|
|
| (182 intermediate revisions by 3 users not shown) |
| Line 1: |
Line 1: |
| | ==Physical examination== |
| | ==References== |
| | {{reflist|2}} |
|
| |
|
| <font color="red">Cherry</font>
| | {{WH}} |
| | {{WS}} |
|
| |
|
| | ==References== |
| | {{Reflist|2}} |
|
| |
|
|
| |
|
| ==Physical Examination== | | ===Pathophysiology prev=== |
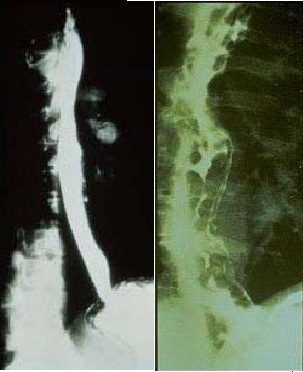
| [[Image: Normal versus Abnormal Barium study of esophagus.jpg|thumb|left|200px|Normal versus Abnormal Barium study of esophagus with varices]]
| | <div style="-webkit-user-select: none;"> |
| | | {| class="infobox" style="position: fixed; top: 65%; right: 10px; margin: 0 0 0 0; border: 0; float: right;" |
| | |
| ===GIF maker=== | |
| | |
| [[File:Cirrhosis baba gif.gif|500px|Right|thumb|Liver Cirhhosis <br> Source:Wikimedia commons<ref name="urlCategory:Histopathology of cirrhosis - Wikimedia Commons">{{cite web |url=https://commons.wikimedia.org/wiki/Category:Histopathology_of_cirrhosis#/media/File:Cirrhosis_high_mag.jpg |title=Category:Histopathology of cirrhosis - Wikimedia Commons |format= |work= |accessdate=}}</ref>]]
| |
| | |
| | |
| | |
| | |
| | |
| [[File:Spider angioma p.jpg|500px|center|thumb|Spider angiomata <br> Source:Wikimedia commons ]]
| |
| [[File:Output OBujt7.gif|500px|left|thumb|Spider angiomata <br> Source:Wikimedia commons]]
| |
| | |
| ===Eyes===
| |
| | |
| | |
| [[Image:Kayser-Fleischer ring.jpg|thumb|center|300px|A Kayser-Fleischer ring in a 32-year-old patient who had longstanding speech difficulties and [[tremor]].]]
| |
| | |
| [[Image:Muehrcke's lines.JPG|thumb|center|300px|Muehrcke's nails]]
| |
| | |
| | |
| | |
| ==Physical Examination==
| |
| | |
| *Physical examination of [[Patient|patients]] with [[cirrhosis]] is usually remarkable for: [[jaundice]], [[Spider angioma|spider angiomata]], [[ascites]], [[asterixis]], [[Splenomegaly|spleenomegaly]] and [[palmar erythema]].
| |
| | |
| ===Appearance of the Patient===
| |
| | |
| *[[Patient|Patients]] with [[cirrhosis]] usually appear weak due to constitutional [[Symptom|symptoms]] such as [[weight loss]], [[anorexia]] and [[muscle atrophy]]. Yellowish discoloration of [[skin]] and [[abdominal distension]] may also be present due to [[ascites]].
| |
| | |
| *Normal/low [[blood pressure]] with normal [[pulse pressure]].
| |
| | |
| ===Skin===
| |
| *[[Jaundice]] : yellow discoloration of the skin, eyes, and mucus membranes due to increased [[bilirubin]] (at least 2-3 mg/dL or 30 mmol/L). Urine may also appear dark.
| |
| *[[Pallor]]
| |
| *[[Bruise|Bruises]]
| |
| *[[Palmar erythema]] on the [[Thenar eminence|thenar]] and [[Hypothenar eminence|hypothenar eminences]], due to altered sex hormone metabolism.
