Bronchoalveolar carcinoma: Difference between revisions
Trushatank (talk | contribs) |
|||
| (36 intermediate revisions by 3 users not shown) | |||
| Line 1: | Line 1: | ||
__NOTOC__ | __NOTOC__ | ||
{{SI}} | {{SI}} | ||
{{CMG}} | {{CMG}} '''Associate Editor-in-Chief:''' [https://www.wikidoc.org/index.php/User%3AK.Nouman <nowiki>Khuram Nouman, M.D. [2]</nowiki>] | ||
==Overview== | ==Overview== | ||
[[Lung cancer]] the leading cause of cancer related death in the world. Bronchoalveolar carcinoma (BAC) was first described by Malassez in 1876 as a bilateral,multinodular malignant [[pulmonary carcinoma]]. " Bronchoalveolar cell carcinoma" term was first coined by Leibow in 1960 due to confusion over cell type. BAC was use as a term in 1999 and 2004 WHO classification for a broad range of [[Tumor|tumors]] including single small [[non-invasive peripheral lung tumor]], minimally invasive adenocarcinoma, mixed subtype invasive adenocarcinoma, mucinous and nonmucinous subtypes that are previously known as BAC and advanced type with invasion and poor prognosis. The 1999 WHO classification was largely based on histologic characteristics, the 2004 revised classification in addition to histological factors took other factors like genetic and clinical factors into consideration but these two classification continue to use the term BAC. Later, in 2011 IASLC in collaboration with other lung societies introduced a new classification based on multidisciplinary approach to avoid the confusion related to use of BAC for broad range of tumors. Bronchoalveolar carcinoma is a preinvasive carcinoma with no [[Stromal cell|stromal]],[[vascular]] and [[pleural invasion]]. Adenocarcinoma in situ, minimally invasive adenocarcinoma and invasive adenocarcinoma of the lung are the relatively new terms that were introduced in 2011 [[IASLC/ATS/ERS classifications]] for [[bronchoalveolar carcinoma]] (BAC). BAC is usually asymptomatic but may present with [[cough]], [[hemoptysis]], [[Chest pain, cough and dyspnea|chest pain]], [[loss of appetite]] and [[weight loss]]. It is a rare pulmonary tumor and the incidence for BAC varies from 4-24% of all the primary lung malignancies. Surgery is the mainstay of treatment but mucinous type respond very well to [[List of chemotherapy regimens|chemotherapy]] because of genetic associations. The five year survival rate for surgically resected tumor is 100%. | |||
==Historical Perspective== | ==Historical Perspective== | ||
*Bronchoalveolar Carcinoma was first described by Malassez in 1876 as a bilateral, multinodular type of malignant lung carcinoma. | *Bronchoalveolar Carcinoma was first described by Malassez in 1876 as a bilateral, multinodular type of malignant lung carcinoma. | ||
*The term "Bronchoalveolar cell carcinoma" was first introduced by Liebow in 1960 due to confusion over true cell type.It comes from two cell types. columnar epithelium similar to bronchial cells and cuboidal type reminiscent of type 2 pneumocytes | *The term "Bronchoalveolar cell carcinoma" was first introduced by Liebow in 1960 due to confusion over true cell type.It comes from two cell types. [[Columnar epithelia|columnar epithelium]] similar to [[bronchial cells]] and [[Cuboidal epithelia|cuboidal]] type reminiscent of type 2 pneumocytes. | ||
==Classification== | ==Classification== | ||
*Bronchoalveolar Carcinoma may be classified according to pathology into fo subtypes/groups: | *Bronchoalveolar Carcinoma may be classified according to pathology into fo subtypes/groups: | ||
'''Pathology of lung adenocarcinomas according to previous 2004 WHO and current IASLC/ATS/ERS classifications''' | |||
{| class="wikitable" | {| class="wikitable" | ||
| colspan="1" rowspan="1" |2004 WHO classification | | colspan="1" rowspan="1" style="background:#4479BA; color: #FFFFFF;" align="center" |2004 WHO classification | ||
|- | |- | ||
| colspan="1" rowspan="1" | Mixed subtype | | colspan="1" rowspan="1" | Mixed subtype | ||
|- | |- | ||
| colspan="1" rowspan="1" | Acinar | | colspan="1" rowspan="1" | [[Acinar]] | ||
|- | |- | ||
