Fibroma x ray: Difference between revisions
No edit summary |
No edit summary |
||
| (13 intermediate revisions by 2 users not shown) | |||
| Line 3: | Line 3: | ||
{{CMG}}; {{AE}} {{M.N}}, {{Simrat}} | {{CMG}}; {{AE}} {{M.N}}, {{Simrat}} | ||
==Overview== | ==Overview== | ||
[[X-ray]] may be helpful in the [[diagnosis]] of fibroma. Findings on [[x-ray]] suggestive of a particular fibroma depends on the type of the fibroma. Findings on [[x-ray]] suggestive of non-ossifying fibromas include sharply demarcated, asymmetrical, and [[Cortical bone|cortically]] based lucencies with a thin sclerotic rim. Findings on [[x-ray]] suggestive of [[ossifying fibroma]] include well-circumscribed [[lesion]], intracortical [[Osteolysis|osteolysi]]<nowiki/>s with a characteristic sclerotic band, [[Cortical bone|cortical]] expansion, and a [[lytic]] thinning of the [[Diaphysis|diaphyseal]] [[cortical bone]] with interspersed [[sclerosis]]. Findings on [[x-ray]] suggestive of [[chondromyxoid fibroma]] include a lobulated, eccentric [[radiolucent]] [[lesion]]. Findings on [[x-ray]] suggestive of desmoplastic fibroma include a [[lytic]] [[bone]] [[lesions]] with a geographic pattern of [[bone]] destruction and a narrow zone of [[transition]] and non-sclerotic margins. | [[X-ray]] may be helpful in the [[diagnosis]] of fibroma. Findings on [[x-ray]] suggestive of a particular fibroma depends on the type of the fibroma. Findings on [[x-ray]] suggestive of non-ossifying fibromas include sharply demarcated, asymmetrical, and [[Cortical bone|cortically]] based lucencies with a thin sclerotic rim. Findings on [[x-ray]] suggestive of [[ossifying fibroma]] include well-circumscribed [[lesion]], intracortical [[Osteolysis|osteolysi]]<nowiki/>s with a characteristic sclerotic band, [[Cortical bone|cortical]] expansion, and a [[lytic]] thinning of the [[Diaphysis|diaphyseal]] [[cortical bone]] with interspersed [[sclerosis]]. Findings on [[x-ray]] suggestive of [[chondromyxoid fibroma]] include a lobulated, eccentric [[radiolucent]] [[lesion]]. Findings on [[x-ray]] suggestive of desmoplastic fibroma include a [[lytic]] [[bone]] [[lesions]] with a geographic pattern of [[bone]] destruction and a narrow zone of [[transition]] and non-sclerotic margins. | ||
==X-Ray== | ==X Ray== | ||
===Ossifying Fibroma=== | |||
*The following [[radiographic]] features are noted on [[x-ray]] of ossifying fibroma:<ref name="pmid20587656">{{cite journal| author=Araki M, Matsumoto K, Matsumoto N, Honda K, Ohki H, Komiyama K| title=Unusual radiographic appearance of ossifying fibroma in the left mandibular angle. | journal=Dentomaxillofac Radiol | year= 2010 | volume= 39 | issue= 5 | pages= 314-9 | pmid=20587656 | doi=10.1259/dmfr/81820042 | pmc=3520244 | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=20587656 }} </ref> | |||
**Ossifying fibroma is seen as a well-circumscribed lesion | |||
**Ossifying fibroma demonstrates evidence of intracortical [[osteolysis]] with a characteristic sclerotic band | |||
**[[Cortical bone|Cortical]] expansion | |||
**[[Radiographic]] features of ossifying fibroma include a [[lytic]] thinning of the [[Diaphysis|diaphyseal]] [[cortical bone]] with interspersed [[sclerosis]].<ref name="pmid8692589">{{cite journal| author=Copley L, Dormans JP| title=Benign pediatric bone tumors. Evaluation and treatment. | journal=Pediatr Clin North Am | year= 1996 | volume= 43 | issue= 4 | pages= 949-66 | pmid=8692589 | doi= | pmc= | url=http://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=8692589 }} | |||
==X Ray== | |||
===Non-ossifying Fibroma=== | ===Non-ossifying Fibroma=== | ||
| Line 11: | Line 20: | ||