| |
| *[[Spider angioma|Spider angiomata]]: Increased estradiol levels lead to the formation of vascular lesions consisting of central arterioles surrounded by smaller vessels <ref name="pmid10423070">{{cite journal |author=Li CP, Lee FY, Hwang SJ, ''et al'' |title=Spider angiomas in patients with liver cirrhosis: role of alcoholism and impaired liver function|journal=Scand. J. Gastroenterol. |volume=34 |issue=5 |pages=520-3 |year=1999 |pmid=10423070 |doi=}}</ref>
| |
| *'''[[Telangiectasia|Telangiectasias]]''' or '''spider veins:''' small dilated [[blood vessel]]s near the surface of the [[skin]].
| |
| | |
| ===HEENT===
| |
| * Abnormalities of the head/hair may include thinning of hair on the scalp due to [[hyperestrogenism]]
| |
| * '''[[Kayser-Fleischer ring]]s''' : dark rings that appear to encircle the [[iris (anatomy)|iris]] of the [[eye]] in [[Patient|patients]] with [[Wilson's disease]].
| |
| * [[Parotid gland]] enlargement
| |
| * [[Fetor hepaticus]]: severe portal-systemic shunting leads to increased levels of [[dimethyl sulfide]] leads to a sweet pungent smell in the breath
| |
| | |
| ===Abdomen===
| |
| * Inspection:
| |
| ** [[Abdominal distension]]
| |
| ** [[Caput medusae]]
| |
| | |
| * Palpation:
| |
| ** Fluid wave
| |
| ** [[Hepatomegaly]] may be present in initial stages. The liver may also be normal or shrunken.
| |
| ** [[Splenomegaly|Spleenomegaly]] may be present in patients with [[cirrhosis]] from nonalcoholic etiologies, due to portal hypertension
| |
| | |
| * Percussion:
| |
| ** Flank dullness may be present due to [[ascites]] (needs approximately 1500ml for detection)
| |
| | |
| * Auscultation:
| |
| ** [[Cruveilhier-Baumgarten murmur]]: venous hum that may be present in patients with [[portal hypertension]].
| |
| *** Mechanism: due to collateral connections between remnant of the [[umbilical vein]] and the [[Portal venous system|portal system]]
| |
| *** Location: [[Epigastrium]]
| |
| *** Exacerbating factors: [[Valsalva maneuver]]
| |
| *** Diminished by: application of [[pressure]] on the [[skin]] above the [[Navel|umbilicus]]
| |
| | |
| ===Genitourinary===
| |
| *[[Testicular atrophy]]
| |
| *Inversion of the normal male [[pubic hair]] pattern
| |
| ===Neuromuscular===
| |
| * [[Hepatic encephalopathy]] may have signs of:
| |
| ** Alteration of [[Mental status examination|mental status]]
| |
| ** [[Confusion]]
| |
| ** [[Coma]]
| |
| * [[Asterixis]] (bilateral but asynchronous flapping motions of outstretched, dorsiflexed hands) is seen in patients with [[hepatic encephalopathy]].
| |
| | |
| ===Extremities===
| |
| *[[edema]] of the lower extremities
| |
| *[[Muscle atrophy]]
| |
| *Nail changes:
| |
| **Muehrcke nails: paired horizontal white bands separated by normal color due to [[hypoalbuminemia]]
| |
| **Terry nails: the proximal two-thirds of the nail plate appears white, whereas the distal one-third is red due to [[hypoalbuminemia]]
| |
| ** [[Clubbing]]: the angle between the nail plate and proximal nail fold is greater than 180 degrees
| |
| **Severe [[clubbing]]:
| |
| ***"Drum stick" appearance of distal fingers
| |
| ***[[Hypertrophic pulmonary osteoarthropathy|Hypertrophic osteoarthropathy]]: chronic proliferative [[periostitis]] of the [[long bones]]
| |
| **[[Dupuytrens contracture|Dupuytren's contracture]] may cause flexion deformities of the fingers: This occurs due to shortening and thickening of the palmar fascia, due to collagen deposition and fibroblastic proliferation.
