
| * quick and simple to perform in a cooperative patient with a normal INR and platelet count.
| |
| * The gold standard for diagnosing cirrhosis is:
| |
| ** Examination of an explanted liver, either at autopsy or following liver transplantation, because the architecture of the entire liver can be appreciated.
| |
| | |
| * Cirrhosis is diagnosed with a liver biopsy
| |
| | |
| * Sample of the liver is obtained by:
| |
| ** Percutaneous
| |
| ** Transjugular
| |
| ** Laparoscopic radiographically-guided fine-needle approach.
| |
| | |
| * Liver biopsy is not necessary if the clinical, laboratory, and radiologic data strongly suggest the presence of cirrhosis and if the results would not alter the patient's management.
| |
| | |
| * Patient with a history of heavy alcohol use who has ascites, severe coagulopathy, and a shrunken, nodular-appearing liver on ultrasonography.
| |
| | |
| * Liver biopsy may be suggestive of etiology:
| |
| * Metabolic causes of cirrhosis include:
| |
| ** Hereditary hemochromatosis
| |
| ** Nonalcoholic steatohepatitis
| |
| ** Wilson disease
| |
| ** Alpha-1 antitrypsin deficiency
| |
| | |
| * Risks:
| |
| ** haemorrhage
| |
| ** biliary peritonitis
| |
| ** haematoma
| |
| ** perforation of other viscera
| |
| ** mortality rates of between 0.01% and 0.1%
| |
| | |
| * Percutaneous biopsy of focal lesions may be performed in combination with either ultrasound or CT imaging.
| |
| | |
| * Prerequisites:
| |
| ** normal INR and platelet count.
| |
| | |
| * May be performed in combination with either ultrasound or CT.
| |
| * Patients with moderate coagulopathy:
| |
| ** Plugged liver biopsy : injection of gelatin sponges or metal coils down the tract after biopsy
| |
| ** Laparoscopic liver biopsy performed on a sedated patient with moderate coagulopathy
| |
| *** Advantage: allows direct visualisation of the liver
| |
| | |
| * Patients with severe clotting disorders:
| |
| * Transjugular liver biopsy :
| |
| ** risk of intraperitoneal bleed is less
| |
| ** Disadvantages:
| |
| *** biopsies are small: multiple biopsies required
| |
| *** taken 'blindly'
| |
| | |
| ===rough===
| |
| '''Diagnosis of Cirrhosis'''
| |
| | |
| '''Laboratory findings''' —
| |
| | |
| Laboratory abnormalities may be the first indication of cirrhosis.
| |
| | |
| Common abnormalities include:
| |
| | |
| Increased serum bilirubin levels
| |
| | |
| Abnormal aminotransferase levels
| |
| | |
| Elevated alkaline phosphatase / gamma-glutamyl transpeptidase
| |
| | |
| Prolonged prothrombin time
| |
| | |
| Elevated international normalized ratio (INR)
| |
| | |
| Hyponatremia
| |
| | |
| Thrombocytopenia
| |
| | |
| '''Liver function tests''' . .
| |
| | |
| ●Aminotransferases –
| |
| | |
| Aspartate aminotransferase (AST) and alanine aminotransferase (ALT) are usually moderately elevated
| |
| | |
| AST is more often elevated than ALT
| |
| | |
| Levels may be normal
| |
| | |
| ●Alkaline phosphatase –
| |
| | |
| Alkaline phosphatase is usually elevated
| |
| | |
| High levels may be seen in patients with underlying cholestatic liver disease such as
| |
| | |
| primary sclerosing cholangitis
| |
| | |
| primary biliary cirrhosis
| |
| | |
| ●Gamma-glutamyl transpeptidase –
| |
| | |
| Non specific
| |
| | |
| Correlates with ALP levels
| |
| | |
| Higher in CLD due to alcohol use:
| |
| | |
| Alcohol causes GGT release from hepatocytes
| |
| | |
| Alcohol induces microsomal GGT in liver
| |
| | |
| ●Bilirubin – Bilirubin levels may be normal or raised
| |
| | |
| ●Albumin – Albumin levels reflect synthetic function of the liver
| |
| | |
| Serum albumin levels helps grade the severity of cirrhosis
| |
| | |
| Hypoalbuminemia is non specific for liver disease: heart failure, nephrotic syndrome, protein losing enteropathy, or malnutrition.
| |
| | |
| ●Prothrombin time – Prothrombin time reflects the degree of hepatic synthetic function.
| |
| | |
| Worsening coagulopathy correlates with the severity of hepatic dysfunction.
| |
| | |
| '''Serum chemistries''' —
| |
| | |
| Hyponatremia is common in patients with cirrhosis and ascites and is related to an inability to excrete free water.
| |
| | |
| Due to ADH elevation
| |
| | |
| Reflects poor prognosis
| |
| | |
| progressive rise in serum creatinine: hepatorenal syndrome
| |
| | |
| '''Hematologic abnormalities''' —
| |
| | |
| '''Thrombocytopenia''':most common
| |
| | |
| Mechanism of thrombocytopenia:
| |
| | |
| caused by portal hypertension with congestive splenomegaly: sequesters circulating platelets
| |
| | |
| Decreased thrombopoietin levels
| |
| | |
| '''Leukopenia/neutropenia''': due to hypersplenism with splenic margination.
| |
| | |
| '''Anemia'''
| |
| | |
| Mechanism of anemia:
| |
| | |
| Acute and chronic gastrointestinal blood loss
| |
| | |
| Folate deficiency
| |
| | |
| Direct toxicity due to alcohol
| |
| | |
| Hypersplenism
| |
| | |
| Bone marrow suppression ( hepatitis-associated aplastic anemia)
| |
| | |
| Anemia of chronic disease (inflammation)
| |
| | |
| Hemolysis
| |
| | |
| '''Other abnormalities''' — Globulins tend to be increased
| |
| | |
| Disseminated intravascular coagulation
| |
| | |
| Fibrinolysis
| |
| | |
| Vitamin K deficiency
| |
| | |
| Dysfibrinogenemia
| |
| | |
| Insulin resistance: nonalcoholic fatty liver disease
| |
| | |
| Diabetes: seen in patients with hemochromatosis
| |
| | |
| '''Radiologic findings''' — Radiologic studies include:
| |
| | |
| Abdominal ultrasound
| |
| | |
| Computed tomography scan
| |
| | |
| Magnetic resonance imaging
| |
| | |
| Findings may include:
| |
| | |
| A liver that appears shrunken, irregular, and nodular.