| colspan="1" rowspan="1" | Papillary | | colspan="1" rowspan="1" | [[Papillary]] | ||
|- | |- | ||
| colspan="1" rowspan="1" | BAC | | colspan="1" rowspan="1" | BAC | ||
|- | |- | ||
| colspan="1" rowspan="1" | | | colspan="1" rowspan="1" | [[Non mucinous]] | ||
|- | |- | ||
| colspan="1" rowspan="1" | | | colspan="1" rowspan="1" | [[Mucinous]] | ||
|- | |- | ||
| colspan="1" rowspan="1" | Mixed | | colspan="1" rowspan="1" | Mixed | ||
| Line 32: | Line 31: | ||
| colspan="1" rowspan="1" | Solid adenocarcinoma | | colspan="1" rowspan="1" | Solid adenocarcinoma | ||
|- | |- | ||
| colspan="1" rowspan="1" | | | colspan="1" rowspan="1" | [[Colloid]] | ||
|- | |- | ||
| colspan="1" rowspan="1" | | | colspan="1" rowspan="1" | [[Fetal]] | ||
|- | |- | ||
| colspan="1" rowspan="1" | | | colspan="1" rowspan="1" | [[Mucinous cystadenocarcinoma]] | ||
|- | |- | ||
| colspan="1" rowspan="1" | | | colspan="1" rowspan="1" | [[Signet-ring]] | ||
|- | |- | ||
| colspan="1" rowspan="1" | | | colspan="1" rowspan="1" | [[Clear-cell]] | ||
|- | |- | ||
| colspan="1" rowspan="1" |Major changes in the new IASLC/ATS/ERS classification | | colspan="1" rowspan="1" style="background:#4479BA; color: #FFFFFF;" align="center" |Major changes in the new IASLC/ATS/ERS classification | ||
|- | |- | ||
| colspan="1" rowspan="1" | Discontinuation of the term BAC | | colspan="1" rowspan="1" | Discontinuation of the term BAC | ||
| Line 52: | Line 51: | ||
| colspan="1" rowspan="1" | Introduction of AIS and MIA as new entities | | colspan="1" rowspan="1" | Introduction of AIS and MIA as new entities | ||
|- | |- | ||
| colspan="1" rowspan="1" | Introduction of micropapillary adenocarcinoma as a predominant subtype | | colspan="1" rowspan="1" | Introduction of [[micropapillary adenocarcinoma]] as a predominant subtype | ||
|- | |- | ||
| colspan="1" rowspan="1" | Introduction of lepidic predominant adenocarcinoma and lepidic growth as new terminologies | | colspan="1" rowspan="1" | Introduction of lepidic predominant adenocarcinoma and [[lepidic growth]] as new terminologies | ||
|- | |- | ||
| colspan="1" rowspan="1" | Exclusion of signet-ring and clear cell adenocarcinomas | | colspan="1" rowspan="1" | Exclusion of signet-ring and clear cell adenocarcinomas | ||
|- | |- | ||
| colspan="1" rowspan="1" |IASLC/ATS/ERS classification | | colspan="1" rowspan="1" style="background:#4479BA; color: #FFFFFF;" align="center" |IASLC/ATS/ERS classification | ||
|- | |- | ||
| colspan="1" rowspan="1" | Pre-invasive lesions | | colspan="1" rowspan="1" | Pre-invasive lesions | ||
| Line 66: | Line 65: | ||
| colspan="1" rowspan="1" | AIS | | colspan="1" rowspan="1" | AIS | ||
|- | |- | ||
| colspan="1" rowspan="1" | | | colspan="1" rowspan="1" | [[Non-mucinous]] | ||
|- | |- | ||
| colspan="1" rowspan="1" | | | colspan="1" rowspan="1" | [[Mucinous]] | ||
|- | |- | ||
| colspan="1" rowspan="1" | Mixed | | colspan="1" rowspan="1" | Mixed | ||
| Line 76: | Line 75: | ||
| colspan="1" rowspan="1" | Non-mucinous | | colspan="1" rowspan="1" | Non-mucinous | ||
|- | |- | ||
| colspan="1" rowspan="1" | | | colspan="1" rowspan="1" | [[Mucinous]] | ||
|- | |- | ||
| colspan="1" rowspan="1" | Mixed | | colspan="1" rowspan="1" | Mixed | ||
| Line 86: | Line 85: | ||
| colspan="1" rowspan="1" | Acinar predominant | | colspan="1" rowspan="1" | Acinar predominant | ||
|- | |- | ||
| colspan="1" rowspan="1" | Papillary predominant | | colspan="1" rowspan="1" | [[Apillary predominant| Papillary predominant]] | ||
|- | |- | ||
| colspan="1" rowspan="1" | | | colspan="1" rowspan="1" | [[Micropapillary predominant]] | ||
|- | |- | ||
| colspan="1" rowspan="1" | Solid predominant with mucin production | | colspan="1" rowspan="1" | Solid predominant with mucin production | ||
| Line 98: | Line 97: | ||
| colspan="1" rowspan="1" | Colloid | | colspan="1" rowspan="1" | Colloid | ||
|- | |- | ||
| colspan="1" rowspan="1" | | | colspan="1" rowspan="1" | [[Fetal]] | ||
|- | |- | ||
| colspan="1" rowspan="1" | | | colspan="1" rowspan="1" | [[Enteric]] | ||
|} | |} | ||