| |
| **[[Asterixis]] in cases with [[hepatic encephalopathy]]
| |
| | |
| === Chest findings ===
| |
| * [[Gynecomastia]]: due to increased estradiol levels
| |
| * Loss of chest or [[Underarm hair|axillary hair]]
| |
| ===Other findings===
| |
| * [[Hemorrhoids]]
| |
| * [[Hematemesis]]
| |
| * [[Melena]]
| |
| | |
| ==History==
| |
| | |
| === Psychosocial history ===
| |
| *Past history of abuse
| |
| | |
| === Past Medical history ===
| |
| *History of
| |
| | |
| === Menstrual history ===
| |
| *History of
| |
| | |
| === Family history ===
| |
| *[[Family history]] of:
| |
| **
| |
| | |
| === Medication history ===
| |
| *History of [[medication]] use should be obtained as many [[:Category:Drugs|drugs]] such as [[Opioid|opioids]] cause [[constipation]] as a side effect.
| |
| | |
| ===Causes===
| |
| {| class="wikitable" | |
| ! style="background:#4479BA; color: #FFFFFF;" align="center" + |Drugs and Toxins
| |
| ! style="background:#4479BA; color: #FFFFFF;" align="center" + |Infections
| |
| ! style="background:#4479BA; color: #FFFFFF;" align="center" + |Autoimmune
| |
| ! style="background:#4479BA; color: #FFFFFF;" align="center" + |Metabolic
| |
| ! style="background:#4479BA; color: #FFFFFF;" align="center" + |Biliary obstruction(Secondary bilary cirrhosis)
| |
| ! style="background:#4479BA; color: #FFFFFF;" align="center" + |Vascular
| |
| ! style="background:#4479BA; color: #FFFFFF;" align="center" + |Miscellaneous
| |
| |- | | |- |
| |Alcohol | | | {{#ev:youtube|https://https://www.youtube.com/watch?v=5szNmKtyBW4|350}} |
| |Hepatitis B | |
| |Primary Biliary Cirrhosis | |
| |Wilson's disease
| |
| |Cystic fibrosis
| |
| |Chronic RHF
| |
| |Sarcoidosis
| |
| |- | | |- |
| |Methotrexate | | |} |
| |Hepatitis C
| | __NOTOC__ |
| |Autoimmune hepatitis
| | {{Cirrhosis}} |
| |Hemochromatosis
| | {{CMG}} {{AE}} |
| |Biliary atresia
| | |
| |Budd-Chiari syndrome
| |
| |Intestinal
| |
|
| |
|
| bypass operations for obesity
| | ===Pathophysiology prev=== |
| |-
| | <div style="-webkit-user-select: none;"> |
| |Isoniazid
| | {| class="infobox" style="position: fixed; top: 65%; right: 10px; margin: 0 0 0 0; border: 0; float: right;" |
| |Schistosoma japonicum
| |
| |Primary Sclerosing Cholangitis
| |
| |Alpha-1 antitrypsin deficiency
| |
| |Bile duct strictures
| |
| |Veno-occlusive disease
| |
| |Cryptogenic: unknown | |
| |- | | |- |
| |Methyldopa | | | {{#ev:youtube|https://https://www.youtube.com/watch?v=5szNmKtyBW4|350}} |
| | | |
| |
| |
| |Porphyria
| |
| |Gallstones
| |
| |
| |
| | | |
| |- | | |- |
| |
| |
| |
| |
| |
| |
| |Glycogen storage diseases (such as Galactosaemia, Abetalipoproteinaemia)
| |
| |
| |
| |
| |
| |
| |
| |} | | |} |
| | __NOTOC__ |
| | {{Cirrhosis}} |
| | {{CMG}} {{AE}} |
|
| |
|
| ===Cirrhosis=== | | == History and Symptoms == |
|
| |
|