| |
| | |
| Evidence of Portal HTN:
| |
| | |
| varices
| |
| | |
| Ascites
| |
| | |
| '''DIAGNOSIS''' —
| |
| | |
| Abdominal imaging (typically ultrasound) helps:
| |
| | |
| Evaluate the liver parenchyma
| |
| | |
| Detects extrahepatic manifestations of cirrhosis
| |
| | |
| '''Laboratory tests''' — AST to platelet ratio index
| |
| | |
| FibroTest/FibroSure
| |
| | |
| '''Imaging studies''' — Findings on abdominal imaging are viewed in light of other signs of cirrhosis, such as physical examination or laboratory test findings.
| |
| | |
| In addition to evaluating the liver, abdominal imaging may reveal:
| |
| | |
| Hepatocellular carcinoma
| |
| | |
| Extrahepatic findings suggestive of cirrhosis:
| |
| | |
| ascites,
| |
| | |
| varices,
| |
| | |
| splenomegaly,
| |
| | |
| hepatic or portal vein thrombosis.
| |
| | |
| Diagnosis
| |
| | |
| Diagnosis
| |
| | |
| '''-USG''': first line investigation of choice
| |
| | |
| ''' Ultrasound''' '''with colour Doppler imaging''' measures changes in blood flow due to portal hypertension
| |
| | |
| excludes biliary obstruction in jaundiced patients
| |
| | |
| safe
| |
| | |
| cheap
| |
| | |
| Noninvasive
| |
| | |
| Early signs of cirrhosis in B-ultrasonography include:
| |
| | |
| inhomogeneity of the hepatic tissue
| |
| | |
| Irregularity of the hepatic surface
| |
| | |
| enlargement of the caudate lobe
| |
| | |
| Splenomegaly due to portal HTN
| |
| | |
| The diagnostic evaluation of cirrhosis with ultrasonography is based on the direct relation between the extent of fibrosis and the ultrasonographically determined degree of liver stiffness.
| |
| | |
| ultrasonography can rule cirrhosis in or out in over 90% of cases , its findings are less than 100% specific because of occasional in -correct measurements and false-positive findings
| |
| | |
| '''-Computed tomography (CT) scanning :'''
| |
| | |
| Classical appearances in some diseases, eg, haemochromatosis: Heaptic density increases due to excess iron deposition
| |
| | |
| '''-Magnetic resonance imaging (MRI)'''
| |
| | |
| Helps differentiaiting focal lesions based on their nature:
| |
| | |
| hepatic metastases
| |
| | |
| nodular regeneration
| |
| | |
| '''-endoscopic retrograde cholangiopancreatography''': in diagnosis of sclerosing cholangitis
| |
| | |
| '''-Liver biopsy'''
| |
| | |
| Cirrhosis is primarily a histological diagnosis
| |
| | |
| -Prerequisites:
| |
| | |
| normal INR and platelet count.
| |
| | |
| -Risks
| |
| | |
| Haemorrhage
| |
| | |
| biliary peritonitis
| |
| | |
| haematoma
| |
| | |
| perforation of other viscera
| |
| | |
| mortality rates of between 0.01% and 0.1%
| |
| | |
| May be performed in combination with either ultrasound or CT.
| |
| | |
| -Patients with moderate coagulopathy:
| |
| | |
| Plugged liver biopsy : injection of gelatin sponges or metal
| |
| | |
| coils down the tract after biopsy.
| |
| | |
| Laparoscopic liver biopsy performed on a sedated patient with moderate coagulopathy
| |
| | |
| Advantage: allows direct visualisation of the liver
| |
| | |
| -patients with severe clotting disorders: Transjugular liver biopsy :
| |
| | |
| risk of intraperitoneal bleed is less
| |
| | |
| Disadvantages:
| |
| | |
| biopsies are small: multiple biopsies required
| |
| | |
| taken 'blindly'
| |
| | |
| Findings in liver biopsy
| |
| | |
| Fibrous septa between the portal fields
| |
| | |
| Nodules- micronodular, macronodular
| |
| | |
| In advanced liver disease approaching the stage of cirrhosis:
| |
| | |
| thrombocytopenia
| |
| | |
| Impaired hepatic biosynthesis
| |
| | |
| Low concentration of albumin
| |
| | |
| Low concentration of cholinesterase
| |
| | |
| elevation of the international normalized ratio [INR])
| |
| | |
| impairment of the detoxifying function of the liver : e.g., elevated bilirubin concentration
| |
| | |
| transaminase levels are generally in the normal range or only mildly elevated.
| |
| | |
| Ancillary studies include:
| |
| | |
| Upper abdominal ultrasonography
| |
| | |
| Gastroscopy
| |
| | |
| Esophagogastroduo -denoscopy (EGD) : used to demonstrate eso -phageal varices
| |
| | |
| Assessment of bleeding
| |
| | |
| Performed in all cases of cirrhosis
| |
| | |
| Liver biopsy is contraindicated, if the diagnosis of cirrhosis has been clearly established
| |
| | |
| from the clinical findings and imaging:
| |
| | |
| evidence of decompensation, with ascites
| |
| | |
| Labs indicating impaired hepatic biosynthesis
| |
| | |
| Liver biopsy is indicated :
| |
| | |
| etiology of liver disease is unclear
| |
| | |
| stage cannot be determined: length of punch cylinders used for liver biopsy should be atleast 15 mm long, and at least 10 portal fields should be examined per sectional level
| |
| | |
| diagnosis in doubt
| |
| | |
| if the biopsy is expected to yield information about the cause of cirrhosis that will affect the treatment choice
| |
| | |
| Noninvasive diagnostic evaluation of cirrhosis
| |
| | |
| Laboratory-based methods:
| |
| | |
| Routine liver function tests
| |
| | |
| Hyaluronic acid concentration
| |
| | |
| AST-to-platelet ratio index: (APRI) is easily calculated as the quotient of the AST
| |
| | |
| (GOT)
| |
| | |
| Platelet count: screening index for advanced fibrosis and cirrhosis
| |
| | |
| Transient elastography and the acoustic radiation force impulse (ARFI) technique are now well-established methods for the staging of fibrosis in various liver diseases
| |
|
| |
| -USG: first line investigation of choice
| |
| Ultrasound with colour Doppler imaging measures changes in blood flow due to portal hypertension
| |
| excludes biliary obstruction in jaundiced patients
| |
| safe
| |
| cheap
| |
| Noninvasive
| |
| | |
| Early signs of cirrhosis in B-ultrasonography include:
| |
| | |
| inhomogeneity of the hepatic tissue
| |
| Irregularity of the hepatic surface
| |
| enlargement of the caudate lobe
| |
| Splenomegaly due to portal HTN
| |
| | |
| -Computed tomography (CT) scanning :
| |
| Classical appearances in some diseases, eg, haemochromatosis: Heaptic density increases due to excess iron deposition
| |
| | |
| -Magnetic resonance imaging (MRI)
| |
| Helps differentiaiting focal lesions based on their nature:
| |
| hepatic metastases
| |
| nodular regeneration
| |
| | |
| | |
| | |
| -endoscopic retrograde cholangiopancreatography: in diagnosis of sclerosing
| |
| cholangitis.
