Rimabotulinumtoxinb: Difference between revisions
No edit summary |
m (Protected "Rimabotulinumtoxinb": Bot: Protecting all pages from category Drug ([Edit=Allow only administrators] (indefinite) [Move=Allow only administrators] (indefinite))) |
||
| (18 intermediate revisions by one other user not shown) | |||
| Line 5: | Line 5: | ||
|drugClass=neurotoxic protein | |drugClass=neurotoxic protein | ||
|indicationType=treatment | |indicationType=treatment | ||
|indication=adults with cervical dystonia to reduce the severity of abnormal head position and neck pain associated with cervical dystonia | |indication=adults with [[cervical dystonia]] to reduce the severity of abnormal head position and neck pain associated with [[cervical dystonia]] | ||
|hasBlackBoxWarning=Yes | |hasBlackBoxWarning=Yes | ||
|adverseReactions=dry mouth, dysphagia, dyspepsia, and injection site pain | |adverseReactions=[[dry mouth]], [[dysphagia]], [[dyspepsia]], and injection site pain | ||
|blackBoxWarningTitle=<span style="color:#FF0000;">DISTANT SPREAD OF TOXIN EFFECT</span> | |blackBoxWarningTitle=<span style="color:#FF0000;">DISTANT SPREAD OF TOXIN EFFECT</span> | ||
|blackBoxWarningBody=<i><span style="color:#FF0000;">Postmarketing reports indicate that the effects of | |blackBoxWarningBody=<i><span style="color:#FF0000;">Postmarketing reports indicate that the effects of rimabotulinumtoxinb and all botulinum toxin products may spread from the area of injection to produce symptoms consistent with botulinum toxin effects. These may include asthenia, generalized muscle weakness, diplopia, blurred vision, ptosis, dysphagia, dysphonia, dysarthria, urinary incontinence, and breathing difficulties. These symptoms have been reported hours to weeks after injection. Swallowing and breathing difficulties can be life threatening and there have been reports of death. The risk of symptoms is probably greatest in children treated for spasticity but symptoms can also occur in adults treated for spasticity and other conditions, particularly in those patients who have underlying conditions that would predispose them to these symptoms. In unapproved uses, including spasticity in children and adults, and in approved indications, cases of spread of effect have occurred at doses comparable to those used to treat cervical dystonia and at lower doses.</span></i> | ||
|fdaLIADAdult====Indications=== | |fdaLIADAdult====Indications=== | ||
* | *Rimabotulinumtoxinb is indicated for the treatment of adults with [[cervical dystonia]] to reduce the severity of abnormal head position and neck pain associated with [[cervical dystonia]]. | ||
===Dosage=== | ===Dosage=== | ||
The recommended initial dose of | *The recommended initial dose of rimabotulinumtoxinb for patients with a prior history of tolerating [[botulinum toxin]] injections is 2,500 to 5,000 Units divided among affected muscles. Patients without a prior history of tolerating botulinum toxin injections should receive a lower initial dose. Subsequent dosing should be optimized according to the patient's individual response. Rimabotulinumtoxinb should be administered by physicians familiar and experienced in the assessment and management of patients with CD. | ||
The method described for performing the potency assay is specific to Solstice Neurosciences' manufacture of | *The method described for performing the potency assay is specific to Solstice Neurosciences' manufacture of rimabotulinumtoxinb. Due to differences in the specific details of this assay such as the vehicle, dilution scheme and laboratory protocols for various potency assays, Units of biological activity of rimabotulinumtoxinb cannot be compared to or converted into units of any other [[botulinum toxin]] or any toxin assessed with any other specific assay method. Therefore, differences in species' sensitivities to different botulinum neurotoxin serotypes preclude extrapolation of animal dose-activity relationships to human dose estimates. | ||
The duration of effect in patients responding to | *The duration of effect in patients responding to rimabotulinumtoxinb treatment has been observed in studies to be between 12 and 16 weeks at doses of 5,000 Units or 10,000 Units. | ||
|offLabelAdultGuideSupport=There is limited information regarding <i>Off-Label Guideline-Supported Use</i> of Rimabotulinumtoxinb in adult patients. | |offLabelAdultGuideSupport=*There is limited information regarding <i>Off-Label Guideline-Supported Use</i> of Rimabotulinumtoxinb in adult patients. | ||
|offLabelAdultNoGuideSupport=There is limited information regarding <i>Off-Label Non–Guideline-Supported Use</i> of Rimabotulinumtoxinb in adult patients. | |offLabelAdultNoGuideSupport=*There is limited information regarding <i>Off-Label Non–Guideline-Supported Use</i> of Rimabotulinumtoxinb in adult patients. | ||
|fdaLIADPed=Safety and effectiveness in pediatric patients have not been established. | |fdaLIADPed=*Safety and effectiveness in pediatric patients have not been established. | ||
|offLabelPedGuideSupport=There is limited information regarding <i>Off-Label Guideline-Supported Use</i> of Rimabotulinumtoxinb in pediatric patients. | |offLabelPedGuideSupport=*There is limited information regarding <i>Off-Label Guideline-Supported Use</i> of Rimabotulinumtoxinb in pediatric patients. | ||
|offLabelPedNoGuideSupport=There is limited information regarding <i>Off-Label Non–Guideline-Supported Use</i> of Rimabotulinumtoxinb in pediatric patients. | |offLabelPedNoGuideSupport=*There is limited information regarding <i>Off-Label Non–Guideline-Supported Use</i> of Rimabotulinumtoxinb in pediatric patients. | ||
|contraindications= | |contraindications=*Rimabotulinumtoxinb is contraindicated in patients with a known [[hypersensitivity]] to any [[botulinum toxin]] preparation or to any of the components in the formulation. | ||
*Rimabotulinumtoxinb is contraindicated for use in patients with infection at the proposed injection site(s). | |||
|warnings=Lack of Interchangeability between Botulinum Toxin Products | |warnings=====Lack of Interchangeability between Botulinum Toxin Products==== | ||
The potency Units of | *The potency Units of rimabotulinumtoxinb are specific to the preparation and assay method utilized. They are not interchangeable with other preparations of [[botulinum toxin]] products and, therefore, units of biological activity of rimabotulinumtoxinb cannot be compared to or converted into units of any other botulinum toxin products assessed with any other specific assay method. | ||