*They often appear multiloculated. They are located in the metaphysis, adjacent to the physis. As the patient ages, they seem to migrate away from the growth plate. | *They often appear multiloculated. They are located in the metaphysis, adjacent to the physis. As the patient ages, they seem to migrate away from the growth plate. | ||
*They have no associated periosteal reaction, cortical breach or associated soft tissue mass. | *They have no associated periosteal reaction, cortical breach or associated soft tissue mass. | ||
*[[Nonossifying fibroma]] appear as well defined, small, eccentric, lytic, expansile lesions located in the metaphysis with scalloped sclerotic borders. Multiple lesions may be present.<nowiki><ref name="pmid12544273"></nowiki>{{cite journal| author=Yildiz C, Erler K, Atesalp AS, Basbozkurt M| title=Benign bone tumors in children. | journal=Curr Opin Pediatr | year= 2003 | volume= 15 | issue= 1 | pages= 58-67 | pmid=12544273 | doi= | pmc= | url=http://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=12544273 | *[[Nonossifying fibroma]] appear as well defined, small, eccentric, lytic, expansile lesions located in the metaphysis with scalloped sclerotic borders. Multiple lesions may be present.<nowiki><ref name="pmid12544273"></nowiki>{{cite journal| author=Yildiz C, Erler K, Atesalp AS, Basbozkurt M| title=Benign bone tumors in children. | journal=Curr Opin Pediatr | year= 2003 | volume= 15 | issue= 1 | pages= 58-67 | pmid=12544273 | doi= | pmc= | url=http://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=12544273 }}</ref> | ||
===Chondromyxoid Fibroma=== | ===Chondromyxoid Fibroma=== | ||
The following features are seen on plain [[radiograph]] of chondromyxoid fibromas:<ref name="CappellePans2016">{{cite journal|last1=Cappelle|first1=Sarah|last2=Pans|first2=Steven|last3=Sciot|first3=Raf|title=Imaging features of chondromyxoid fibroma: report of 15 cases and literature review|journal=The British Journal of Radiology|volume=89|issue=1064|year=2016|pages=20160088|issn=0007-1285|doi=10.1259/bjr.20160088}}</ref> | *The following features are seen on plain [[radiograph]] of chondromyxoid fibromas:<ref name="CappellePans2016">{{cite journal|last1=Cappelle|first1=Sarah|last2=Pans|first2=Steven|last3=Sciot|first3=Raf|title=Imaging features of chondromyxoid fibroma: report of 15 cases and literature review|journal=The British Journal of Radiology|volume=89|issue=1064|year=2016|pages=20160088|issn=0007-1285|doi=10.1259/bjr.20160088}}</ref> | ||
*Chondromyxoid fibroma is seen as a lobulated, eccentric radiolucent [[lesion]] | **Chondromyxoid fibroma is seen as a lobulated, eccentric radiolucent [[lesion]] | ||
*Long axis is parallel to long axis of [[long bone]] | **Long axis is parallel to long axis of [[long bone]] | ||
*No [[periosteal reaction]] (unless a complicating [[fracture]] present) | **No [[periosteal reaction]] (unless a complicating [[fracture]] present) | ||
*In approximately 100% of cases geographic bone destruction is present | **In approximately 100% of cases geographic bone destruction is present | ||
*In approximately 85% of cases well defined sclerotic margin is present | **In approximately 85% of cases well defined sclerotic margin is present | ||
*In approximately 60% of cases there can be presence of septations (pseudo trabeculation) | **In approximately 60% of cases there can be presence of septations (pseudo trabeculation) | ||
*In approximately 12.5% there can be presence of [[matrix]] [[calcification]] | **In approximately 12.5% there can be presence of [[matrix]] [[calcification]] | ||
===Desmoplastic Fibroma=== | ===Desmoplastic Fibroma=== | ||