| Pathophysiology <ref name="pmid7932316">{{cite journal |vauthors=Arthur MJ, Iredale JP |title=Hepatic lipocytes, TIMP-1 and liver fibrosis |journal=J R Coll Physicians Lond |volume=28 |issue=3 |pages=200–8 |year=1994 |pmid=7932316 |doi= |url=}}</ref><ref name="pmid8502273">{{cite journal |vauthors=Friedman SL |title=Seminars in medicine of the Beth Israel Hospital, Boston. The cellular basis of hepatic fibrosis. Mechanisms and treatment strategies |journal=N. Engl. J. Med. |volume=328 |issue=25 |pages=1828–35 |year=1993 |pmid=8502273 |doi=10.1056/NEJM199306243282508 |url=}}</ref><ref name="pmid8682489">{{cite journal |vauthors=Iredale JP |title=Matrix turnover in fibrogenesis |journal=Hepatogastroenterology |volume=43 |issue=7 |pages=56–71 |year=1996 |pmid=8682489 |doi= |url=}}</ref><ref name="pmid7959178">{{cite journal |vauthors=Gressner AM |title=Perisinusoidal lipocytes and fibrogenesis |journal=Gut |volume=35 |issue=10 |pages=1331–3 |year=1994 |pmid=7959178 |pmc=1374996 |doi= |url=}}</ref><ref name="pmid17332881">{{cite journal |vauthors=Iredale JP |title=Models of liver fibrosis: exploring the dynamic nature of inflammation and repair in a solid organ |journal=J. Clin. Invest. |volume=117 |issue=3 |pages=539–48 |year=2007 |pmid=17332881 |pmc=1804370 |doi=10.1172/JCI30542 |url=}}</ref><ref name="pmid11984538">{{cite journal |vauthors=Arthur MJ |title=Reversibility of liver fibrosis and cirrhosis following treatment for hepatitis C |journal=Gastroenterology |volume=122 |issue=5 |pages=1525–8 |year=2002 |pmid=11984538 |doi= |url=}}</ref>
| | * History should include: |
| * When an injured issue is replaced by a collagenous scar, it is termed as fibrosis.
| | ** Appearance of bowel movements |
| * When fibrosis of the liver reaches an advanced stage where distortion of the hepatic vasculature also occurs, it is termed as cirrhosis of the liver.
| | ** Travel history |
| * The cellular mechanisms responsible for cirrhosis are similar regardless of the type of initial insult and site of injury within the liver lobule.
| | ** Associated symptoms |
| * Viral hepatitis involves the periportal region, whereas involvement in alcoholic liver disease is largely pericentral.
| | ** Immune status |
| * If the damage progresses, panlobular cirrhosis may result.
| | ** Woodland exposure |
| * Cirrhosis involves the following steps: <ref name="pmid7737629">{{cite journal |vauthors=Wanless IR, Wong F, Blendis LM, Greig P, Heathcote EJ, Levy G |title=Hepatic and portal vein thrombosis in cirrhosis: possible role in development of parenchymal extinction and portal hypertension |journal=Hepatology |volume=21 |issue=5 |pages=1238–47 |year=1995 |pmid=7737629 |doi= |url=}}</ref> | | ==References== |
| ** Inflammation | | {{reflist|2}} |
| ** Hepatic stellate cell activation
| |
| ** Angiogenesis
| |
| ** Fibrogenesis
| |
| * Kupffer cells are hepatic macrophages responsible for Hepatic Stellate cell activation during injury.
| |
| * The hepatic stellate cell (also known as the perisinusoidal cell or Ito cell) plays a key role in the pathogenesis of liver fibrosis/cirrhosis.