Spread of Toxin Effect | ====Spread of Toxin Effect==== | ||
Postmarketing safety data from | *Postmarketing safety data from rimabotulinumtoxinb and other approved [[botulinum toxin]]s suggest that botulinum toxin effects may, in some cases, be observed beyond the site of local injection. The symptoms are consistent with the mechanism of action of botulinum toxin and may include [[asthenia]], generalized muscle weakness, [[diplopia]], [[blurred vision]], [[ptosis]], [[dysphagia]], [[dysphonia]], [[dysarthria]], [[urinary incontinence]], and [[breathing difficulties]]. These symptoms have been reported hours to weeks after injection. Swallowing and [[breathing difficulties]] can be life threatening and there have been reports of death related to spread of toxin effects. The risk of symptoms is probably greatest in children treated for spasticity but symptoms can also occur in adults treated for spasticity and other conditions, and particularly in those patients who have underlying conditions that would predispose them to these symptoms. In unapproved uses, including spasticity in children and adults, and in approved indications, symptoms consistent with spread of toxin effect have been reported at doses comparable to or lower than doses used to treat [[cervical dystonia]]. | ||
Dysphagia and Breathing Difficulties in Treatment of Cervical Dystonia | ====Dysphagia and Breathing Difficulties in Treatment of Cervical Dystonia==== | ||
Treatment with | *Treatment with rimabotulinumtoxinb and other [[botulinum toxin]] products can result in swallowing or [[breathing difficulties]]. Patients with pre-existing swallowing or [[breathing difficulties]] may be more susceptible to these complications. In most cases, this is a consequence of weakening of muscles in the area of injection that are involved in breathing or swallowing. When distant effects occur, additional respiratory muscles may be involved. | ||
Deaths as a complication of severe dysphagia have been reported after treatment with botulinum toxin. | *Deaths as a complication of severe [[dysphagia]] have been reported after treatment with [[botulinum toxin]]. [[dysphagia]] may persist for several months, and require use of a feeding tube to maintain adequate nutrition and hydration. Aspiration may result from severe [[dysphagia]] and is a particular risk when treating patients in whom swallowing or respiratory function is already compromised. | ||
Treatment of cervical dystonia with botulinum | *Treatment of [[cervical dystonia]] with [[botulinum toxin]]s may weaken neck muscles that serve as accessory muscles of ventilation. This may result in a critical loss of breathing capacity in patients with respiratory disorders who may have become dependent upon these accessory muscles. There have been postmarketing reports of serious breathing difficulties, including respiratory failure, in [[cervical dystonia]] patients. Patients treated with [[botulinum toxin]] may require immediate medical attention should they develop problems with swallowing, speech or respiratory disorders. These reactions can occur within hours to weeks after injection with botulinum toxin. | ||
Pre-Existing Neuromuscular Disorders | ====Pre-Existing Neuromuscular Disorders==== | ||
Individuals with peripheral motor neuropathic diseases, amyotrophic lateral sclerosis, or neuromuscular junctional disorders (e.g., myasthenia gravis or Lambert-Eaton syndrome) should be monitored particularly closely when given botulinum toxin. Patients with neuromuscular disorders may be at increased risk of clinically significant effects including severe dysphagia and respiratory compromise from typical doses of | *Individuals with peripheral motor neuropathic diseases, [[amyotrophic lateral sclerosis]], or neuromuscular junctional disorders (e.g., [[myasthenia gravis]] or [[Lambert-Eaton syndrome]]) should be monitored particularly closely when given [[botulinum toxin]]. Patients with neuromuscular disorders may be at increased risk of clinically significant effects including severe [[dysphagia]] and respiratory compromise from typical doses of rimabotulinumtoxinb. | ||
Human Albumin | ====Human Albumin==== | ||
This product contains albumin, a derivative of human blood. Based on effective donor screening and product manufacturing processes, it carries an extremely remote risk for transmission of viral diseases. A theoretical risk for transmission of Creutzfeldt-Jakob disease (CJD) also is considered extremely remote. No cases of transmission of viral diseases or CJD have ever been identified for albumin. | *This product contains albumin, a derivative of human blood. Based on effective donor screening and product manufacturing processes, it carries an extremely remote risk for transmission of viral diseases. A theoretical risk for transmission of [[Creutzfeldt-Jakob disease]] (CJD) also is considered extremely remote. No cases of transmission of viral diseases or CJD have ever been identified for albumin. | ||
===Precations=== | ===Precations=== | ||
Only 9 subjects without a prior history of tolerating injections of type A botulinum toxin have been studied. Treatment of botulinum toxin naïve patients should be initiated at lower doses of | *Only 9 subjects without a prior history of tolerating injections of type A [[botulinum toxin]] have been studied. Treatment of botulinum toxin naïve patients should be initiated at lower doses of rimabotulinumtoxinb. | ||
|clinicalTrials=Overview | |clinicalTrials=====Overview==== | ||
The most commonly reported adverse events associated with | *The most commonly reported adverse events associated with rimabotulinumtoxinb treatment in all studies were [[dry mouth]], [[dysphagia]], [[dyspepsia]], and injection site pain. [[dry mouth]] and [[dysphagia]] were the adverse reactions most frequently resulting in discontinuation of treatment. There was an increased incidence of [[dysphagia]] with increased dose in the sternocleidomastoid muscle. The incidence of [[dry mouth]] showed some dose-related increase with doses injected into the splenius capitis, trapezius and sternocleidomastoid muscles. | ||