WHO, World Health Organization; IASLC, International Association for the Study of Lung Cancer; ATS, American Thoracic Society; ERS, European Respiratory Society; BAC, bronchioloalveolar carcinoma; AIS, adenocarcinoma ''in situ''; MIA, minimally invasive adenocarcinoma; IMA, invasive mucinous adenocarcinoma. | <small> WHO, World Health Organization; IASLC, International Association for the Study of Lung Cancer; ATS, American Thoracic Society; ERS, European Respiratory Society; BAC, bronchioloalveolar carcinoma; AIS, adenocarcinoma ''in situ''; MIA, minimally invasive adenocarcinoma; IMA, invasive mucinous adenocarcinoma. </small> | ||
==Pathophysiology== | ==Pathophysiology== | ||
* | *In 2011, the term bronchoalveolar carcinoma is discontinued and new terms [[adenocarcinoma in situ]] and minimally invasive adenocarcinoma replaced the term BAC, | ||
* | {| class="wikitable" | ||
* | |+ | ||
* | ! style="background:#4479BA; color: #FFFFFF;" align="center" |Type | ||
! style="background:#4479BA; color: #FFFFFF;" align="center" |Subtypes | |||
! style="background:#4479BA; color: #FFFFFF;" align="center" |Cell Type | |||
! style="background:#4479BA; color: #FFFFFF;" align="center" |Comments | |||
|- | |||
![[Adenocarcinoma in Situ]] | |||
| | |||
* [[Non Mucinous]] | |||
* [[Mucinous]] | |||
* Mixed | |||
| | |||
Non-Mucinous: | |||
* type II pneumocytes and/or Clara cells | |||
Mucinous: | |||
* tall [[columnar cells]] with basal nuclei | |||
* abundant cytoplasmic mucin | |||
| | |||
* Non-Mucinous type is most common | |||
* Small size < 3 cm | |||
* pure lepidic growth | |||
* Well circumscribed | |||
* No [[stromal]], [[vascular]] or [[pleural invasion]]. | |||
|- | |||
![[Minimally Invasive Adenocarcinoma]] | |||
| | |||
* Non Mucinous | |||
* [[Mucinous]] | |||
| | |||
* Non-Mucinous | |||
* [[Mucinous]] | |||
| | |||
* lepidic pattern | |||
* Small size < 3 cm | |||
* < 5 mm invasion | |||
|} | |||
* | |||
==Differentiating Bronchoalveolar carcinoma from other Diseases== | ==Differentiating Bronchoalveolar carcinoma from other Diseases== | ||
*BAC must be differentiated from other diseases that cause cough, hemoptysis, and solitary nodule on X-Ray such as: | *BAC must be differentiated from other diseases that cause cough, hemoptysis, and solitary nodule on X-Ray such as: | ||
:*Malignant and benign lesion | :*Malignant and benign lesion | ||
:* | :*Infection e.g pulmonary [[Tuberculosis, pulmonary|tuberculosis]] | ||
:*Congenital | :*Congenital | ||
:* | :*Miscellaneous e.g [[Wegener's granulomatosis|Wegener]] and [[lymphomatoid granulomatosis]] | ||
==Epidemiology and Demographics== | ==Epidemiology and Demographics== | ||
* Bronchoalveolar carcinoma is a rare tumor, the incidence of BAC vary from 4-24% of all the primary lung malignancies. More newer studies suggest Adenocarcinoma in situ and minimally invasive carcinoma constitutes 2-14% of all the primary types of lung cancers. | * Bronchoalveolar carcinoma is a rare tumor, the incidence of BAC vary from 4-24% of all the primary lung malignancies. More newer studies suggest [[Adenocarcinoma]] in situ and minimally invasive carcinoma constitutes 2-14% of all the primary types of lung cancers. | ||
===Age=== | ===Age=== | ||
*Patients of all age groups may develop | *Patients of all age groups may develop BAC. | ||
* | *BAC is more commonly observed among patients of middle aged group. | ||
===Gender=== | ===Gender=== | ||
*Bronchoalveolar Carcinoma affects men and women disproportionately. | *Bronchoalveolar Carcinoma affects men and women disproportionately. | ||
*Women are more commonly affected with bronchoalveolar carcinoma than men. | *Women are more commonly affected with bronchoalveolar [[carcinoma]] than men. | ||
===Race=== | ===Race=== | ||
| Line 138: | Line 169: | ||
==Risk Factors== | ==Risk Factors== | ||
*Common risk factors in the development of BAC are Asian race, women gender, and pulmonary fibrosis. | *Common risk factors in the development of BAC are Asian race, women gender, and [[pulmonary fibrosis]]. | ||
== Lung cancer Screening == | |||