| |
| * Hepatic stellate cells(HSC) are usually located in the subendothelial space of Disse and become activated to a myofibroblast-like phenotype in areas of liver injury. | |
| * Collagen and non collagenous matrix proteins responsible for fibrosis are produced by the activated Hepatic Stellate Cells(HSC). | |
| * Hepatocyte damage causes the release of lipid peroxidases from injured cell membranes leading to necrosis of parenchymal cells. | |
| * Activated HSC produce numerous cytokines and their receptors, such as PDGF and TGF-f31 which are responsible for fibrogenesis. | |
| * The matrix formed due to HSC activation is deposited in the space of Disse and leads to loss of fenestrations of endothelial cells, which is a process called capillarization. | |
| * Cirrhosis leads to hepatic microvascular changes characterised by <ref name="pmid19157625">{{cite journal |vauthors=Fernández M, Semela D, Bruix J, Colle I, Pinzani M, Bosch J |title=Angiogenesis in liver disease |journal=J. Hepatol. |volume=50 |issue=3 |pages=604–20 |year=2009 |pmid=19157625 |doi=10.1016/j.jhep.2008.12.011 |url=}}</ref> | |
| ** formation of intra hepatic shunts (due to angiogenesis and loss of parenchymal cells)
| |
| ** hepatic endothelial dysfunction | |
| * The endothelial dysfunction is characterised by <ref name="pmid22504334">{{cite journal |vauthors=García-Pagán JC, Gracia-Sancho J, Bosch J |title=Functional aspects on the pathophysiology of portal hypertension in cirrhosis |journal=J. Hepatol. |volume=57 |issue=2 |pages=458–61 |year=2012 |pmid=22504334 |doi=10.1016/j.jhep.2012.03.007 |url=}}</ref>
| |
| ** insufficient release of vasodilators, such as nitric oxide due to oxidative stress
| |
| ** increased production of vasoconstrictors (mainly adrenergic stimulation and activation of endothelins and RAAS)
| |
| * Fibrosis eventually leads to formation of septae that grossly distort the liver architecture which includes both the liver parenchyma and the vasculature. A cirrhotic liver compromises hepatic sinusoidal exchange by shunting arterial and portal blood directly into the central veins (hepatic outflow). Vascularized fibrous septa connect central veins with portal tracts leading to islands of hepatocytes surrounded by fibrous bands without central veins.<ref name="pmid18328931">{{cite journal |vauthors=Schuppan D, Afdhal NH |title=Liver cirrhosis |journal=Lancet |volume=371 |issue=9615 |pages=838–51 |year=2008 |pmid=18328931 |pmc=2271178 |doi=10.1016/S0140-6736(08)60383-9 |url=}}</ref><ref name="pmid15094237">{{cite journal |vauthors=Desmet VJ, Roskams T |title=Cirrhosis reversal: a duel between dogma and myth |journal=J. Hepatol. |volume=40 |issue=5 |pages=860–7 |year=2004 |pmid=15094237 |doi=10.1016/j.jhep.2004.03.007 |url=}}</ref><ref name="pmid11079009">{{cite journal |vauthors=Wanless IR, Nakashima E, Sherman M |title=Regression of human cirrhosis. Morphologic features and the genesis of incomplete septal cirrhosis |journal=Arch. Pathol. Lab. Med. |volume=124 |issue=11 |pages=1599–607 |year=2000 |pmid=11079009 |doi=10.1043/0003-9985(2000)124<1599:ROHC>2.0.CO;2 |url=}}</ref>
| |
| * The formation of fibrotic bands is accompanied by regenerative nodule formation in the hepatic parenchyma.
| |
| * Advancement of cirrhosis may lead to parenchymal dysfunction and development of portal hypertension.
| |
| * Portal HTN results from the combination of the following:
| |
| ** Structural disturbances associated with advanced liver disease account for 70% of total hepatic vascular resistance.
| |
| ** Functional abnormalities such as endothelial dysfunction and increased hepatic vascular tone account for 30% of total hepatic vascular resistance.
| |
|
| |
|
| Pathogenesis of Cirrhosis due to Alcohol:
| | {{WH}} |
| * More than 66 percent of all American adults consume alcohol.
| | {{WS}} |
| * Cirrhosis due to alcohol accounts for approximately forty percent of mortality rates due to cirrhosis.
| | |
| * Mechanisms of alcohol-induced damage include:
| | ==Other Imaging Findings== |
| ** Impaired protein synthesis, secretion, glycosylation
| | * [[Endoscopy]] |
| * Ethanol intake leads to elevated accumulation of intracellular triglycerides by:
| | * [[Barium enema]] |
| ** Lipoprotein secretion
| | * [[Colonoscopy]] |
| ** Decreased fatty acid oxidation
| | * [[Sigmoidoscopy]] |
| ** Increased fatty acid uptake
| | |
| * Alcohol is converted by Alcohol dehydrogenase to acetaldehyde. | | ==Other diagnostic studies== |
| * Due to the high reactivity of acetaldehyde, it forms acetaldehyde-protein adducts which cause damage to cells by: | | == Other Diagnostic Studies == |
| ** Trafficking of hepatic proteins | |
| ** Interrupting microtubule formation | |
| ** Interfering with enzyme activities
| |
| * Damage of hepatocytes leads to the formation of reactive oxygen species that activate Kupffer cells.<ref name="pmid11984538">{{cite journal |vauthors=Arthur MJ |title=Reversibility of liver fibrosis and cirrhosis following treatment for hepatitis C |journal=Gastroenterology |volume=122 |issue=5 |pages=1525–8 |year=2002 |pmid=11984538 |doi= |url=}}</ref>
| |
| *Kupffer cell activation leads to the production of profibrogenic cytokines that stimulates stellate cells.