Only nine subjects without a prior history of tolerating injections of type A botulinum toxin have been studied. Adverse event rates have not been adequately evaluated in these patients, and may be higher than those described in Table 3. | *Only nine subjects without a prior history of tolerating injections of type A [[botulinum toxin]] have been studied. Adverse event rates have not been adequately evaluated in these patients, and may be higher than those described in Table 3. | ||
Discussion | ====Discussion==== | ||
Adverse reaction rates observed in the clinical trials for a product cannot be directly compared to rates in clinical trials for another product and may not reflect the rates observed in actual clinical practice. However, adverse reaction information from clinical trials does provide a basis for identifying the adverse events that appear to be related to drug use and for approximating rates. | *Adverse reaction rates observed in the clinical trials for a product cannot be directly compared to rates in clinical trials for another product and may not reflect the rates observed in actual clinical practice. However, adverse reaction information from clinical trials does provide a basis for identifying the adverse events that appear to be related to drug use and for approximating rates. | ||
*Rimabotulinumtoxinb was studied in both placebo controlled single treatment studies and uncontrolled repeated treatment studies; most treatment sessions and patients were in the uncontrolled studies. The data described below reflect exposure to rimabotulinumtoxinb at varying doses in 570 subjects, including more than 300 patients with 4 or more treatment sessions. Most treatment sessions were at doses of 12,500 Units or less. There were 57 patients administered a dose of 20,000 or 25,000 Units. All but nine patients had a prior history of receiving type A [[botulinum toxin]] and adequately tolerating the treatment to have received repeated doses. | |||
The rates of adverse events and association with | *The rates of adverse events and association with rimabotulinumtoxinb are best assessed in the results from the placebo controlled studies of a single treatment session with active monitoring. The data in Table 3 reflect those adverse events occurring in at least 5% of patients exposed to rimabotulinumtoxinb treatment in pooled placebo controlled clinical trials. Annual rates of adverse events are higher in the overall data which includes longer duration follow-up of patients with repeated treatment experience. The mean age of the population in these studies was 55-years-old with approximately 66% being female. Most of the patients studied were Caucasian and all had [[cervical dystonia]] that was rated as moderate to severe in severity. | ||
[[File:Rimabotulinumtoxinb1.png|thumb|none|400px|This image is provided by the National Library of Medicine.]] | [[File:Rimabotulinumtoxinb1.png|thumb|none|400px|This image is provided by the National Library of Medicine.]] | ||
In the overall clinical trial experience with | *In the overall clinical trial experience with rimabotulinumtoxinb (570 patients, including the uncontrolled studies), most cases of [[dry mouth]] or [[dysphagia]] were reported as mild or moderate in severity. Severe [[dysphagia]] was reported by 3% of patients. Severe [[dry mouth]] was reported by 6% of patients. [[dysphagia]] and [[dry mouth]] were the most frequent adverse events reported as a reason for discontinuation from repeated treatment studies. These adverse events led to discontinuation from further treatments with rimabotulinumtoxinb in some patients even when not reported as severe. | ||
The following additional adverse events were reported in 2% or greater of patients participating in any of the clinical studies (COSTART terms, by body system): | *The following additional adverse events were reported in 2% or greater of patients participating in any of the clinical studies (COSTART terms, by body system): | ||
Body as a Whole: allergic reaction, fever, headache related to injection, chest pain, chills, hernia, malaise, abscess, cyst, neoplasm, viral infection | :*Body as a Whole: allergic reaction, fever, headache related to injection, chest pain, chills, hernia, malaise, abscess, cyst, neoplasm, viral infection | ||
|postmarketing=The following adverse events have been reported during postmarketing use for approved and unapproved indications: angioedema, urticaria, rash and constipation. | :*Musculoskeletal: arthritis, joint disorder | ||
|drugInteractions=Co-administration of | :*Cardiovascular System: migraine; Respiratory: dyspnea, lung disorder, pneumonia | ||
:*Nervous System: anxiety, tremor, hyperesthesia, somnolence, confusion, pain related to CD/torticollis, vertigo, vasodilation | |||
:*Digestive System: gastrointestinal disorder, vomiting, glossitis, stomatitis, tooth disorder | |||
:*Skin and Appendages: pruritis | |||
:*Urogenital System: urinary tract infection, cystitis, vaginal moniliasis | |||
:*Special Senses: amblyopia, otitis media, abnormal vision, taste perversion, tinnitus | |||
:* Metabolic and Nutritional Disorders: peripheral edema, edema, hypercholesterolemia | |||
:* Hemic and Lymphatic System: ecchymosis. | |||
|postmarketing=*The following adverse events have been reported during postmarketing use for approved and unapproved indications: angioedema, urticaria, rash and constipation. | |||
|drugInteractions=*Co-administration of rimabotulinumtoxinb and aminoglycosides or other agents interfering with neuromuscular transmission (e.g., curare-like compounds) should only be performed with caution as the effect of the toxin may be potentiated. | |||
The effect of administering different botulinum neurotoxin serotypes at the same time or within less than 4 months of each other is unknown. However, neuromuscular paralysis may be potentiated by co-administration or overlapping administration of different botulinum toxin serotypes. | *The effect of administering different botulinum neurotoxin serotypes at the same time or within less than 4 months of each other is unknown. However, neuromuscular paralysis may be potentiated by co-administration or overlapping administration of different [[botulinum toxin]] serotypes. | ||
|FDAPregCat=C | |FDAPregCat=C | ||
|useInPregnancyFDA=Animal reproduction studies have not been conducted with | |useInPregnancyFDA=*Animal reproduction studies have not been conducted with rimabotulinumtoxinb. It is also not known whether rimabotulinumtoxinb can cause fetal harm when administered to a pregnant woman or can affect reproduction capacity. Rimabotulinumtoxinb should be given to a pregnant woman only if clearly needed. | ||