| |
| | |
| -Liver biopsy
| |
| Cirrhosis is primarily a histological diagnosis.
| |
| | |
|
| |
| -Prerequisites:
| |
| normal INR and platelet count.
| |
| | |
| -Risks
| |
| Haemorrhage
| |
| biliary peritonitis
| |
| haematoma
| |
| perforation of other viscera
| |
| mortality rates of between 0.01% and 0.1%
| |
| | |
| May be performed in combination with either ultrasound or CT.
| |
| | |
| -Patients with moderate coagulopathy:
| |
| Plugged liver biopsy : injection of gelatin sponges or metal
| |
| coils down the tract after biopsy.
| |
| | |
| Laparoscopic liver biopsy performed on a sedated patient with moderate coagulopathy
| |
| Advantage: allows direct visualisation of the liver
| |
| | |
| | |
| -patients with severe clotting disorders: Transjugular liver biopsy :
| |
| risk of intraperitoneal bleed is less
| |
| | |
| Disadvantages:
| |
| biopsies are small: multiple biopsies required
| |
| taken 'blindly'
| |
| | |
| | |
| | |
| Findings in liver biopsy
| |
| Fibrous septa between the portal fields
| |
| Nodules- micronodular, macronodular
| |
| | |
| | |
| In advanced liver disease approaching the stage of cirrhosis:
| |
| thrombocytopenia
| |
| Impaired hepatic biosynthesis
| |
| Low concentration of albumin
| |
| Low concentration of cholinesterase
| |
| elevation of the international normalized ratio [INR])
| |
| impairment of the detoxifying function of the liver : e.g., elevated bilirubin concentration
| |
| transaminase levels are generally in the normal range or only mildly elevated.
| |
| | |
| Findings in liver biopsy
| |
| | |
| Fibrous septa between the portal fields
| |
| | |
| Nodules- micronodular, macronodular
| |
| | |
| In advanced liver disease approaching the stage of cirrhosis:
| |
| | |
| thrombocytopenia
| |
| | |
| Impaired hepatic biosynthesis
| |
| | |
| Low concentration of albumin
| |
| | |
| Low concentration of cholinesterase
| |
| | |
| Elevation of the international normalized ratio [INR])
| |
| | |
| Impairment of the detoxifying function of the liver : e.g., elevated bilirubin concentration
| |
| | |
| transaminase levels are generally in the normal range or only mildly elevated.
| |
| | |
| Ancillary studies include:
| |
| | |
| Upper abdominal ultrasonography
| |
| | |
| Gastroscopy
| |
| | |
| Esophagogastroduo -denoscopy (EGD) : used to demonstrate eso -phageal varices
| |
| | |
| Assessment of bleeding
| |
| | |
| Performed in all cases of cirrhosis
| |
| | |
| Liver biopsy is contraindicated, if the diagnosis of cirrhosis has been clearly established
| |
| | |
| from the clinical findings and imaging:
| |
| | |
| Evidence of decompensation, with ascites
| |
| | |
| Labs indicating impaired hepatic biosynthesis
| |
| | |
| Liver biopsy is indicated :
| |
| | |
| Etiology of liver disease is unclear
| |
| | |
| Stage cannot be determined: length of punch cylinders used for liver biopsy should be atleast 15 mm long, and at least 10 portal fields should be examined per sectional level
| |
| | |
| Diagnosis in doubt
| |
| | |
| If the biopsy is expected to yield information about the cause of cirrhosis that will affect the treatment choice
| |
| | |
| Noninvasive diagnostic evaluation of cirrhosis
| |
| | |
| Laboratory-based methods:
| |
| | |
| Routine liver function tests
| |
| | |
| Hyaluronic acid concentration
| |
| | |
| AST-to-platelet ratio index: (APRI) is easily calculated as the quotient of the AST
| |
| | |
| (GOT)
| |
| | |
| Platelet count: screening index for advanced fibrosis and cirrhosis
| |
| | |
| Transient elastography and the acoustic radiation force impulse (ARFI) technique are now well-established methods for the staging of fibrosis in various liver diseases
| |
| | |
| '''Is Liver Biopsy the Gold Standard'''
| |
| | |
| '''in the Diagnosis of Cirrhosis?'''
| |
| | |
| Liver biopsy is the gold standard in the diagnosis of cirrhosis, it is an imperfect test.
| |
| | |
| It is an invasive procedure with complications:
| |
| | |
| Sampling errors
| |
| | |
| Death
| |
| | |
| '''Measurement of hepatic venous pressure gradient (HVPG)''':
| |
| | |
| Indirect measure of sinusoidal pressure obtained through hepatic vein catheterization, has a greater diagnostic accuracy than liver biopsy.
| |
| | |
| Very accurate in predicting the development of disease progression and the presence of significant fibrosis.
| |
| | |
| HVPG measurement of 6 mmHg or greater indicates the presence of cirrhosis.
| |
| | |
| HVPG addresses a larger area of hepatic parenchyma than liver biopsy, since the pressure obtained is
| |
| | |
| the average pressure of many sinusoids, thus reducing the possibility of sampling error due to
| |
| | |
| the presence of fibrosis heterogeneity within the diseased liver.
| |
| | |
| Noninvasive tests including serum markers, ultrasound, and liver and/or spleen stiffness measurements have become important tools in ruling in or excluding cirrhosis with a high diagnostic accuracy and may substitute for liver biopsy in the diagnosis of cirrhosis.
| |
| | |
| '''Laboratory findings''' —
| |
| | |
| Laboratory abnormalities may be the first indication of cirrhosis.