The U.S. Preventive Services Task Force recommends annual [[lung cancer]] screening with low density [[Computed tomography|CT Scan]] for people who has history of, | |||
* Have a 30 pack per year or more smoking history, '''''and''''' | |||
* Current smoker or left smoking within the past 15 years, '''''and''''' | |||
* Are aged between 55 and 80 years old. | |||
== Natural History, Complications and Prognosis== | == Natural History, Complications and Prognosis== | ||
*The majority of patients with | *The majority of patients with BAC remain asymptomatic for many years. | ||
* | *Late clinical features include [[cough]], [[mucus production]], and persistent [[chest pain.]] | ||
*If left untreated, | *If left untreated,patients with BAC may progress to invasive adenocarcinoma. | ||
*Prognosis is generally good, and the 5 survival rate of patients with BAC is approximately. | |||
*Prognosis is generally | *Prognosis of BAC depends on the histologic type. Non-mucinous AIS has better prognosis than [[mucinous]] type AIS. | ||
*Mixed type has far worse survival rate than either of the [[monophasic]] form. | |||
== Diagnosis == | == Diagnosis == | ||
=== Clinical Features === | |||
Bronchoalveolar carcinoma is usually asymptomatic and takes a very long time before becoming symptomatic. BAC may cause large quantities of mucus production, patients may present with bronchorrhea. | |||
Solitary pulmonary nodule on Chest X-Ray that does not resolve despite taking antimicrobial therapy should be evaluated further for BAC. | |||
CT or guided biopsy should be done in such cases. to reach the definite diagnosis. | |||
===Diagnostic Criteria=== | ===Diagnostic Criteria=== | ||
*The diagnostic criteria for bronchoalveolar carcinoma have changed over time.According to new 2011 IASLC/ATS recommendations, adopted in the 2015 WHO guidelines, use the following criteria for bronchoalveolar carcinoma | *The diagnostic criteria for bronchoalveolar carcinoma have changed over time. According to new 2011 IASLC/ATS recommendations, adopted in the 2015 WHO guidelines, use the following criteria for bronchoalveolar carcinoma | ||
:*Localized small tumor < 3 cm | :*Localized small tumor < 3 cm | ||
:*pure "lepidic growth" | :*pure "[[lepidic growth]]" | ||
:*No stromal, vascular or pleural invasion | :*No [[stromal]], [[vascular]] or [[pleural]] invasion | ||
:*Nuclear atypia absent/minimal in both mucinous/non-mucinous AIS | :*[[Nuclear atypia]] absent/minimal in both mucinous/non-mucinous AIS | ||
:*Septal broadening with sclerosis (non-mucinous type) | :*[[Septal broadening]] with [[sclerosis]] (non-mucinous type) | ||
:*No spread through air spaces | :*No spread through air spaces | ||
=== Symptoms === | === Symptoms === | ||
*Bronchoalveolar carcinoma is usually asymptomatic. | *Bronchoalveolar carcinoma is usually asymptomatic because presence of symptoms are usually an indication of an advanced disease. | ||
*Symptoms of BAC may include the following: | *Symptoms of BAC may include the following: | ||
:*Cough | :*[[Cough]] | ||
:*Sputum | :*[[Sputum]] | ||
:* | :* | ||
:*Hemoptysis | :*[[Hemoptysis (patient information)|Hemoptysis]] | ||
:*Chest pain | :*[[Chest pain, cough and dyspnea|Chest pain]] | ||
:*Weakness | :*[[Weakness]] | ||
:*loss of appetite | :*[[loss of appetite]] | ||
:*Repeated Lung infections like pneumonia and bronchitis | :*Repeated [[Lung infections]] like [[pneumonia]] and [[bronchitis]] | ||
=== Physical Examination === | === Physical Examination === | ||
*Patients with BAC usually appear | *Patients with BAC usually appear | ||
*Physical examination may be remarkable for: | *Physical examination may be remarkable for: | ||
:*[ | :*[[Low-grade fever|Low grade fever]] | ||
:*[ | :*[[Cachexia]] | ||
:*[ | :*[[bronchorrhea]] | ||
:*[ | :*Other signs like [[dyspnea]], [[Pleural effusion|pleura]]<nowiki/>l effusion and enlargement of [[lymph nodes]] can occur in advanced stage disease. | ||
=== Laboratory Findings === | === Laboratory Findings === | ||