|useInNursing=It is not known whether this drug is excreted in human milk. Because many drugs are excreted in human milk, caution should be exercised when | |useInNursing=*It is not known whether this drug is excreted in human milk. Because many drugs are excreted in human milk, caution should be exercised when rimabotulinumtoxinb is administered to a nursing woman. | ||
|useInPed=Safety and effectiveness in pediatric patients have not been established. | |useInPed=*Safety and effectiveness in pediatric patients have not been established. | ||
|useInGeri=In the controlled studies summarized in CLINICAL STUDIES, for | |useInGeri=*In the controlled studies summarized in CLINICAL STUDIES, for rimabotulinumtoxinb treated patients, 152 (74.5%) were under the age of 65, and 52 (25.5%) were aged 65 or greater. For these age groups, the most frequent reported adverse events occurred at similar rates in both age groups. Efficacy results did not suggest any large differences between these age groups. | ||
Very few patients aged 75 or greater were enrolled, therefore no conclusions regarding the safety and efficacy of | Very few patients aged 75 or greater were enrolled, therefore no conclusions regarding the safety and efficacy of rimabotulinumtoxinb within this age group can be determined. | ||
|overdose=Excessive doses of | |administration=*Intramuscular. | ||
|monitoring=*In the event of overdose, the patient should be medically monitored for symptoms of excessive muscle weakness or muscle paralysis. | |||
*Monitore individuals with peripheral motor neuropathic diseases, amyotrophic lateral sclerosis, or neuromuscular junctional disorders when given [[botulinum toxin]]. | |||
|IVCompat=*There is limited information regarding <i>IV Compatibility</i>. | |||
|overdose=*Excessive doses of rimabotulinumtoxinb may be expected to produce neuromuscular weakness with a variety of symptoms. Respiratory support may be required where excessive doses cause paralysis of respiratory muscles. In the event of overdose, the patient should be medically monitored for symptoms of excessive muscle weakness or muscle paralysis. Symptomatic treatment may be necessary. | |||
Symptoms of overdose are likely not to be present immediately following injection. Should accidental injection or oral ingestion occur, the person should be medically supervised for several weeks for signs and symptoms of excessive muscle weakness or muscle paralysis. | *Symptoms of overdose are likely not to be present immediately following injection. Should accidental injection or oral ingestion occur, the person should be medically supervised for several weeks for signs and symptoms of excessive muscle weakness or muscle paralysis. | ||
In the event of overdose, antitoxin raised against botulinum toxin is available from the Centers for Disease Control and Prevention (CDC) in Atlanta, GA. However, the antitoxin will not reverse any botulinum toxin-induced effects already apparent by the time of antitoxin administration. In the event of suspected or actual cases of botulinum toxin poisoning, please contact your local or state Health Department to process a request for antitoxin through the CDC. | *In the event of overdose, antitoxin raised against [[botulinum toxin]] is available from the Centers for Disease Control and Prevention (CDC) in Atlanta, GA. However, the antitoxin will not reverse any botulinum toxin-induced effects already apparent by the time of antitoxin administration. In the event of suspected or actual cases of botulinum toxin poisoning, please contact your local or state Health Department to process a request for antitoxin through the CDC. | ||
| | |mechAction=*The seven serologically distinct botulinum neurotoxins, designated A through G, share a common structural organization consisting of one Heavy Chain and one Light Chain polypeptide linked by a single disulfide bond. These toxins inhibit acetylcholine release at the neuromuscular junction via a three stage process: 1) Heavy Chain mediated neurospecific binding of the toxin, 2) internalization of the toxin by receptor-mediated endocytosis, and 3) ATP and pH dependent translocation of the Light Chain to the neuronal cytosol where it acts as a zinc-dependent endoprotease cleaving polypeptides essential for neurotransmitter release. rimabotulinumtoxinb specifically has been demonstrated to cleave synaptic Vesicle Associated Membrane Protein (VAMP, also known as synaptobrevin) which is a component of the protein complex responsible for docking and fusion of the synaptic vesicle to the presynaptic membrane, a necessary step to neurotransmitter release. | ||
| | |structure=*RimabotulinumtoxinB injection is a sterile liquid formulation of a purified neurotoxin that acts at the neuromuscular junction to produce flaccid paralysis. The neurotoxin is produced by fermentation of the bacterium Clostridium botulinum type B (Bean strain) and exists in noncovalent association with hemagglutinin and nonhemagglutinin proteins as a neurotoxin complex. The neurotoxin complex is recovered from the fermentation process and purified through a series of precipitation and chromatography steps. | ||
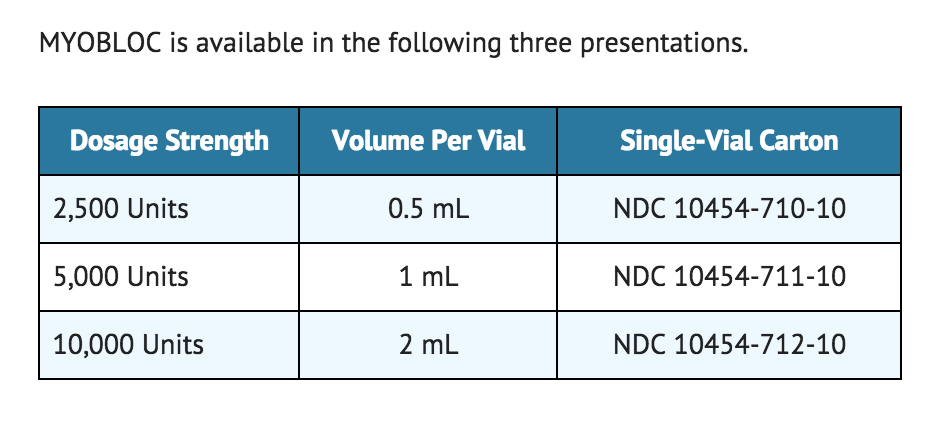
MYOBLOC is available in the following three presentations. | *Rimabotulinumtoxinb is provided as a clear and colorless to light-yellow sterile injectable solution in 3.5-mL glass vials. Each single-use vial of formulated rimabotulinumtoxinb contains 5,000 Units of [[botulinum toxin]] type B per milliliter in 0.05% human serum albumin, 0.01 M sodium succinate, and 0.1 M sodium chloride at approximately pH 5.6. | ||
[[File: | |||
*One unit of rimabotulinumtoxinb corresponds to the calculated median lethal intraperitoneal dose (LD50) in mice. The method for performing the assay is specific to Solstice Neurosciences' manufacture of rimabotulinumtoxinb. Due to differences in specific details such as the vehicle, dilution scheme and laboratory protocols for various mouse LD50 assays, units of biological activity of rimabotulinumtoxinb cannot be compared to or converted into units of any other botulinum toxin or any toxin assessed with any other specific assay method. Therefore, differences in species sensitivities to different botulinum neurotoxin serotypes preclude extrapolation of animal dose-activity relationships to human dose estimates. The specific activity of rimabotulinumtoxinb ranges between 70 to 130 Units/ng. | |||