| |
| | |
| Common abnormalities include:
| |
| | |
| Increased serum bilirubin levels
| |
| | |
| abnormal aminotransferases
| |
| | |
| elevated alkaline phosphatase/gamma-glutamyl transpeptidase
| |
| | |
| prolonged prothrombin time
| |
| | |
| elevated international normalized ratio (INR)
| |
| | |
| Hyponatremia
| |
| | |
| Thrombocytopenia
| |
| | |
| <font color="red">Cherry</font>
| |
| | |
| | |
| | |
| ==Physical Examination==
| |
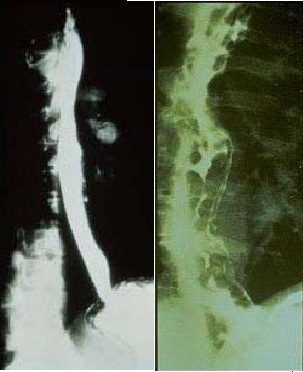
| [[Image: Normal versus Abnormal Barium study of esophagus.jpg|thumb|left|200px|Normal versus Abnormal Barium study of esophagus with varices]]
| |
| | |
| | |
| ===GIF maker===
| |
| | |
| [[File:Cirrhosis baba gif.gif|500px|right|thumb|Liver Cirhhosis <br> Source:Wikimedia commons<ref name="urlCategory:Histopathology of cirrhosis - Wikimedia Commons">{{cite web |url=https://commons.wikimedia.org/wiki/Category:Histopathology_of_cirrhosis#/media/File:Cirrhosis_high_mag.jpg |title=Category:Histopathology of cirrhosis - Wikimedia Commons |format= |work= |accessdate=}}</ref>]]
| |
| | |
| | |
| | |
| [[File:Spider angioma p.jpg|500px|center|thumb|Spider angiomata <br> Source:Wikimedia commons ]]
| |
| [[File:Output OBujt7.gif|500px|left|thumb|Spider angiomata <br> Source:Wikimedia commons]]
| |
| | |
| | |
| | |
| ==Physical Examination==
| |
| | |
| *Physical examination of [[Patient|patients]] with [[cirrhosis]] is usually remarkable for: [[jaundice]], [[Spider angioma|spider angiomata]], [[ascites]], [[asterixis]], [[Splenomegaly|spleenomegaly]] and [[palmar erythema]].
| |
| | |
| ===Appearance of the Patient===
| |
| | |
| *[[Patient|Patients]] with [[cirrhosis]] usually appear weak due to constitutional [[Symptom|symptoms]] such as [[weight loss]], [[anorexia]] and [[muscle atrophy]]. Yellowish discoloration of [[skin]] and [[abdominal distension]] may also be present due to [[ascites]].
| |
| | |
| *Normal/low [[blood pressure]] with normal [[pulse pressure]].
| |
| | |
| ===Skin===
| |
| *[[Jaundice]] : yellow discoloration of the skin, eyes, and mucus membranes due to increased [[bilirubin]] (at least 2-3 mg/dL or 30 mmol/L). Urine may also appear dark.
| |
| *[[Pallor]]
| |
| *[[Bruise|Bruises]]
| |
| *[[Palmar erythema]] on the [[Thenar eminence|thenar]] and [[Hypothenar eminence|hypothenar eminences]], due to altered sex hormone metabolism.
| |
| *[[Spider angioma|Spider angiomata]]: Increased estradiol levels lead to the formation of vascular lesions consisting of central arterioles surrounded by smaller vessels <ref name="pmid10423070">{{cite journal |author=Li CP, Lee FY, Hwang SJ, ''et al'' |title=Spider angiomas in patients with liver cirrhosis: role of alcoholism and impaired liver function|journal=Scand. J. Gastroenterol. |volume=34 |issue=5 |pages=520-3 |year=1999 |pmid=10423070 |doi=}}</ref>
| |
| *'''[[Telangiectasia|Telangiectasias]]''' or '''spider veins:''' small dilated [[blood vessel]]s near the surface of the [[skin]].
| |
| | |
| ===HEENT===
| |
| * Abnormalities of the head/hair may include thinning of hair on the scalp due to [[hyperestrogenism]]
| |
| * '''[[Kayser-Fleischer ring]]s''' : dark rings that appear to encircle the [[iris (anatomy)|iris]] of the [[eye]] in [[Patient|patients]] with [[Wilson's disease]].
| |
| * [[Parotid gland]] enlargement
| |
| * [[Fetor hepaticus]]: severe portal-systemic shunting leads to increased levels of [[dimethyl sulfide]] leads to a sweet pungent smell in the breath
| |
| | |
| ===Abdomen===
| |
| * Inspection:
| |
| ** [[Abdominal distension]]
| |
| ** [[Caput medusae]]
| |
| | |
| * Palpation:
| |
| ** Fluid wave
| |
| ** [[Hepatomegaly]] may be present in initial stages. The liver may also be normal or shrunken.
| |
| ** [[Splenomegaly|Spleenomegaly]] may be present in patients with [[cirrhosis]] from nonalcoholic etiologies, due to portal hypertension
| |
| | |
| * Percussion:
| |
| ** Flank dullness may be present due to [[ascites]] (needs approximately 1500ml for detection)
| |
| | |
| * Auscultation:
| |
| ** [[Cruveilhier-Baumgarten murmur]]: venous hum that may be present in patients with [[portal hypertension]].
| |
| *** Mechanism: due to collateral connections between remnant of the [[umbilical vein]] and the [[Portal venous system|portal system]]
| |
| *** Location: [[Epigastrium]]
| |
| *** Exacerbating factors: [[Valsalva maneuver]]
| |
| *** Diminished by: application of [[pressure]] on the [[skin]] above the [[Navel|umbilicus]]
| |
| | |
| ===Genitourinary===
| |
| *[[Testicular atrophy]]
| |
| *Inversion of the normal male [[pubic hair]] pattern
| |
| ===Neuromuscular===
| |
| * [[Hepatic encephalopathy]] may have signs of:
| |
| ** Alteration of [[Mental status examination|mental status]]
| |
| ** [[Confusion]]
| |
| ** [[Coma]]
| |
| * [[Asterixis]] (bilateral but asynchronous flapping motions of outstretched, dorsiflexed hands) is seen in patients with [[hepatic encephalopathy]].