The following features are seen on plain [[radiograph]] of desmoplastic fibromas:<ref name="WoodsCohen2014">{{cite journal|last1=Woods|first1=T. R.|last2=Cohen|first2=D. M.|last3=Islam|first3=M. N.|last4=Rawal|first4=Y.|last5=Bhattacharyya|first5=I.|title=Desmoplastic Fibroma of the Mandible: A Series of Three Cases and Review of Literature|journal=Head and Neck Pathology|volume=9|issue=2|year=2014|pages=196–204|issn=1936-055X|doi=10.1007/s12105-014-0561-5}}</ref> | *The following features are seen on plain [[radiograph]] of desmoplastic fibromas:<ref name="WoodsCohen2014">{{cite journal|last1=Woods|first1=T. R.|last2=Cohen|first2=D. M.|last3=Islam|first3=M. N.|last4=Rawal|first4=Y.|last5=Bhattacharyya|first5=I.|title=Desmoplastic Fibroma of the Mandible: A Series of Three Cases and Review of Literature|journal=Head and Neck Pathology|volume=9|issue=2|year=2014|pages=196–204|issn=1936-055X|doi=10.1007/s12105-014-0561-5}}</ref> | ||
*[[Desmoplastic fibroma]] are typically seen as a [[lytic]] [[bone]] [[lesions]] with a geographic pattern of [[bone]] destruction | **[[Desmoplastic fibroma]] are typically seen as a [[lytic]] [[bone]] [[lesions]] with a geographic pattern of [[bone]] destruction | ||
*It often has a narrow zone of [[transition]] and non-sclerotic margins | **It often has a narrow zone of [[transition]] and non-sclerotic margins | ||
*In approximately more than 90% of cases internal pseudo trabeculation is present | **In approximately more than 90% of cases internal pseudo trabeculation is present | ||
*[[Matrix]] [[mineralization]] is not present | **[[Matrix]] [[mineralization]] is not present | ||
*In approximately 90% of cases widening of the host [[bone]] from gradual apposition of [[Periosteal reaction|periosteal]] new [[bone]] formation is seen | **In approximately 90% of cases widening of the host [[bone]] from gradual apposition of [[Periosteal reaction|periosteal]] new [[bone]] formation is seen | ||
[[File:Desmoplastic fibroma.jpg|400px|thumb|none|X-ray revealed uneven density in the distal left femur, in which lamellate high-density opacity and bone destruction were observed.,Xu Y, Wang Y, Yan J, Bai X, Xing G. Desmoplastic fibroma of the femur with atypical image findings: A case report. Medicine (Baltimore). 2018;97(52):e13787. Published 2018 Dec 28. doi:10.1097/MD.0000000000013787,https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6314775/]] | [[File:Desmoplastic fibroma.jpg|400px|thumb|none|X-ray revealed uneven density in the distal left femur, in which lamellate high-density opacity and bone destruction were observed.,Xu Y, Wang Y, Yan J, Bai X, Xing G. Desmoplastic fibroma of the femur with atypical image findings: A case report. Medicine (Baltimore). 2018;97(52):e13787. Published 2018 Dec 28. doi:10.1097/MD.0000000000013787,https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6314775/]] | ||
===Pleural Fibroma=== | ===Pleural Fibroma=== | ||
The following features are seen on plain [[radiograph]] of [[Pleural fibroma|pleural fibromas]]: | *The following features are seen on plain [[radiograph]] of [[Pleural fibroma|pleural fibromas]]:<ref name="MittalMittal2013">{{cite journal|last1=Mittal|first1=MaheshKumar|last2=Mittal|first2=Aliza|last3=Sinha|first3=Mukul|last4=Sureka|first4=Binit|last5=Thukral|first5=BrijBhushan|title=Radiological review of pleural tumors|journal=Indian Journal of Radiology and Imaging|volume=23|issue=4|year=2013|pages=313|issn=0971-3026|doi=10.4103/0971-3026.125577}}</ref> | ||