| |
| *Stellate cell activation leads to the production of extracellular matrix and collagen.
| |
| * Portal triads develop connections with central veins due to connective tissue formation in pericentral and periportal zones, leading to the formation of regenerative nodules.
| |
| * Shrinkage of the liver occurs over years due to repeated insults that lead to:
| |
| ** Loss of hepatocytes
| |
| ** Increased production and deposition of collagen
| |
|
| |
|
| | * Breath hydrogen test |
|
| |
|
| Pathology
| | * [[HIV test]]ing for those patients suspected of having HIV |
| * There are four stages of Cirrhosis as it progresses: | |
| ** Chronic nonsuppurative destructive cholangitis - inflammation and necrosis of portal tracts with lymphocyte infiltration leading to the destruction of the bile ducts.
| |
| ** Development of biliary stasis and fibrosis
| |
| *Periportal fibrosis progresses to bridging fibrosis
| |
| *Increased proliferation of smaller bile ductules leading to regenerative nodule formation.
| |
|
| |
|
| ===Classification=== | | == |
| __NOTOC__
| |
| {{Cirrhosis}}
| |
| {{CMG}} {{AE}} {{CP}}
| |
|
| |
|
| ==Overview== | | ==Overview== |
| Cirrhosis of the [[liver]] can be classified using two methods; classification based on [[etiology]], and classification based on [[morphology]]. Currently, classifying cirrhosis based on morphology is not used, as it requires an invasive procedure to examine the gross appearance of the liver, and it provides little diagnostic value. Classifying cirrhosis according to etiology is a more accepted form of classification, as it can be attained through non-invasive laboratory testing, and has a higher diagnostic value.
| |
|
| |
|
| ==Classification Based on Etiology== | | ==References== |
| Cirrhosis can be classified by its etiology. This is the most widely accepted method of [[classification]].
| | {{reflist|2}} |
| ===Alcoholic Cirrhosis===
| |
| This is the most common cause of cirrhosis, and is caused by continuous and prolonged [[alcohol abuse]]. The American Academy of Family Physicians estimate that 60-70 percent of all cases of cirrhosis are a result of [[alcohol abuse]].
| |
| ===Post-Necrotic Cirrhosis===
| |
| This type of cirrhosis occurs after a massive event causes liver [[cell death]]. [[Viral hepatitis]] is the most common cause for this type of cirrhosis. Agents that are [[toxic]] to the liver can also cause this type of cirrhosis, as well as certain types of [[carcinomas]].
| |
|
| |
|
| ===Biliary Cirrhosis===
| | {{WH}} |
| This type of cirrhosis results from any diseases that cause [[biliary obstruction]]. There is usually a blockage in the [[bile duct]] and there may also be [[inflammation]]. The excess [[bile]] in the liver causes tissue destruction. It commonly results in [[jaundice]].
| | {{WS}} |
| ===Cardiac Cirrhosis===
| |
| This type of cirrhosis is caused by [[congestive heart failure]] causing poor circulation of [[oxygenated blood]] to the liver. This results in liver cell death, and the subsequent replacement of dead cells by [[fibrous tissue]].
| |
| ===Genetic Disorder===
| |
| This is when the cirrhosis is caused by a [[genetic disorder]] such as [[hemochromatosis]], [[Wilson's disease]], or [[alpha-1 antitrypsin deficiency]].
| |
| ===Malnutrition===
| |
| This category contains cirrhosis caused by various forms of [[malnutrition]], particularly chronic starvation.