| |
| | |
| ===Extremities===
| |
| *[[edema]] of the lower extremities
| |
| *[[Muscle atrophy]]
| |
| *Nail changes:
| |
| **Muehrcke nails: paired horizontal white bands separated by normal color due to [[hypoalbuminemia]]
| |
| **Terry nails: the proximal two-thirds of the nail plate appears white, whereas the distal one-third is red due to [[hypoalbuminemia]]
| |
| ** [[Clubbing]]: the angle between the nail plate and proximal nail fold is greater than 180 degrees
| |
| **Severe [[clubbing]]:
| |
| ***"Drum stick" appearance of distal fingers
| |
| ***[[Hypertrophic pulmonary osteoarthropathy|Hypertrophic osteoarthropathy]]: chronic proliferative [[periostitis]] of the [[long bones]]
| |
| **[[Dupuytrens contracture|Dupuytren's contracture]] may cause flexion deformities of the fingers: This occurs due to shortening and thickening of the palmar fascia, due to collagen deposition and fibroblastic proliferation.
| |
| **[[Asterixis]] in cases with [[hepatic encephalopathy]]
| |
| | |
| === Chest findings ===
| |
| * [[Gynecomastia]]: due to increased estradiol levels
| |
| * Loss of chest or [[Underarm hair|axillary hair]]
| |
| ===Other findings===
| |
| * [[Hemorrhoids]]
| |
| * [[Hematemesis]]
| |
| * [[Melena]]
| |
| | |
| ==History==
| |
| | |
| === Psychosocial history ===
| |
| *Past history of abuse
| |
| | |
| === Past Medical history ===
| |
| *History of
| |
| | |
| === Menstrual history ===
| |
| *History of
| |
| | |
| === Family history ===
| |
| *[[Family history]] of:
| |
| **
| |
|
| |
|
| === Medication history ===
| |
| *History of [[medication]] use should be obtained as many [[:Category:Drugs|drugs]] such as [[Opioid|opioids]] cause [[constipation]] as a side effect.
| |
|
| |
|
| ===Causes=== | | ===Pathophysiology prev=== |
| {| class="wikitable"
| | <div style="-webkit-user-select: none;"> |
| ! style="background:#4479BA; color: #FFFFFF;" align="center" + |Drugs and Toxins
| | {| class="infobox" style="position: fixed; top: 65%; right: 10px; margin: 0 0 0 0; border: 0; float: right;" |
| ! style="background:#4479BA; color: #FFFFFF;" align="center" + |Infections
| |
| ! style="background:#4479BA; color: #FFFFFF;" align="center" + |Autoimmune
| |
| ! style="background:#4479BA; color: #FFFFFF;" align="center" + |Metabolic
| |
| ! style="background:#4479BA; color: #FFFFFF;" align="center" + |Biliary obstruction(Secondary bilary cirrhosis)
| |
| ! style="background:#4479BA; color: #FFFFFF;" align="center" + |Vascular
| |
| ! style="background:#4479BA; color: #FFFFFF;" align="center" + |Miscellaneous
| |
| |- | | |- |
| |Alcohol | | | {{#ev:youtube|https://https://www.youtube.com/watch?v=5szNmKtyBW4|350}} |
| |Hepatitis B | |
| |Primary Biliary Cirrhosis | |
| |Wilson's disease
| |
| |Cystic fibrosis
| |
| |Chronic RHF
| |
| |Sarcoidosis
| |
| |- | | |- |
| |Methotrexate | | |} |
| |Hepatitis C
| | __NOTOC__ |
| |Autoimmune hepatitis
| | {{Cirrhosis}} |
| |Hemochromatosis
| | {{CMG}} {{AE}} |
| |Biliary atresia
| |
| |Budd-Chiari syndrome
| |
| |Intestinal
| |
|
| |
|
| bypass operations for obesity
| | |
| | ===Pathophysiology prev=== |
| | <div style="-webkit-user-select: none;"> |
| | {| class="infobox" style="position: fixed; top: 65%; right: 10px; margin: 0 0 0 0; border: 0; float: right;" |
| |- | | |- |
| |Isoniazid | | | {{#ev:youtube|https://https://www.youtube.com/watch?v=5szNmKtyBW4|350}} |
| |Schistosoma japonicum | |
| |Primary Sclerosing Cholangitis
| |
| |Alpha-1 antitrypsin deficiency
| |
| |Bile duct strictures
| |
| |Veno-occlusive disease
| |
| |Cryptogenic: unknown | |
| |- | | |- |
| |Methyldopa
| |
| |
| |
| |
| |
| |Porphyria
| |
| |Gallstones
| |
| |
| |
| |
| |
| |-
| |
| |
| |
| |
| |
| |
| |
| |Glycogen storage diseases (such as Galactosaemia, Abetalipoproteinaemia)
| |
| |
| |
| |
| |
| |
| |
| |} | | |} |
| | __NOTOC__ |
| | {{Cirrhosis}} |
| | {{CMG}} {{AE}} |
|
| |
|
| ===Cirrhosis=== | | == History and Symptoms == |
|
| |
|
| Pathophysiology <ref name="pmid7932316">{{cite journal |vauthors=Arthur MJ, Iredale JP |title=Hepatic lipocytes, TIMP-1 and liver fibrosis |journal=J R Coll Physicians Lond |volume=28 |issue=3 |pages=200–8 |year=1994 |pmid=7932316 |doi= |url=}}</ref><ref name="pmid8502273">{{cite journal |vauthors=Friedman SL |title=Seminars in medicine of the Beth Israel Hospital, Boston. The cellular basis of hepatic fibrosis. Mechanisms and treatment strategies |journal=N. Engl. J. Med. |volume=328 |issue=25 |pages=1828–35 |year=1993 |pmid=8502273 |doi=10.1056/NEJM199306243282508 |url=}}</ref><ref name="pmid8682489">{{cite journal |vauthors=Iredale JP |title=Matrix turnover in fibrogenesis |journal=Hepatogastroenterology |volume=43 |issue=7 |pages=56–71 |year=1996 |pmid=8682489 |doi= |url=}}</ref><ref name="pmid7959178">{{cite journal |vauthors=Gressner AM |title=Perisinusoidal lipocytes and fibrogenesis |journal=Gut |volume=35 |issue=10 |pages=1331–3 |year=1994 |pmid=7959178 |pmc=1374996 |doi= |url=}}</ref><ref name="pmid17332881">{{cite journal |vauthors=Iredale JP |title=Models of liver fibrosis: exploring the dynamic nature of inflammation and repair in a solid organ |journal=J. Clin. Invest. |volume=117 |issue=3 |pages=539–48 |year=2007 |pmid=17332881 |pmc=1804370 |doi=10.1172/JCI30542 |url=}}</ref><ref name="pmid11984538">{{cite journal |vauthors=Arthur MJ |title=Reversibility of liver fibrosis and cirrhosis following treatment for hepatitis C |journal=Gastroenterology |volume=122 |issue=5 |pages=1525–8 |year=2002 |pmid=11984538 |doi= |url=}}</ref>
| | * History should include: |
| * When an injured issue is replaced by a collagenous scar, it is termed as fibrosis.