|PD=*There is limited information regarding <i>pharmacodynamics</i> | |||
|PK=*Using currently available analytical technology, it is not possible to detect rimabotulinumtoxinb in the peripheral blood following intramuscular injection at the recommended doses. | |||
|nonClinToxic=*No long-term carcinogenicity studies in animals have been performed. | |||
|clinicalStudies=*Two phase 3, randomized, multi-center, double-blind, placebo controlled studies of the treatment of [[cervical dystonia]] were conducted. Both studies enrolled only adult patients who had a history of receiving botulinum toxin type A in an open label manner, with a perceived good response and tolerable adverse effects. Study #301 enrolled patients who were perceived as having an acceptable response to type A toxin, while Study #302 enrolled only patients who had secondarily lost responsiveness to type A toxin. Other eligibility criteria common to both studies were that all subjects had moderate or greater severity of [[cervical dystonia]] with at least 2 muscles involved, no neck contractures or other causes of decreased neck range of motion, and no history of any other neuromuscular disorder. Subjects in Study #301 were randomized to receive placebo, 5,000 Units or 10,000 Units of rimabotulinumtoxinb, and subjects in Study #302 were randomized to receive placebo or 10,000 Units of rimabotulinumtoxinb. Study agent was administered to subjects in a single treatment session by investigators who selected 2 to 4 muscles per subject from the following: Splenius capitis, Sternocleidomastoid, Levator scapulae, Trapezius, Semispinalis capitis, and Scalene muscles. The total dose was divided between the selected muscles, and from 1 to 5 injections were made per muscle. There were 109 subjects enrolled into Study #301, and 77 into Study #302. Patient evaluations continued for 16 weeks post injection. | |||
*The primary efficacy outcome variable for both studies was the Toronto Western Spasmodic Torticollis Rating Scale (TWSTRS)-Total Score (scale range of possible scores is 0–87) at Week 4. TWSTRS is comprised of three sub-scales which examine 1) Severity—the severity of the patient's abnormal head position; 2) Pain—the severity and duration of pain due to the dystonia; and 3) Disability— the effects of the abnormal head position and pain on a patient's activities. The secondary endpoints were the Patient Global and Physician Global Assessments of change at Week 4. Both Global Assessments used a 100-point visual-analog scale (VAS). The Patient Global Assessment allows patients to indicate how they feel at the time of their evaluation compared to the pre-injection baseline. Likewise, the Physician Global Assessment indicates the physician's assessment of a patient's change from baseline to Week 4. Scores of 50 indicate no change, 0 much worse, and 100 much better. Results of comparisons of the primary and secondary efficacy variables are summarized in Table 1. | |||
[[File:Rimabotulinumtoxinb8.png|thumb|none|400px|This image is provided by the National Library of Medicine.]] | |||
*There were no statistically significant differences in results between the 5,000 Units and 10,000 Units doses in Study #301. Exploratory analyses of these two studies suggested that the majority of patients who showed a beneficial response by Week 4 had returned to their baseline status between Weeks 12 to 16 post injection. Although there was a rimabotulinumtoxinb associated decrease in pain, there remained many patients who experienced an increase in dystonia-related neck pain irrespective of treatment group. TWSTRS Total Score at Week 4 and Patient Global Assessment among subgroups by gender or age showed consistent treatment-associated effects across these subgroups. There were too few non-Caucasian patients enrolled to draw any conclusions regarding relative efficacy in racial subsets. | |||
*Rimabotulinumtoxinb was studied in two phase 2 dose ranging studies, Studies #08 and #09, which preceded the phase 3 studies. Studies #08 and #09 had a study design similar to the phase 3 studies, including eligibility criteria. Study #08 enrolled 85 subjects randomized between doses of placebo, 400 Units, 1,200 Units, or 2,400 Units (21 or 22 subjects per group). Study #09 enrolled 122 subjects and randomized between doses of placebo, 2,500 Units, 5,000 Units, and 10,000 Units (30 or 31 subjects per group). These studies demonstrated efficacy on the TWSTRS-Total, baseline to Week 4, at doses of 2,400 Units, 2,500 Units, 5,000 Units, and 10,000 Units. Study #08 showed mean improvement from baseline on the Week 4 TWSTRS for placebo and 2,400 Units of 2.0 and 8.5 points respectively (from baselines of 42.0 and 42.4 points). Study #09 showed mean improvement from baseline to Week 4 for placebo, 2,500 Units, 5,000 Units, and 10,000 Units of 3.3, 11.6, 12.5, and 16.4 points, respectively (from baselines of 45.5, 45.6, 45.2, and 47.5 points). Study #08 also indicated there is less response for doses below 2,400 Units. | |||
*Study #352 was an open label, intrapatient dose-escalation study of 3 treatment sessions where each patient with [[cervical dystonia]] sequentially received 10,000 Units, 12,500 Units, and 15,000 Units, at periods of 12 to 16 weeks between treatment sessions irrespective of their response to their previous dose. This study enrolled 145 patients, of whom 125 received all three treatments. Although this was an open label design where investigators and patients knew the dose at each treatment session, there were similar mean improvements on the TWSTRS-Total, from baseline to Week 4, for all three doses. | |||
*In the rimabotulinumtoxinb injected patients (n=112) of the phase 3 studies, 19% had 2 muscles injected, 48% had 3 muscles injected, and 33% had 4 muscles injected. Table 2 indicates the frequency of use for each of the permitted muscles, and the fraction of the total dose of the treatment injected into each muscle, for those patients in whom the muscle was injected. | |||
[[File:Rimabotulinumtoxinb9.png|thumb|none|400px|This image is provided by the National Library of Medicine.]] | |||