*There are no specific laboratory findings associated with [disease | *There are no specific laboratory findings associated with BAC. But, these lab findings can be helpful in patients with advanced diseases, | ||
{| class="wikitable" | |||
|+ | |||
! style="background:#4479BA; color: #FFFFFF;" align="center" + |Test | |||
! style="background:#4479BA; color: #FFFFFF;" align="center" + |Comments | |||
|- | |||
![[Complete blood count|CBC]] | |||
|To rule out [[neutropenic fever]] in patients taking [[chemotherapy]]. | |||
|- | |||
!Liver function test (LFTs) | |||
|Insignificant except in advanced disease. | |||
|- | |||
![[Electrolyte|Serum electrolytes]] | |||
|To check for hyponatremia to rule out [[SIADH]] | |||
|- | |||
!Arterial Blood Gases (ABGs) | |||
|To detect [[respiratory failure]] in sick patient. | |||
|- | |||
!Serum [[Calcium]] | |||
|[[Hypercalcemia]] can occur due to Parathyroid hormone related protein (PTH-rP) | |||
|- | |||
!Serum [[PTH]] | |||
|To check for cause of [[hypercalcemia]]. It helps to differentiate whether the high calcium level is due to [[hyperparathyroidism]] or [[paraneoplastic syndrome]] (PTH-rP) | |||
|} | |||
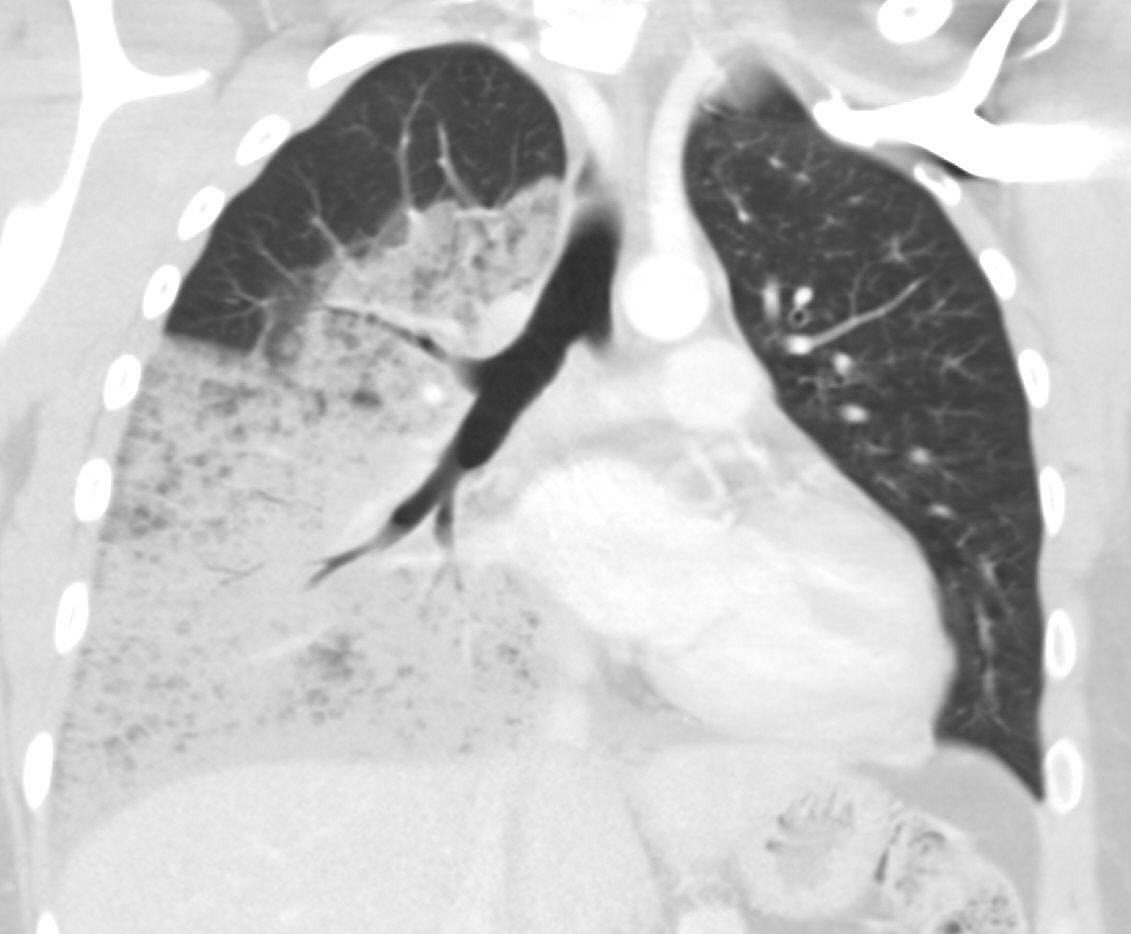
===Imaging Findings=== | ===Imaging Findings=== | ||
*There are three radiologic findings associated with bronchoalveolar carcinoma are | *There are three radiologic findings associated with bronchoalveolar carcinoma are: | ||
**Solitary nodule- most common | **[[Solitary nodule]]- most common | ||
**Consolidation | **[[Consolidation (medicine)|Consolidation]] | ||
** | **Multinodular opacities | ||
*The nodular form is the commonest and can not be differentiated from other adenocarcinoma subtypes on plain X-ray. | *The [[nodular]] form is the commonest and can not be differentiated from other adenocarcinoma subtypes on plain X-ray. | ||
*CT scan is imaging modality of the choice for bronchoalveolar carcinoma. | *[[CT scan]] is imaging modality of the choice for bronchoalveolar carcinoma. | ||
**Non-Mucinous BAC: It appears as solid nodule surrounded by ground glass opacification- Fried egg sign | **Non-Mucinous BAC: It appears as solid nodule surrounded by ground glass opacification- [[Fried egg sign]] | ||
**Mucinous BAC: It appears as single solid nodule. | **Mucinous BAC: It appears as single solid nodule | ||
'''Bronchoalveolar carcinoma CT scan''' | |||
*Subtype of adenocarcinoma<ref name="GandaraAberle2006">{{cite journal|last1=Gandara|first1=David R.|last2=Aberle|first2=Denise|last3=Lau|first3=Derick|last4=Jett|first4=James|last5=Akhurst|first5=Tim|last6=Mulshine|first6=James|last7=Berg|first7=Christine|last8=Patz|first8=Edward F.|title=Radiographic Imaging of Bronchioloalveolar Carcinoma: Screening, Patterns of Presentation and Response Assessment|journal=Journal of Thoracic Oncology|volume=1|issue=9|year=2006|pages=S20–S26|issn=15560864|doi=10.1016/S1556-0864(15)30005-8}}</ref> | |||
*Single pulmonary nodule or mass | |||
*Multicentric or diffuse disease | |||
*Localized area of parenchymal consolidation | |||
*Bubble-like areas of low attenuation within the mass are a characteristic finding | |||
*[[Hilar lymphadenopathy|Hilar]] and [[mediastinal lymphadenopathy]] is uncommon | |||
*Persistent peripheral [[Lung consolidation|consolidation]] with associated [[Pulmonary nodule|nodules]] | |||
<gallery align="right" mode="packed"> | <gallery align="right" mode="packed"> | ||
| Line 204: | Line 274: | ||
=== Other Diagnostic Studies === | === Other Diagnostic Studies === | ||
*BAC may also be differentiated from invasive adenocarcinoma by using magnetic resonance imaging. | *BAC may also be differentiated from invasive adenocarcinoma by using [[magnetic resonance imaging]]. | ||
*Image guided per-cutaneous fine needle aspiration biopsy or core biopsy can be used to get molecular characteristic of the tumor. | *Image guided per-cutaneous fine needle aspiration biopsy or core biopsy can be used to get molecular characteristic of the tumor. | ||
*[[ECG]] can be done to rule out other causes of chest pain. | |||
== Treatment == | == Treatment == | ||