| |
|
| |
|
| ==Classification Based on Morphology== | | ===Pathophysiology prev=== |
| [[Cirrhosis]] has historically been classified upon the [[Nodule (medicine)|nodular]] morphology that is seen on upon the gross appearance of the [[liver]]. Accurate assessment of the [[liver]] morphology can only be obtained through [[surgery]], [[biopsy]], or [[autopsy]], therefore more recently, more non-invasive means of classifying and determining the causes of [[cirrhosis]] are used.
| | <div style="-webkit-user-select: none;"> |
| | | {| class="infobox" style="position: fixed; top: 65%; right: 10px; margin: 0 0 0 0; border: 0; float: right;" |
| {| class="wikitable" | |
| ! style="background:#4479BA; color: #FFFFFF;" |Micronodular
| |
| ! style="background:#4479BA; color: #FFFFFF;" |Macronodular
| |
| ! style="background:#4479BA; color: #FFFFFF;" |Mixed
| |
| |- | | |- |
| |Micronodular [[cirrhosis]] is characterized by [[Nodule (medicine)|nodules]] that are less than 3mm in diameter | | | {{#ev:youtube|https://https://www.youtube.com/watch?v=5szNmKtyBW4|350}} |
| |Macronodular [[cirrhosis]] is characterized by [[Nodule (medicine)|nodules]] that are more than 3mm in diameter
| |
| |Micronodular [[cirrhosis]] can often progress into macronodular [[Cirrhosis|cirrhosis.]] During this transformation, a mixed form of [[cirrhosis]] may be seen.<ref name="pmid6629323">{{cite journal| author=Fauerholdt L, Schlichting P, Christensen E, Poulsen H, Tygstrup N, Juhl E| title=Conversion of micronodular cirrhosis into macronodular cirrhosis. | journal=Hepatology | year= 1983 | volume= 3 | issue= 6 | pages= 928-31 | pmid=6629323 | doi= | pmc= | url=http://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=6629323 }} </ref>
| |
| |- | | |- |
| |Causes:
| |
| *[[Alcohol]]
| |
| *[[Hemochromatosis]]
| |
| *[[Cholestasis|Cholestatic]] causes of [[cirrhosis]]
| |
| *Hepatic venous outflow obstruction
| |
| *[[Nutrition|Nutritional]] causes of [[cirrhosis]]
| |
| |
| |
| Causes:
| |
| *Chronic [[viral hepatitis]]
| |
| *[[Hemochromatosis]]
| |
| *[[Wilson's disease]]
| |
| *Post-necrotic [[cirrhosis]]
| |
| |Mixed nodular [[cirrhosis]] is also seen in Indian childhood [[cirrhosis]]. <ref name="pmid47794">{{cite journal| author=Nayak NC, Ramalingaswami V| title=Indian childhood cirrhosis. | journal=Clin Gastroenterol | year= 1975 | volume= 4 | issue= 2 | pages= 333-49 | pmid=47794 | doi= | pmc= | url=http://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=47794 }} </ref>
| |
| |} | | |} |
| | __NOTOC__ |
| | {{Cirrhosis}} |
| | {{CMG}} {{AE}} |
|
| |
|
| ==Video codes== | | ==Video codes== |
| Line 292: |
Line 85: |
| ===Normal video=== | | ===Normal video=== |
| {{#ev:youtube|x6e9Pk6inYI}} | | {{#ev:youtube|x6e9Pk6inYI}} |
| | {{#ev:youtube|4uSSvD1BAHg}} |
| | {{#ev:youtube|PQXb5D-5UZw}} |
| | {{#ev:youtube|UVJYQlUm2A8}} |
|
| |
|
| ===Video in table=== | | ===Video in table=== |
| Line 305: |
Line 101: |
| |- | | |- |
| |} | | |} |
|
| |
|
| |
|
| ===Redirect=== | | ===Redirect=== |
| Line 324: |
Line 119: |
| ===Image and text to the right=== | | ===Image and text to the right=== |
|
| |
|