|howSupplied=*MYOBLOC is provided as a clear and colorless to light-yellow sterile injectable solution in single-use 3.5-mL glass vials. Each single-use vial of formulated MYOBLOC contains 5,000 Units1 of botulinum toxin type B per milliliter in 0.05% human serum albumin, 0.01 M sodium succinate, 0.1 M sodium chloride at approximately pH 5.6. | |||
*MYOBLOC is available in the following three presentations. | |||
[[File:Rimabotulinumtoxinb2.png|thumb|none|400px|This image is provided by the National Library of Medicine.]] | |||
|storage=*Store under refrigeration at 2°- 8°C (36°- 46°F). | |storage=*Store under refrigeration at 2°- 8°C (36°- 46°F). | ||
| Line 96: | Line 129: | ||
[[File:Rimabotulinumtoxinb5.jpeg|thumb|none|400px|This image is provided by the National Library of Medicine.]] | [[File:Rimabotulinumtoxinb5.jpeg|thumb|none|400px|This image is provided by the National Library of Medicine.]] | ||
[[File:Rimabotulinumtoxinb6.png|thumb|none|400px|This image is provided by the National Library of Medicine.]] | [[File:Rimabotulinumtoxinb6.png|thumb|none|400px|This image is provided by the National Library of Medicine.]] | ||
|fdaPatientInfo=The physician should provide a copy of the FDA-Approved Patient Medication Guide and review the contents with the patient. Patients should be advised to inform their doctor or pharmacist if they develop any unusual symptoms (including difficulty with swallowing, speaking or breathing), or if any existing symptom worsens. | |fdaPatientInfo=*The physician should provide a copy of the FDA-Approved Patient Medication Guide and review the contents with the patient. Patients should be advised to inform their doctor or pharmacist if they develop any unusual symptoms (including difficulty with swallowing, speaking or breathing), or if any existing symptom worsens. | ||
*Patients should be counseled that if loss of strength, muscle weakness, or impaired vision occur, they should avoid driving a car or engaging in other potentially hazardous activities. | |||
[[File:Rimabotulinumtoxinb7.png|thumb|none|400px|This image is provided by the National Library of Medicine.]] | |||
|alcohol=Alcohol-Rimabotulinumtoxinb interaction has not been established. Talk to your doctor about the effects of taking alcohol with this medication. | |alcohol=*Alcohol-Rimabotulinumtoxinb interaction has not been established. Talk to your doctor about the effects of taking alcohol with this medication. | ||
|brandNames=*MYOBLOC ®<ref>{{Cite web | title = MYOBLOC- rimabotulinumtoxinb injection, solution | url = http://dailymed.nlm.nih.gov/dailymed/drugInfo.cfm?setid=675cb354-9d13-482e-8ac2-22f709c58b4f}}</ref> | |||
|lookAlike=*There is limited information regarding <i>Look-Alike Drug Names</i>. | |||
}} | }} | ||
[[Category:Muscle relaxants]] | |||
[[Category:Neurotoxins]] | |||
[[Category:Plastic surgery]] | |||
[[Category:Drug]] | |||
[[Category:EC 3.4.24]] | |||
Latest revision as of 17:04, 20 August 2015
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]; Associate Editor(s)-in-Chief: Turky Alkathery, M.D. [2]
Disclaimer
WikiDoc MAKES NO GUARANTEE OF VALIDITY. WikiDoc is not a professional health care provider, nor is it a suitable replacement for a licensed healthcare provider. WikiDoc is intended to be an educational tool, not a tool for any form of healthcare delivery. The educational content on WikiDoc drug pages is based upon the FDA package insert, National Library of Medicine content and practice guidelines / consensus statements. WikiDoc does not promote the administration of any medication or device that is not consistent with its labeling. Please read our full disclaimer here.
Black Box Warning
|
DISTANT SPREAD OF TOXIN EFFECT
See full prescribing information for complete Boxed Warning.
Postmarketing reports indicate that the effects of rimabotulinumtoxinb and all botulinum toxin products may spread from the area of injection to produce symptoms consistent with botulinum toxin effects. These may include asthenia, generalized muscle weakness, diplopia, blurred vision, ptosis, dysphagia, dysphonia, dysarthria, urinary incontinence, and breathing difficulties. These symptoms have been reported hours to weeks after injection. Swallowing and breathing difficulties can be life threatening and there have been reports of death. The risk of symptoms is probably greatest in children treated for spasticity but symptoms can also occur in adults treated for spasticity and other conditions, particularly in those patients who have underlying conditions that would predispose them to these symptoms. In unapproved uses, including spasticity in children and adults, and in approved indications, cases of spread of effect have occurred at doses comparable to those used to treat cervical dystonia and at lower doses.
|
Overview
Rimabotulinumtoxinb is a neurotoxic protein that is FDA approved for the treatment of adults with cervical dystonia to reduce the severity of abnormal head position and neck pain associated with cervical dystonia. There is a Black Box Warning for this drug as shown here. Common adverse reactions include dry mouth, dysphagia, dyspepsia, and injection site pain.
Adult Indications and Dosage
FDA-Labeled Indications and Dosage (Adult)
Indications
- Rimabotulinumtoxinb is indicated for the treatment of adults with cervical dystonia to reduce the severity of abnormal head position and neck pain associated with cervical dystonia.
Dosage
- The recommended initial dose of rimabotulinumtoxinb for patients with a prior history of tolerating botulinum toxin injections is 2,500 to 5,000 Units divided among affected muscles. Patients without a prior history of tolerating botulinum toxin injections should receive a lower initial dose. Subsequent dosing should be optimized according to the patient's individual response. Rimabotulinumtoxinb should be administered by physicians familiar and experienced in the assessment and management of patients with CD.
- The method described for performing the potency assay is specific to Solstice Neurosciences' manufacture of rimabotulinumtoxinb. Due to differences in the specific details of this assay such as the vehicle, dilution scheme and laboratory protocols for various potency assays, Units of biological activity of rimabotulinumtoxinb cannot be compared to or converted into units of any other botulinum toxin or any toxin assessed with any other specific assay method. Therefore, differences in species' sensitivities to different botulinum neurotoxin serotypes preclude extrapolation of animal dose-activity relationships to human dose estimates.