=== Medical Therapy === | === Medical Therapy === | ||
*Non-Mucinous BAC responds well to targeted chemotherapy like epidermal growth factor receptor tyrosine kinase inhibitors erlotinib and gefitinib. | *Non-Mucinous BAC responds well to targeted [[chemotherapy]] like epidermal growth factor receptor [[tyrosine kinase inhibitors]] [[erlotinib]] and [[gefitinib.]] | ||
*Patient with non-resectable tumor can benefit from erlotinib and gefitinib than other subtypes of non small cell lung carcinoma. | *Patient with non-resectable tumor can also benefit from [[erlotinib]] and [[gefitinib]] than other subtypes of [[Non small cell lung cancer|non small cell lung carcinoma]]. | ||
*Mucinous BAC are highly associated with K-RAS mutation and wild-type EGFR and does not respond well to EGFR tyrosine kinase inhibitor. | *Mucinous BAC are highly associated with K-RAS mutation and wild-type [[EGFR]] and does not respond well to EGFR [[tyrosine kinase inhibitor]]. | ||
=== Surgery === | === Surgery === | ||
*Surgery is the mainstay of therapy for bronchoalveolar carcinoma. | *Surgery is the mainstay of therapy for bronchoalveolar carcinoma. | ||
*Pneumonectomy or lobectomy in conjunction with ipsilateral lymphadenectomy is the most common approach to the treatment of BAC. | *[[Pneumonectomy]] or [[Lobectomy of lung|lobectomy]] in conjunction with ipsilateral [[lymphadenectomy]] is the most common approach to the treatment of BAC. | ||
=== Prevention === | === Prevention === | ||
* Effective measures for the primary prevention of Lung cancer include smoking cessation, avoid passive smoking, and taking precautionary measures to avoid exposure to harmful particles in work places. | |||
*Effective measures for the primary prevention of | * | ||
See also, [https://www.uspreventiveservicestaskforce.org/Page/Document/UpdateSummaryFinal/lung-cancer-screening Lung cancer screening] [https://www.mskcc.org/cancer-care/types/lung/screening/lung-screening-decision-tool Lung Cancer Screening Decision Tool] | |||
==References== | ==References== | ||
<references /> | |||
Latest revision as of 16:49, 8 January 2019
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1] Associate Editor-in-Chief: Khuram Nouman, M.D. [2]
Overview
Lung cancer the leading cause of cancer related death in the world. Bronchoalveolar carcinoma (BAC) was first described by Malassez in 1876 as a bilateral,multinodular malignant pulmonary carcinoma. " Bronchoalveolar cell carcinoma" term was first coined by Leibow in 1960 due to confusion over cell type. BAC was use as a term in 1999 and 2004 WHO classification for a broad range of tumors including single small non-invasive peripheral lung tumor, minimally invasive adenocarcinoma, mixed subtype invasive adenocarcinoma, mucinous and nonmucinous subtypes that are previously known as BAC and advanced type with invasion and poor prognosis. The 1999 WHO classification was largely based on histologic characteristics, the 2004 revised classification in addition to histological factors took other factors like genetic and clinical factors into consideration but these two classification continue to use the term BAC. Later, in 2011 IASLC in collaboration with other lung societies introduced a new classification based on multidisciplinary approach to avoid the confusion related to use of BAC for broad range of tumors. Bronchoalveolar carcinoma is a preinvasive carcinoma with no stromal,vascular and pleural invasion. Adenocarcinoma in situ, minimally invasive adenocarcinoma and invasive adenocarcinoma of the lung are the relatively new terms that were introduced in 2011 IASLC/ATS/ERS classifications for bronchoalveolar carcinoma (BAC). BAC is usually asymptomatic but may present with cough, hemoptysis, chest pain, loss of appetite and weight loss. It is a rare pulmonary tumor and the incidence for BAC varies from 4-24% of all the primary lung malignancies. Surgery is the mainstay of treatment but mucinous type respond very well to chemotherapy because of genetic associations. The five year survival rate for surgically resected tumor is 100%.