*On [[x-ray]] [[Pleural fibroma|pleural fibromas]] presents as a pleural based mass. They tend to be relatively circumscribed and can sometimes be lobulated. It often forms an obtuse angle with the [[chest wall]]. [[Tumors]] may grow to a large size. [[Pedunculated]] [[lesions]] can change position and appearance with [[respiration]] or with a change in position. [[Calcification]], [[rib]] destruction, and [[Pleural effusion|pleural effusions]] are typically not associated features. | **On [[x-ray]] [[Pleural fibroma|pleural fibromas]] presents as a pleural based mass. They tend to be relatively circumscribed and can sometimes be lobulated. It often forms an obtuse angle with the [[chest wall]]. [[Tumors]] may grow to a large size. [[Pedunculated]] [[lesions]] can change position and appearance with [[respiration]] or with a change in position. [[Calcification]], [[rib]] destruction, and [[Pleural effusion|pleural effusions]] are typically not associated features. | ||
===Cemento-ossifying fibroma=== | ===Cemento-ossifying fibroma=== | ||
The following features are seen on plain [[radiograph]] of cemento-ossifying fibromas:<ref name="pmid23029635">{{cite journal| author=Mithra R, Baskaran P, Sathyakumar M| title=Imaging in the diagnosis of cemento-ossifying fibroma: a case series. | journal=J Clin Imaging Sci | year= 2012 | volume= 2 | issue= | pages= 52 | pmid=23029635 | doi=10.4103/2156-7514.100373 | pmc=3440937 | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=23029635 }} </ref> | *The following features are seen on plain [[radiograph]] of cemento-ossifying fibromas:<ref name="pmid23029635">{{cite journal| author=Mithra R, Baskaran P, Sathyakumar M| title=Imaging in the diagnosis of cemento-ossifying fibroma: a case series. | journal=J Clin Imaging Sci | year= 2012 | volume= 2 | issue= | pages= 52 | pmid=23029635 | doi=10.4103/2156-7514.100373 | pmc=3440937 | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=23029635 }} </ref> | ||
*[[Cemento-ossifying fibroma]] are usually well circumscribed masses which expand the underlying [[bone]]. They are usually small, but can become large. This is particularly the case when they arise from the [[maxilla]] or [[paranasal sinuses]] because there is more room to expand. | **[[Cemento-ossifying fibroma]] are usually well circumscribed masses which expand the underlying [[bone]]. They are usually small, but can become large. This is particularly the case when they arise from the [[maxilla]] or [[paranasal sinuses]] because there is more room to expand. | ||
*They are initially lucent on [[x-ray]]. As they mature, they gradually develop increasing amounts of [[calcification]]/[[ossification]] as they mature. They usually expand the [[bone]] without [[Cortical area|cortical]] breach. | **They are initially lucent on [[x-ray]]. As they mature, they gradually develop increasing amounts of [[calcification]]/[[ossification]] as they mature. They usually expand the [[bone]] without [[Cortical area|cortical]] breach. | ||
===Uterine Fibromas=== | ===Uterine Fibromas=== | ||
| Line 51: | Line 54: | ||
===Non-ossifying Fibroma=== | ===Non-ossifying Fibroma=== | ||
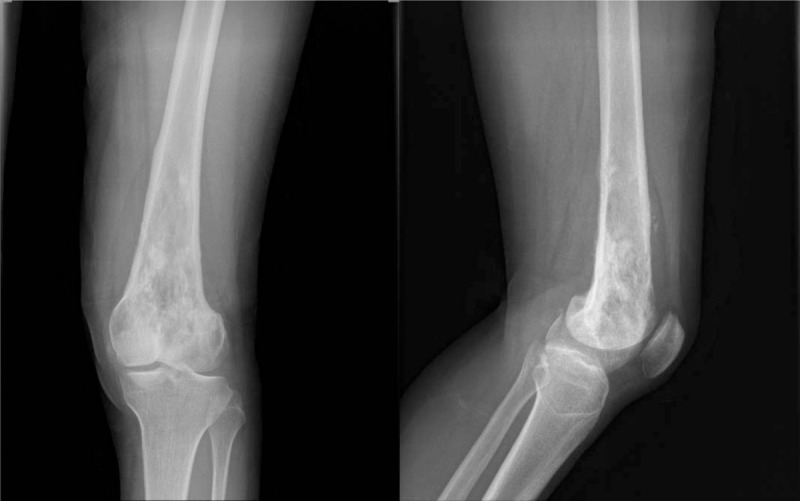
*On x- | *On [[x-ray]], non-ossifying fibromas are characterized by sharply demarcated, asymmetrical, cortically based lucencies with a thin sclerotic rim.<ref name="pmid30541476">{{cite journal| author=Su W, Shi X, Lin M, Huang C, Wang L, Song H et al.| title=Non-ossifying fibroma with a pathologic fracture in a 12-year-old girl with tricho-rhino-phalangeal syndrome: a case report. | journal=BMC Med Genet | year= 2018 | volume= 19 | issue= 1 | pages= 211 | pmid=30541476 | doi=10.1186/s12881-018-0732-4 | pmc=6292130 | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=30541476 }} </ref> | ||
*They often appear multiloculated. They are located in the metaphysis, adjacent to the physis. As the patient ages, they seem to migrate away from the growth plate. | *They often appear multiloculated. They are located in the metaphysis, adjacent to the physis. As the patient ages, they seem to migrate away from the growth plate. | ||
*They have no associated periosteal reaction, cortical breach or associated soft tissue mass. | *They have no associated periosteal reaction, cortical breach or associated soft tissue mass. | ||