- The duration of effect in patients responding to rimabotulinumtoxinb treatment has been observed in studies to be between 12 and 16 weeks at doses of 5,000 Units or 10,000 Units.
Off-Label Use and Dosage (Adult)
Guideline-Supported Use
- There is limited information regarding Off-Label Guideline-Supported Use of Rimabotulinumtoxinb in adult patients.
Non–Guideline-Supported Use
- There is limited information regarding Off-Label Non–Guideline-Supported Use of Rimabotulinumtoxinb in adult patients.
Pediatric Indications and Dosage
FDA-Labeled Indications and Dosage (Pediatric)
- Safety and effectiveness in pediatric patients have not been established.
Off-Label Use and Dosage (Pediatric)
Guideline-Supported Use
- There is limited information regarding Off-Label Guideline-Supported Use of Rimabotulinumtoxinb in pediatric patients.
Non–Guideline-Supported Use
- There is limited information regarding Off-Label Non–Guideline-Supported Use of Rimabotulinumtoxinb in pediatric patients.
Contraindications
- Rimabotulinumtoxinb is contraindicated in patients with a known hypersensitivity to any botulinum toxin preparation or to any of the components in the formulation.
- Rimabotulinumtoxinb is contraindicated for use in patients with infection at the proposed injection site(s).
Warnings
|
DISTANT SPREAD OF TOXIN EFFECT
See full prescribing information for complete Boxed Warning.
Postmarketing reports indicate that the effects of rimabotulinumtoxinb and all botulinum toxin products may spread from the area of injection to produce symptoms consistent with botulinum toxin effects. These may include asthenia, generalized muscle weakness, diplopia, blurred vision, ptosis, dysphagia, dysphonia, dysarthria, urinary incontinence, and breathing difficulties. These symptoms have been reported hours to weeks after injection. Swallowing and breathing difficulties can be life threatening and there have been reports of death. The risk of symptoms is probably greatest in children treated for spasticity but symptoms can also occur in adults treated for spasticity and other conditions, particularly in those patients who have underlying conditions that would predispose them to these symptoms. In unapproved uses, including spasticity in children and adults, and in approved indications, cases of spread of effect have occurred at doses comparable to those used to treat cervical dystonia and at lower doses.
|
Lack of Interchangeability between Botulinum Toxin Products
- The potency Units of rimabotulinumtoxinb are specific to the preparation and assay method utilized. They are not interchangeable with other preparations of botulinum toxin products and, therefore, units of biological activity of rimabotulinumtoxinb cannot be compared to or converted into units of any other botulinum toxin products assessed with any other specific assay method.
Spread of Toxin Effect
- Postmarketing safety data from rimabotulinumtoxinb and other approved botulinum toxins suggest that botulinum toxin effects may, in some cases, be observed beyond the site of local injection. The symptoms are consistent with the mechanism of action of botulinum toxin and may include asthenia, generalized muscle weakness, diplopia, blurred vision, ptosis, dysphagia, dysphonia, dysarthria, urinary incontinence, and breathing difficulties. These symptoms have been reported hours to weeks after injection. Swallowing and breathing difficulties can be life threatening and there have been reports of death related to spread of toxin effects. The risk of symptoms is probably greatest in children treated for spasticity but symptoms can also occur in adults treated for spasticity and other conditions, and particularly in those patients who have underlying conditions that would predispose them to these symptoms. In unapproved uses, including spasticity in children and adults, and in approved indications, symptoms consistent with spread of toxin effect have been reported at doses comparable to or lower than doses used to treat cervical dystonia.
Dysphagia and Breathing Difficulties in Treatment of Cervical Dystonia
- Treatment with rimabotulinumtoxinb and other botulinum toxin products can result in swallowing or breathing difficulties. Patients with pre-existing swallowing or breathing difficulties may be more susceptible to these complications. In most cases, this is a consequence of weakening of muscles in the area of injection that are involved in breathing or swallowing. When distant effects occur, additional respiratory muscles may be involved.
- Deaths as a complication of severe dysphagia have been reported after treatment with botulinum toxin. dysphagia may persist for several months, and require use of a feeding tube to maintain adequate nutrition and hydration. Aspiration may result from severe dysphagia and is a particular risk when treating patients in whom swallowing or respiratory function is already compromised.
- Treatment of cervical dystonia with botulinum toxins may weaken neck muscles that serve as accessory muscles of ventilation. This may result in a critical loss of breathing capacity in patients with respiratory disorders who may have become dependent upon these accessory muscles. There have been postmarketing reports of serious breathing difficulties, including respiratory failure, in cervical dystonia patients. Patients treated with botulinum toxin may require immediate medical attention should they develop problems with swallowing, speech or respiratory disorders. These reactions can occur within hours to weeks after injection with botulinum toxin.
Pre-Existing Neuromuscular Disorders
- Individuals with peripheral motor neuropathic diseases, amyotrophic lateral sclerosis, or neuromuscular junctional disorders (e.g., myasthenia gravis or Lambert-Eaton syndrome) should be monitored particularly closely when given botulinum toxin. Patients with neuromuscular disorders may be at increased risk of clinically significant effects including severe dysphagia and respiratory compromise from typical doses of rimabotulinumtoxinb.
Human Albumin
- This product contains albumin, a derivative of human blood. Based on effective donor screening and product manufacturing processes, it carries an extremely remote risk for transmission of viral diseases. A theoretical risk for transmission of Creutzfeldt-Jakob disease (CJD) also is considered extremely remote. No cases of transmission of viral diseases or CJD have ever been identified for albumin.
Precations
- Only 9 subjects without a prior history of tolerating injections of type A botulinum toxin have been studied. Treatment of botulinum toxin naïve patients should be initiated at lower doses of rimabotulinumtoxinb.