Historical Perspective
- Bronchoalveolar Carcinoma was first described by Malassez in 1876 as a bilateral, multinodular type of malignant lung carcinoma.
- The term "Bronchoalveolar cell carcinoma" was first introduced by Liebow in 1960 due to confusion over true cell type.It comes from two cell types. columnar epithelium similar to bronchial cells and cuboidal type reminiscent of type 2 pneumocytes.
Classification
- Bronchoalveolar Carcinoma may be classified according to pathology into fo subtypes/groups:
Pathology of lung adenocarcinomas according to previous 2004 WHO and current IASLC/ATS/ERS classifications
| 2004 WHO classification |
| Mixed subtype |
| Acinar |
| Papillary |
| BAC |
| Non mucinous |
| Mucinous |
| Mixed |
| Solid adenocarcinoma |
| Colloid |
| Fetal |
| Mucinous cystadenocarcinoma |
| Signet-ring |
| Clear-cell |
| Major changes in the new IASLC/ATS/ERS classification |
| Discontinuation of the term BAC |
| Discontinuation of the mixed subtype |
| Comprehensive pathologic subtyping in 5% increments and classification of adenocarcinomas according to the predominant subtype |
| Introduction of AIS and MIA as new entities |
| Introduction of micropapillary adenocarcinoma as a predominant subtype |
| Introduction of lepidic predominant adenocarcinoma and lepidic growth as new terminologies |
| Exclusion of signet-ring and clear cell adenocarcinomas |
| IASLC/ATS/ERS classification |
| Pre-invasive lesions |
| Atypical adenomatous hyperplasia |
| AIS |
| Non-mucinous |
| Mucinous |
| Mixed |
| MIA |
| Non-mucinous |
| Mucinous |
| Mixed |
| Invasive adenocarcinomas |
| Lepidic predominant |
| Acinar predominant |
| Papillary predominant |
| Micropapillary predominant |
| Solid predominant with mucin production |
| Variants of invasive adenocarcinomas |
| IMA |
| Colloid |
| Fetal |
| Enteric |
WHO, World Health Organization; IASLC, International Association for the Study of Lung Cancer; ATS, American Thoracic Society; ERS, European Respiratory Society; BAC, bronchioloalveolar carcinoma; AIS, adenocarcinoma in situ; MIA, minimally invasive adenocarcinoma; IMA, invasive mucinous adenocarcinoma.
Pathophysiology
- In 2011, the term bronchoalveolar carcinoma is discontinued and new terms adenocarcinoma in situ and minimally invasive adenocarcinoma replaced the term BAC,
| Type | Subtypes | Cell Type | Comments |
|---|---|---|---|
| Adenocarcinoma in Situ |
|
Non-Mucinous:
Mucinous:
|
|
| Minimally Invasive Adenocarcinoma |
|
|
|
Differentiating Bronchoalveolar carcinoma from other Diseases
- BAC must be differentiated from other diseases that cause cough, hemoptysis, and solitary nodule on X-Ray such as:
- Malignant and benign lesion
- Infection e.g pulmonary tuberculosis
- Congenital
- Miscellaneous e.g Wegener and lymphomatoid granulomatosis
Epidemiology and Demographics
- Bronchoalveolar carcinoma is a rare tumor, the incidence of BAC vary from 4-24% of all the primary lung malignancies. More newer studies suggest Adenocarcinoma in situ and minimally invasive carcinoma constitutes 2-14% of all the primary types of lung cancers.
Age
- Patients of all age groups may develop BAC.
- BAC is more commonly observed among patients of middle aged group.
Gender
- Bronchoalveolar Carcinoma affects men and women disproportionately.
- Women are more commonly affected with bronchoalveolar carcinoma than men.
Race
- Bronchoalveolar Carcinoma usually affects individuals of the Asian race.
Risk Factors
- Common risk factors in the development of BAC are Asian race, women gender, and pulmonary fibrosis.
Lung cancer Screening
The U.S. Preventive Services Task Force recommends annual lung cancer screening with low density CT Scan for people who has history of,
- Have a 30 pack per year or more smoking history, and
- Current smoker or left smoking within the past 15 years, and
- Are aged between 55 and 80 years old.
Natural History, Complications and Prognosis
- The majority of patients with BAC remain asymptomatic for many years.
- Late clinical features include cough, mucus production, and persistent chest pain.
- If left untreated,patients with BAC may progress to invasive adenocarcinoma.
- Prognosis is generally good, and the 5 survival rate of patients with BAC is approximately.
- Prognosis of BAC depends on the histologic type. Non-mucinous AIS has better prognosis than mucinous type AIS.
- Mixed type has far worse survival rate than either of the monophasic form.