| [[File:Global distribution of leptospirosis.jpg|500px]] Recent out break of leptospirosis is reported in Bronx, New York and found 3 cases in the months January and February, 2017. | | <figure-inline><figure-inline><figure-inline><figure-inline><figure-inline><figure-inline><figure-inline><figure-inline><figure-inline><figure-inline><figure-inline><figure-inline><figure-inline><figure-inline><figure-inline><figure-inline><figure-inline><figure-inline><figure-inline><figure-inline><figure-inline><figure-inline><figure-inline><figure-inline><figure-inline><figure-inline><figure-inline>[[File:Global distribution of leptospirosis.jpg|577x577px]]</figure-inline></figure-inline></figure-inline></figure-inline></figure-inline></figure-inline></figure-inline></figure-inline></figure-inline></figure-inline></figure-inline></figure-inline></figure-inline></figure-inline></figure-inline></figure-inline></figure-inline></figure-inline></figure-inline></figure-inline></figure-inline></figure-inline></figure-inline></figure-inline></figure-inline></figure-inline></figure-inline> Recent out break of leptospirosis is reported in Bronx, New York and found 3 cases in the months January and February, 2017. |
|
| |
|
| ===Gallery=== | | ===Gallery=== |
| Line 339: |
Line 134: |
| ==References== | | ==References== |
| {{Reflist|2}} | | {{Reflist|2}} |
|
| |
| [[Category:Gastroenterology]]
| |
| [[Category:Hepatology]]
| |
| [[Category:Disease]]
| |
|
| |
| {{WS}} | | {{WS}} |
| {{WH}} | | {{WH}} |
| Line 350: |
Line 140: |
| REFERENCES | | REFERENCES |
| <references /> | | <references /> |
| | |
| | [[Category:Gastroenterology]] |
| | [[Category:Needs overview]] |
| | [[Category:Hepatology]] |
| | [[Category:Disease]] |
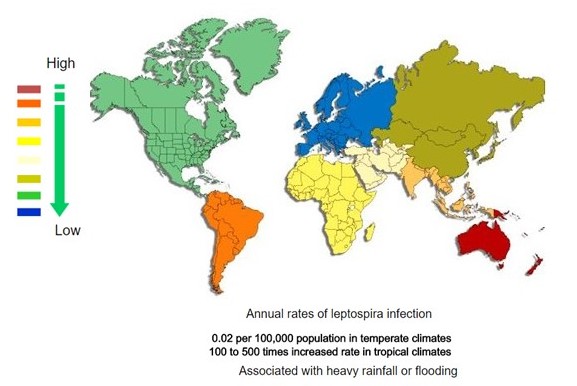 </figure-inline></figure-inline></figure-inline></figure-inline></figure-inline></figure-inline></figure-inline></figure-inline></figure-inline></figure-inline></figure-inline></figure-inline></figure-inline></figure-inline></figure-inline></figure-inline></figure-inline></figure-inline></figure-inline></figure-inline></figure-inline></figure-inline></figure-inline></figure-inline></figure-inline></figure-inline></figure-inline> Recent out break of leptospirosis is reported in Bronx, New York and found 3 cases in the months January and February, 2017.
</figure-inline></figure-inline></figure-inline></figure-inline></figure-inline></figure-inline></figure-inline></figure-inline></figure-inline></figure-inline></figure-inline></figure-inline></figure-inline></figure-inline></figure-inline></figure-inline></figure-inline></figure-inline></figure-inline></figure-inline></figure-inline></figure-inline></figure-inline></figure-inline></figure-inline></figure-inline></figure-inline> Recent out break of leptospirosis is reported in Bronx, New York and found 3 cases in the months January and February, 2017.
![Histopathology of a pancreatic endocrine tumor (insulinoma). Source:https://librepathology.org/wiki/Neuroendocrine_tumour_of_the_pancreas[1]](/images/2/2f/Pancreatic_insulinoma_histology_2.JPG)
![Histopathology of a pancreatic endocrine tumor (insulinoma). Chromogranin A immunostain. Source:https://librepathology.org/wiki/Neuroendocrine_tumour_of_the_pancreas[1]](/images/a/a3/Pancreatic_insulinoma_histopathology_3.JPG)
![Histopathology of a pancreatic endocrine tumor (insulinoma). Insulin immunostain. Source:https://librepathology.org/wiki/Neuroendocrine_tumour_of_the_pancreas[1]](/images/d/d5/Pancreatic_insulinoma_histology_4.JPG)