| | ** Appearance of bowel movements |
| * When fibrosis of the liver reaches an advanced stage where distortion of the hepatic vasculature also occurs, it is termed as cirrhosis of the liver.
| | ** Travel history |
| * The cellular mechanisms responsible for cirrhosis are similar regardless of the type of initial insult and site of injury within the liver lobule.
| | ** Associated symptoms |
| * Viral hepatitis involves the periportal region, whereas involvement in alcoholic liver disease is largely pericentral.
| | ** Immune status |
| * If the damage progresses, panlobular cirrhosis may result.
| | ** Woodland exposure |
| * Cirrhosis involves the following steps: <ref name="pmid7737629">{{cite journal |vauthors=Wanless IR, Wong F, Blendis LM, Greig P, Heathcote EJ, Levy G |title=Hepatic and portal vein thrombosis in cirrhosis: possible role in development of parenchymal extinction and portal hypertension |journal=Hepatology |volume=21 |issue=5 |pages=1238–47 |year=1995 |pmid=7737629 |doi= |url=}}</ref> | | ==References== |
| ** Inflammation | | {{reflist|2}} |
| ** Hepatic stellate cell activation
| |
| ** Angiogenesis
| |
| ** Fibrogenesis
| |
| * Kupffer cells are hepatic macrophages responsible for Hepatic Stellate cell activation during injury.
| |
| * The hepatic stellate cell (also known as the perisinusoidal cell or Ito cell) plays a key role in the pathogenesis of liver fibrosis/cirrhosis.
| |
| * Hepatic stellate cells(HSC) are usually located in the subendothelial space of Disse and become activated to a myofibroblast-like phenotype in areas of liver injury. | |
| * Collagen and non collagenous matrix proteins responsible for fibrosis are produced by the activated Hepatic Stellate Cells(HSC). | |
| * Hepatocyte damage causes the release of lipid peroxidases from injured cell membranes leading to necrosis of parenchymal cells. | |
| * Activated HSC produce numerous cytokines and their receptors, such as PDGF and TGF-f31 which are responsible for fibrogenesis. | |
| * The matrix formed due to HSC activation is deposited in the space of Disse and leads to loss of fenestrations of endothelial cells, which is a process called capillarization. | |
| * Cirrhosis leads to hepatic microvascular changes characterised by <ref name="pmid19157625">{{cite journal |vauthors=Fernández M, Semela D, Bruix J, Colle I, Pinzani M, Bosch J |title=Angiogenesis in liver disease |journal=J. Hepatol. |volume=50 |issue=3 |pages=604–20 |year=2009 |pmid=19157625 |doi=10.1016/j.jhep.2008.12.011 |url=}}</ref> | |
| ** formation of intra hepatic shunts (due to angiogenesis and loss of parenchymal cells)
| |
| ** hepatic endothelial dysfunction | |
| * The endothelial dysfunction is characterised by <ref name="pmid22504334">{{cite journal |vauthors=García-Pagán JC, Gracia-Sancho J, Bosch J |title=Functional aspects on the pathophysiology of portal hypertension in cirrhosis |journal=J. Hepatol. |volume=57 |issue=2 |pages=458–61 |year=2012 |pmid=22504334 |doi=10.1016/j.jhep.2012.03.007 |url=}}</ref>
| |
| ** insufficient release of vasodilators, such as nitric oxide due to oxidative stress
| |
| ** increased production of vasoconstrictors (mainly adrenergic stimulation and activation of endothelins and RAAS)
| |
| * Fibrosis eventually leads to formation of septae that grossly distort the liver architecture which includes both the liver parenchyma and the vasculature. A cirrhotic liver compromises hepatic sinusoidal exchange by shunting arterial and portal blood directly into the central veins (hepatic outflow). Vascularized fibrous septa connect central veins with portal tracts leading to islands of hepatocytes surrounded by fibrous bands without central veins.<ref name="pmid18328931">{{cite journal |vauthors=Schuppan D, Afdhal NH |title=Liver cirrhosis |journal=Lancet |volume=371 |issue=9615 |pages=838–51 |year=2008 |pmid=18328931 |pmc=2271178 |doi=10.1016/S0140-6736(08)60383-9 |url=}}</ref><ref name="pmid15094237">{{cite journal |vauthors=Desmet VJ, Roskams T |title=Cirrhosis reversal: a duel between dogma and myth |journal=J. Hepatol. |volume=40 |issue=5 |pages=860–7 |year=2004 |pmid=15094237 |doi=10.1016/j.jhep.2004.03.007 |url=}}</ref><ref name="pmid11079009">{{cite journal |vauthors=Wanless IR, Nakashima E, Sherman M |title=Regression of human cirrhosis. Morphologic features and the genesis of incomplete septal cirrhosis |journal=Arch. Pathol. Lab. Med. |volume=124 |issue=11 |pages=1599–607 |year=2000 |pmid=11079009 |doi=10.1043/0003-9985(2000)124<1599:ROHC>2.0.CO;2 |url=}}</ref>
| |
| * The formation of fibrotic bands is accompanied by regenerative nodule formation in the hepatic parenchyma.
| |
| * Advancement of cirrhosis may lead to parenchymal dysfunction and development of portal hypertension.
| |
| * Portal HTN results from the combination of the following:
| |
| ** Structural disturbances associated with advanced liver disease account for 70% of total hepatic vascular resistance.
| |
| ** Functional abnormalities such as endothelial dysfunction and increased hepatic vascular tone account for 30% of total hepatic vascular resistance.
| |
|
| |
|
| Pathogenesis of Cirrhosis due to Alcohol:
| | {{WH}} |
| * More than 66 percent of all American adults consume alcohol.
| | {{WS}} |
| * Cirrhosis due to alcohol accounts for approximately forty percent of mortality rates due to cirrhosis.