Diagnosis
Clinical Features
Bronchoalveolar carcinoma is usually asymptomatic and takes a very long time before becoming symptomatic. BAC may cause large quantities of mucus production, patients may present with bronchorrhea.
Solitary pulmonary nodule on Chest X-Ray that does not resolve despite taking antimicrobial therapy should be evaluated further for BAC.
CT or guided biopsy should be done in such cases. to reach the definite diagnosis.
Diagnostic Criteria
- The diagnostic criteria for bronchoalveolar carcinoma have changed over time. According to new 2011 IASLC/ATS recommendations, adopted in the 2015 WHO guidelines, use the following criteria for bronchoalveolar carcinoma
- Localized small tumor < 3 cm
- pure "lepidic growth"
- No stromal, vascular or pleural invasion
- Nuclear atypia absent/minimal in both mucinous/non-mucinous AIS
- Septal broadening with sclerosis (non-mucinous type)
- No spread through air spaces
Symptoms
- Bronchoalveolar carcinoma is usually asymptomatic because presence of symptoms are usually an indication of an advanced disease.
- Symptoms of BAC may include the following:
- Cough
- Sputum
- Hemoptysis
- Chest pain
- Weakness
- loss of appetite
- Repeated Lung infections like pneumonia and bronchitis
Physical Examination
- Patients with BAC usually appear
- Physical examination may be remarkable for:
- Low grade fever
- Cachexia
- bronchorrhea
- Other signs like dyspnea, pleural effusion and enlargement of lymph nodes can occur in advanced stage disease.
Laboratory Findings
- There are no specific laboratory findings associated with BAC. But, these lab findings can be helpful in patients with advanced diseases,
| Test | Comments |
|---|---|
| CBC | To rule out neutropenic fever in patients taking chemotherapy. |
| Liver function test (LFTs) | Insignificant except in advanced disease. |
| Serum electrolytes | To check for hyponatremia to rule out SIADH |
| Arterial Blood Gases (ABGs) | To detect respiratory failure in sick patient. |
| Serum Calcium | Hypercalcemia can occur due to Parathyroid hormone related protein (PTH-rP) |
| Serum PTH | To check for cause of hypercalcemia. It helps to differentiate whether the high calcium level is due to hyperparathyroidism or paraneoplastic syndrome (PTH-rP) |
Imaging Findings
- There are three radiologic findings associated with bronchoalveolar carcinoma are:
- Solitary nodule- most common
- Consolidation
- Multinodular opacities
- The nodular form is the commonest and can not be differentiated from other adenocarcinoma subtypes on plain X-ray.
- CT scan is imaging modality of the choice for bronchoalveolar carcinoma.
- Non-Mucinous BAC: It appears as solid nodule surrounded by ground glass opacification- Fried egg sign
- Mucinous BAC: It appears as single solid nodule
Bronchoalveolar carcinoma CT scan
- Subtype of adenocarcinoma[1]
- Single pulmonary nodule or mass
- Multicentric or diffuse disease
- Localized area of parenchymal consolidation
- Bubble-like areas of low attenuation within the mass are a characteristic finding
- Hilar and mediastinal lymphadenopathy is uncommon
- Persistent peripheral consolidation with associated nodules
-
CXR- Bronchoalveolar Carcinoma
-
CT SCAN: Bronchoalveolar Carcinoma
-
CT SCAN: Bronchoalveolar Carcinoma
Other Diagnostic Studies
- BAC may also be differentiated from invasive adenocarcinoma by using magnetic resonance imaging.
- Image guided per-cutaneous fine needle aspiration biopsy or core biopsy can be used to get molecular characteristic of the tumor.
- ECG can be done to rule out other causes of chest pain.
Treatment
Medical Therapy
- Non-Mucinous BAC responds well to targeted chemotherapy like epidermal growth factor receptor tyrosine kinase inhibitors erlotinib and gefitinib.
- Patient with non-resectable tumor can also benefit from erlotinib and gefitinib than other subtypes of non small cell lung carcinoma.
- Mucinous BAC are highly associated with K-RAS mutation and wild-type EGFR and does not respond well to EGFR tyrosine kinase inhibitor.
Surgery
- Surgery is the mainstay of therapy for bronchoalveolar carcinoma.
- Pneumonectomy or lobectomy in conjunction with ipsilateral lymphadenectomy is the most common approach to the treatment of BAC.
Prevention
- Effective measures for the primary prevention of Lung cancer include smoking cessation, avoid passive smoking, and taking precautionary measures to avoid exposure to harmful particles in work places.
See also, Lung cancer screening Lung Cancer Screening Decision Tool
References
- ↑ Gandara, David R.; Aberle, Denise; Lau, Derick; Jett, James; Akhurst, Tim; Mulshine, James; Berg, Christine; Patz, Edward F. (2006). "Radiographic Imaging of Bronchioloalveolar Carcinoma: Screening, Patterns of Presentation and Response Assessment". Journal of Thoracic Oncology. 1 (9): S20–S26. doi:10.1016/S1556-0864(15)30005-8. ISSN 1556-0864.