*Nonossifying fibroma appear as well defined, small, eccentric, lytic, expansile lesions located in the metaphysis with scalloped sclerotic borders. Multiple lesions may be present. | *Nonossifying fibroma appear as well defined, small, eccentric, lytic, expansile lesions located in the metaphysis with scalloped sclerotic borders. Multiple lesions may be present. | ||
==References== | ==References== | ||
Latest revision as of 16:47, 31 July 2019
|
Fibroma Microchapters |
|
Diagnosis |
|---|
|
Treatment |
|
Case Studies |
|
Fibroma x ray On the Web |
|
American Roentgen Ray Society Images of Fibroma x ray |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]; Associate Editor(s)-in-Chief: Maneesha Nandimandalam, M.B.B.S.[2], Simrat Sarai, M.D. [3]
Overview
X-ray may be helpful in the diagnosis of fibroma. Findings on x-ray suggestive of a particular fibroma depends on the type of the fibroma. Findings on x-ray suggestive of non-ossifying fibromas include sharply demarcated, asymmetrical, and cortically based lucencies with a thin sclerotic rim. Findings on x-ray suggestive of ossifying fibroma include well-circumscribed lesion, intracortical osteolysis with a characteristic sclerotic band, cortical expansion, and a lytic thinning of the diaphyseal cortical bone with interspersed sclerosis. Findings on x-ray suggestive of chondromyxoid fibroma include a lobulated, eccentric radiolucent lesion. Findings on x-ray suggestive of desmoplastic fibroma include a lytic bone lesions with a geographic pattern of bone destruction and a narrow zone of transition and non-sclerotic margins.
X Ray
Ossifying Fibroma
- The following radiographic features are noted on x-ray of ossifying fibroma:[1]
- Ossifying fibroma is seen as a well-circumscribed lesion
- Ossifying fibroma demonstrates evidence of intracortical osteolysis with a characteristic sclerotic band
- Cortical expansion
- Radiographic features of ossifying fibroma include a lytic thinning of the diaphyseal cortical bone with interspersed sclerosis.[2]
Chondromyxoid Fibroma
- The following features are seen on plain radiograph of chondromyxoid fibromas:[3]
- Chondromyxoid fibroma is seen as a lobulated, eccentric radiolucent lesion
- Long axis is parallel to long axis of long bone
- No periosteal reaction (unless a complicating fracture present)
- In approximately 100% of cases geographic bone destruction is present
- In approximately 85% of cases well defined sclerotic margin is present
- In approximately 60% of cases there can be presence of septations (pseudo trabeculation)
- In approximately 12.5% there can be presence of matrix calcification
Desmoplastic Fibroma
- The following features are seen on plain radiograph of desmoplastic fibromas:[4]
- Desmoplastic fibroma are typically seen as a lytic bone lesions with a geographic pattern of bone destruction
- It often has a narrow zone of transition and non-sclerotic margins
- In approximately more than 90% of cases internal pseudo trabeculation is present
- Matrix mineralization is not present
- In approximately 90% of cases widening of the host bone from gradual apposition of periosteal new bone formation is seen
Pleural Fibroma
- The following features are seen on plain radiograph of pleural fibromas:[5]
- On x-ray pleural fibromas presents as a pleural based mass. They tend to be relatively circumscribed and can sometimes be lobulated. It often forms an obtuse angle with the chest wall. Tumors may grow to a large size. Pedunculated lesions can change position and appearance with respiration or with a change in position. Calcification, rib destruction, and pleural effusions are typically not associated features.