| | |
| * Mechanisms of alcohol-induced damage include:
| | ==Other Imaging Findings== |
| ** Impaired protein synthesis, secretion, glycosylation
| | * [[Endoscopy]] |
| * Ethanol intake leads to elevated accumulation of intracellular triglycerides by:
| | * [[Barium enema]] |
| ** Lipoprotein secretion
| | * [[Colonoscopy]] |
| ** Decreased fatty acid oxidation
| | * [[Sigmoidoscopy]] |
| ** Increased fatty acid uptake
| | |
| * Alcohol is converted by Alcohol dehydrogenase to acetaldehyde. | | ==Other diagnostic studies== |
| * Due to the high reactivity of acetaldehyde, it forms acetaldehyde-protein adducts which cause damage to cells by: | | == Other Diagnostic Studies == |
| ** Trafficking of hepatic proteins | |
| ** Interrupting microtubule formation | |
| ** Interfering with enzyme activities
| |
| * Damage of hepatocytes leads to the formation of reactive oxygen species that activate Kupffer cells.<ref name="pmid11984538">{{cite journal |vauthors=Arthur MJ |title=Reversibility of liver fibrosis and cirrhosis following treatment for hepatitis C |journal=Gastroenterology |volume=122 |issue=5 |pages=1525–8 |year=2002 |pmid=11984538 |doi= |url=}}</ref>
| |
| *Kupffer cell activation leads to the production of profibrogenic cytokines that stimulates stellate cells.
| |
| *Stellate cell activation leads to the production of extracellular matrix and collagen.
| |
| * Portal triads develop connections with central veins due to connective tissue formation in pericentral and periportal zones, leading to the formation of regenerative nodules.
| |
| * Shrinkage of the liver occurs over years due to repeated insults that lead to:
| |
| ** Loss of hepatocytes
| |
| ** Increased production and deposition of collagen
| |
|
| |
|
| | * Breath hydrogen test |
|
| |
|
| Pathology
| | * [[HIV test]]ing for those patients suspected of having HIV |
| * There are four stages of Cirrhosis as it progresses: | |
| ** Chronic nonsuppurative destructive cholangitis - inflammation and necrosis of portal tracts with lymphocyte infiltration leading to the destruction of the bile ducts.
| |
| ** Development of biliary stasis and fibrosis
| |
| *Periportal fibrosis progresses to bridging fibrosis
| |
| *Increased proliferation of smaller bile ductules leading to regenerative nodule formation.
| |
|
| |
|
| ===Classification=== | | == |
| __NOTOC__
| |
| {{Cirrhosis}}
| |
| {{CMG}} {{AE}} {{CP}}
| |
|
| |
|
| ==Overview== | | ==Overview== |
| Cirrhosis of the [[liver]] can be classified using two methods; classification based on [[etiology]], and classification based on [[morphology]]. Currently, classifying cirrhosis based on morphology is not used, as it requires an invasive procedure to examine the gross appearance of the liver, and it provides little diagnostic value. Classifying cirrhosis according to etiology is a more accepted form of classification, as it can be attained through non-invasive laboratory testing, and has a higher diagnostic value.
| |
|
| |
|
| ==Classification Based on Etiology== | | ==References== |
| Cirrhosis can be classified by its etiology. This is the most widely accepted method of [[classification]].
| | {{reflist|2}} |
| ===Alcoholic Cirrhosis===
| |
| This is the most common cause of cirrhosis, and is caused by continuous and prolonged [[alcohol abuse]]. The American Academy of Family Physicians estimate that 60-70 percent of all cases of cirrhosis are a result of [[alcohol abuse]].
| |
| ===Post-Necrotic Cirrhosis===
| |
| This type of cirrhosis occurs after a massive event causes liver [[cell death]]. [[Viral hepatitis]] is the most common cause for this type of cirrhosis. Agents that are [[toxic]] to the liver can also cause this type of cirrhosis, as well as certain types of [[carcinomas]].
| |
|
| |
|
| ===Biliary Cirrhosis===
| | {{WH}} |
| This type of cirrhosis results from any diseases that cause [[biliary obstruction]]. There is usually a blockage in the [[bile duct]] and there may also be [[inflammation]]. The excess [[bile]] in the liver causes tissue destruction. It commonly results in [[jaundice]].
| | {{WS}} |
| ===Cardiac Cirrhosis===
| |
| This type of cirrhosis is caused by [[congestive heart failure]] causing poor circulation of [[oxygenated blood]] to the liver. This results in liver cell death, and the subsequent replacement of dead cells by [[fibrous tissue]].
| |
| ===Genetic Disorder===
| |
| This is when the cirrhosis is caused by a [[genetic disorder]] such as [[hemochromatosis]], [[Wilson's disease]], or [[alpha-1 antitrypsin deficiency]].
| |
| ===Malnutrition===
| |
| This category contains cirrhosis caused by various forms of [[malnutrition]], particularly chronic starvation.
| |
|
| |
|
| ==Classification Based on Morphology== | | ===Pathophysiology prev=== |
| [[Cirrhosis]] has historically been classified upon the [[Nodule (medicine)|nodular]] morphology that is seen on upon the gross appearance of the [[liver]]. Accurate assessment of the [[liver]] morphology can only be obtained through [[surgery]], [[biopsy]], or [[autopsy]], therefore more recently, more non-invasive means of classifying and determining the causes of [[cirrhosis]] are used.