Cemento-ossifying fibroma
- The following features are seen on plain radiograph of cemento-ossifying fibromas:[6]
- Cemento-ossifying fibroma are usually well circumscribed masses which expand the underlying bone. They are usually small, but can become large. This is particularly the case when they arise from the maxilla or paranasal sinuses because there is more room to expand.
- They are initially lucent on x-ray. As they mature, they gradually develop increasing amounts of calcification/ossification as they mature. They usually expand the bone without cortical breach.
Uterine Fibromas
- On x-ray popcorn calcification within the pelvis may suggest the diagnosis of uterine fibromas.
Non-ossifying Fibroma
- On x-ray, non-ossifying fibromas are characterized by sharply demarcated, asymmetrical, cortically based lucencies with a thin sclerotic rim.[7]
- They often appear multiloculated. They are located in the metaphysis, adjacent to the physis. As the patient ages, they seem to migrate away from the growth plate.
- They have no associated periosteal reaction, cortical breach or associated soft tissue mass.
- Nonossifying fibroma appear as well defined, small, eccentric, lytic, expansile lesions located in the metaphysis with scalloped sclerotic borders. Multiple lesions may be present.
References
- ↑ Araki M, Matsumoto K, Matsumoto N, Honda K, Ohki H, Komiyama K (2010). "Unusual radiographic appearance of ossifying fibroma in the left mandibular angle". Dentomaxillofac Radiol. 39 (5): 314–9. doi:10.1259/dmfr/81820042. PMC 3520244. PMID 20587656.
- ↑ Copley L, Dormans JP (1996). "Benign pediatric bone tumors. Evaluation and treatment". Pediatr Clin North Am. 43 (4): 949–66. PMID 8692589.
X Ray
Non-ossifying Fibroma
- On X-Ray, non-ossifying fibromas are characterized by sharply demarcated, asymmetrical, cortically based lucencies with a thin sclerotic rim.
- They often appear multiloculated. They are located in the metaphysis, adjacent to the physis. As the patient ages, they seem to migrate away from the growth plate.
- They have no associated periosteal reaction, cortical breach or associated soft tissue mass.
- Nonossifying fibroma appear as well defined, small, eccentric, lytic, expansile lesions located in the metaphysis with scalloped sclerotic borders. Multiple lesions may be present.<ref name="pmid12544273">Yildiz C, Erler K, Atesalp AS, Basbozkurt M (2003). "Benign bone tumors in children". Curr Opin Pediatr. 15 (1): 58–67. PMID 12544273.
- ↑ Cappelle, Sarah; Pans, Steven; Sciot, Raf (2016). "Imaging features of chondromyxoid fibroma: report of 15 cases and literature review". The British Journal of Radiology. 89 (1064): 20160088. doi:10.1259/bjr.20160088. ISSN 0007-1285.
- ↑ Woods, T. R.; Cohen, D. M.; Islam, M. N.; Rawal, Y.; Bhattacharyya, I. (2014). "Desmoplastic Fibroma of the Mandible: A Series of Three Cases and Review of Literature". Head and Neck Pathology. 9 (2): 196–204. doi:10.1007/s12105-014-0561-5. ISSN 1936-055X.
- ↑ Mittal, MaheshKumar; Mittal, Aliza; Sinha, Mukul; Sureka, Binit; Thukral, BrijBhushan (2013). "Radiological review of pleural tumors". Indian Journal of Radiology and Imaging. 23 (4): 313. doi:10.4103/0971-3026.125577. ISSN 0971-3026.
- ↑ Mithra R, Baskaran P, Sathyakumar M (2012). "Imaging in the diagnosis of cemento-ossifying fibroma: a case series". J Clin Imaging Sci. 2: 52. doi:10.4103/2156-7514.100373. PMC 3440937. PMID 23029635.
- ↑ Su W, Shi X, Lin M, Huang C, Wang L, Song H; et al. (2018). "Non-ossifying fibroma with a pathologic fracture in a 12-year-old girl with tricho-rhino-phalangeal syndrome: a case report". BMC Med Genet. 19 (1): 211. doi:10.1186/s12881-018-0732-4. PMC 6292130. PMID 30541476.