| | <div style="-webkit-user-select: none;"> |
| | | {| class="infobox" style="position: fixed; top: 65%; right: 10px; margin: 0 0 0 0; border: 0; float: right;" |
| {| class="wikitable" | |
| ! style="background:#4479BA; color: #FFFFFF;" |Micronodular
| |
| ! style="background:#4479BA; color: #FFFFFF;" |Macronodular
| |
| ! style="background:#4479BA; color: #FFFFFF;" |Mixed
| |
| |- | | |- |
| |Micronodular [[cirrhosis]] is characterized by [[Nodule (medicine)|nodules]] that are less than 3mm in diameter | | | {{#ev:youtube|https://https://www.youtube.com/watch?v=5szNmKtyBW4|350}} |
| |Macronodular [[cirrhosis]] is characterized by [[Nodule (medicine)|nodules]] that are more than 3mm in diameter
| |
| |Micronodular [[cirrhosis]] can often progress into macronodular [[Cirrhosis|cirrhosis.]] During this transformation, a mixed form of [[cirrhosis]] may be seen.<ref name="pmid6629323">{{cite journal| author=Fauerholdt L, Schlichting P, Christensen E, Poulsen H, Tygstrup N, Juhl E| title=Conversion of micronodular cirrhosis into macronodular cirrhosis. | journal=Hepatology | year= 1983 | volume= 3 | issue= 6 | pages= 928-31 | pmid=6629323 | doi= | pmc= | url=http://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=6629323 }} </ref>
| |
| |- | | |- |
| |Causes:
| |
| *[[Alcohol]]
| |
| *[[Hemochromatosis]]
| |
| *[[Cholestasis|Cholestatic]] causes of [[cirrhosis]]
| |
| *Hepatic venous outflow obstruction
| |
| *[[Nutrition|Nutritional]] causes of [[cirrhosis]]
| |
| |
| |
| Causes:
| |
| *Chronic [[viral hepatitis]]
| |
| *[[Hemochromatosis]]
| |
| *[[Wilson's disease]]
| |
| *Post-necrotic [[cirrhosis]]
| |
| |Mixed nodular [[cirrhosis]] is also seen in Indian childhood [[cirrhosis]]. <ref name="pmid47794">{{cite journal| author=Nayak NC, Ramalingaswami V| title=Indian childhood cirrhosis. | journal=Clin Gastroenterol | year= 1975 | volume= 4 | issue= 2 | pages= 333-49 | pmid=47794 | doi= | pmc= | url=http://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=47794 }} </ref>
| |
| |} | | |} |
| | __NOTOC__ |
| | {{Cirrhosis}} |
| | {{CMG}} {{AE}} |
|
| |
|
| ==Video codes== | | ==Video codes== |
| Line 1,032: |
Line 85: |
| ===Normal video=== | | ===Normal video=== |
| {{#ev:youtube|x6e9Pk6inYI}} | | {{#ev:youtube|x6e9Pk6inYI}} |
| | {{#ev:youtube|4uSSvD1BAHg}} |
| | {{#ev:youtube|PQXb5D-5UZw}} |
| | {{#ev:youtube|UVJYQlUm2A8}} |
|
| |
|
| ===Video in table=== | | ===Video in table=== |
| Line 1,063: |
Line 119: |
| ===Image and text to the right=== | | ===Image and text to the right=== |
|
| |
|
| <figure-inline><figure-inline><figure-inline><figure-inline><figure-inline><figure-inline><figure-inline><figure-inline><figure-inline>[[File:Global distribution of leptospirosis.jpg|577x577px]]</figure-inline></figure-inline></figure-inline></figure-inline></figure-inline></figure-inline></figure-inline></figure-inline></figure-inline> Recent out break of leptospirosis is reported in Bronx, New York and found 3 cases in the months January and February, 2017. | | <figure-inline><figure-inline><figure-inline><figure-inline><figure-inline><figure-inline><figure-inline><figure-inline><figure-inline><figure-inline><figure-inline><figure-inline><figure-inline><figure-inline><figure-inline><figure-inline><figure-inline><figure-inline><figure-inline><figure-inline><figure-inline><figure-inline><figure-inline><figure-inline><figure-inline><figure-inline><figure-inline>[[File:Global distribution of leptospirosis.jpg|577x577px]]</figure-inline></figure-inline></figure-inline></figure-inline></figure-inline></figure-inline></figure-inline></figure-inline></figure-inline></figure-inline></figure-inline></figure-inline></figure-inline></figure-inline></figure-inline></figure-inline></figure-inline></figure-inline></figure-inline></figure-inline></figure-inline></figure-inline></figure-inline></figure-inline></figure-inline></figure-inline></figure-inline> Recent out break of leptospirosis is reported in Bronx, New York and found 3 cases in the months January and February, 2017. |
|
| |
|
| ===Gallery=== | | ===Gallery=== |
| Line 1,078: |
Line 134: |
| ==References== | | ==References== |
| {{Reflist|2}} | | {{Reflist|2}} |
|
| |
| [[Category:Gastroenterology]]
| |
| [[Category:Hepatology]]
| |
| [[Category:Disease]]
| |
|
| |
| {{WS}} | | {{WS}} |
| {{WH}} | | {{WH}} |
| Line 1,089: |
Line 140: |
| REFERENCES | | REFERENCES |
| <references /> | | <references /> |
| | |
| | [[Category:Gastroenterology]] |
| | [[Category:Needs overview]] |
| | [[Category:Hepatology]] |
| | [[Category:Disease]] |
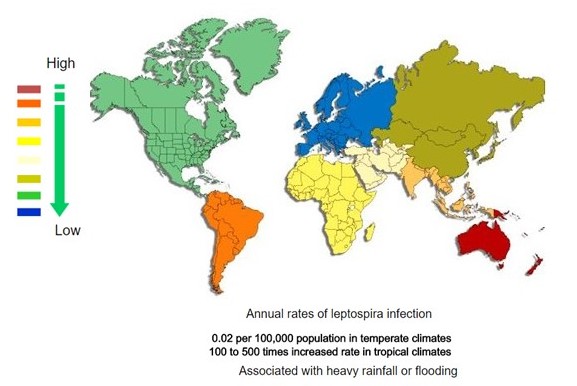 </figure-inline></figure-inline></figure-inline></figure-inline></figure-inline></figure-inline></figure-inline></figure-inline></figure-inline></figure-inline></figure-inline></figure-inline></figure-inline></figure-inline></figure-inline></figure-inline></figure-inline></figure-inline></figure-inline></figure-inline></figure-inline></figure-inline></figure-inline></figure-inline></figure-inline></figure-inline></figure-inline> Recent out break of leptospirosis is reported in Bronx, New York and found 3 cases in the months January and February, 2017.
</figure-inline></figure-inline></figure-inline></figure-inline></figure-inline></figure-inline></figure-inline></figure-inline></figure-inline></figure-inline></figure-inline></figure-inline></figure-inline></figure-inline></figure-inline></figure-inline></figure-inline></figure-inline></figure-inline></figure-inline></figure-inline></figure-inline></figure-inline></figure-inline></figure-inline></figure-inline></figure-inline> Recent out break of leptospirosis is reported in Bronx, New York and found 3 cases in the months January and February, 2017.
![Histopathology of a pancreatic endocrine tumor (insulinoma). Source:https://librepathology.org/wiki/Neuroendocrine_tumour_of_the_pancreas[1]](/images/2/2f/Pancreatic_insulinoma_histology_2.JPG)
![Histopathology of a pancreatic endocrine tumor (insulinoma). Chromogranin A immunostain. Source:https://librepathology.org/wiki/Neuroendocrine_tumour_of_the_pancreas[1]](/images/a/a3/Pancreatic_insulinoma_histopathology_3.JPG)
![Histopathology of a pancreatic endocrine tumor (insulinoma). Insulin immunostain. Source:https://librepathology.org/wiki/Neuroendocrine_tumour_of_the_pancreas[1]](/images/d/d5/Pancreatic_insulinoma_histology_4.JPG)