Adverse Reactions
Clinical Trials Experience
Overview
- The most commonly reported adverse events associated with rimabotulinumtoxinb treatment in all studies were dry mouth, dysphagia, dyspepsia, and injection site pain. dry mouth and dysphagia were the adverse reactions most frequently resulting in discontinuation of treatment. There was an increased incidence of dysphagia with increased dose in the sternocleidomastoid muscle. The incidence of dry mouth showed some dose-related increase with doses injected into the splenius capitis, trapezius and sternocleidomastoid muscles.
- Only nine subjects without a prior history of tolerating injections of type A botulinum toxin have been studied. Adverse event rates have not been adequately evaluated in these patients, and may be higher than those described in Table 3.
Discussion
- Adverse reaction rates observed in the clinical trials for a product cannot be directly compared to rates in clinical trials for another product and may not reflect the rates observed in actual clinical practice. However, adverse reaction information from clinical trials does provide a basis for identifying the adverse events that appear to be related to drug use and for approximating rates.
- Rimabotulinumtoxinb was studied in both placebo controlled single treatment studies and uncontrolled repeated treatment studies; most treatment sessions and patients were in the uncontrolled studies. The data described below reflect exposure to rimabotulinumtoxinb at varying doses in 570 subjects, including more than 300 patients with 4 or more treatment sessions. Most treatment sessions were at doses of 12,500 Units or less. There were 57 patients administered a dose of 20,000 or 25,000 Units. All but nine patients had a prior history of receiving type A botulinum toxin and adequately tolerating the treatment to have received repeated doses.
- The rates of adverse events and association with rimabotulinumtoxinb are best assessed in the results from the placebo controlled studies of a single treatment session with active monitoring. The data in Table 3 reflect those adverse events occurring in at least 5% of patients exposed to rimabotulinumtoxinb treatment in pooled placebo controlled clinical trials. Annual rates of adverse events are higher in the overall data which includes longer duration follow-up of patients with repeated treatment experience. The mean age of the population in these studies was 55-years-old with approximately 66% being female. Most of the patients studied were Caucasian and all had cervical dystonia that was rated as moderate to severe in severity.

- In the overall clinical trial experience with rimabotulinumtoxinb (570 patients, including the uncontrolled studies), most cases of dry mouth or dysphagia were reported as mild or moderate in severity. Severe dysphagia was reported by 3% of patients. Severe dry mouth was reported by 6% of patients. dysphagia and dry mouth were the most frequent adverse events reported as a reason for discontinuation from repeated treatment studies. These adverse events led to discontinuation from further treatments with rimabotulinumtoxinb in some patients even when not reported as severe.
- The following additional adverse events were reported in 2% or greater of patients participating in any of the clinical studies (COSTART terms, by body system):
- Body as a Whole: allergic reaction, fever, headache related to injection, chest pain, chills, hernia, malaise, abscess, cyst, neoplasm, viral infection
- Musculoskeletal: arthritis, joint disorder
- Cardiovascular System: migraine; Respiratory: dyspnea, lung disorder, pneumonia
- Nervous System: anxiety, tremor, hyperesthesia, somnolence, confusion, pain related to CD/torticollis, vertigo, vasodilation
- Digestive System: gastrointestinal disorder, vomiting, glossitis, stomatitis, tooth disorder
- Skin and Appendages: pruritis
- Urogenital System: urinary tract infection, cystitis, vaginal moniliasis
- Special Senses: amblyopia, otitis media, abnormal vision, taste perversion, tinnitus
- Metabolic and Nutritional Disorders: peripheral edema, edema, hypercholesterolemia
- Hemic and Lymphatic System: ecchymosis.
Postmarketing Experience
- The following adverse events have been reported during postmarketing use for approved and unapproved indications: angioedema, urticaria, rash and constipation.
Drug Interactions
- Co-administration of rimabotulinumtoxinb and aminoglycosides or other agents interfering with neuromuscular transmission (e.g., curare-like compounds) should only be performed with caution as the effect of the toxin may be potentiated.
- The effect of administering different botulinum neurotoxin serotypes at the same time or within less than 4 months of each other is unknown. However, neuromuscular paralysis may be potentiated by co-administration or overlapping administration of different botulinum toxin serotypes.
Use in Specific Populations
Pregnancy
- Animal reproduction studies have not been conducted with rimabotulinumtoxinb. It is also not known whether rimabotulinumtoxinb can cause fetal harm when administered to a pregnant woman or can affect reproduction capacity. Rimabotulinumtoxinb should be given to a pregnant woman only if clearly needed.
Pregnancy Category (AUS):
There is no Australian Drug Evaluation Committee (ADEC) guidance on usage of Rimabotulinumtoxinb in women who are pregnant.
Labor and Delivery
There is no FDA guidance on use of Rimabotulinumtoxinb during labor and delivery.
Nursing Mothers
- It is not known whether this drug is excreted in human milk. Because many drugs are excreted in human milk, caution should be exercised when rimabotulinumtoxinb is administered to a nursing woman.
Pediatric Use
- Safety and effectiveness in pediatric patients have not been established.
Geriatic Use
- In the controlled studies summarized in CLINICAL STUDIES, for rimabotulinumtoxinb treated patients, 152 (74.5%) were under the age of 65, and 52 (25.5%) were aged 65 or greater. For these age groups, the most frequent reported adverse events occurred at similar rates in both age groups. Efficacy results did not suggest any large differences between these age groups.
Very few patients aged 75 or greater were enrolled, therefore no conclusions regarding the safety and efficacy of rimabotulinumtoxinb within this age group can be determined.
Gender
There is no FDA guidance on the use of Rimabotulinumtoxinb with respect to specific gender populations.
Race
There is no FDA guidance on the use of Rimabotulinumtoxinb with respect to specific racial populations.
Renal Impairment
There is no FDA guidance on the use of Rimabotulinumtoxinb in patients with renal impairment.
Hepatic Impairment
There is no FDA guidance on the use of Rimabotulinumtoxinb in patients with hepatic impairment.
Females of Reproductive Potential and Males
There is no FDA guidance on the use of Rimabotulinumtoxinb in women of reproductive potentials and males.
Immunocompromised Patients
There is no FDA guidance one the use of Rimabotulinumtoxinb in patients who are immunocompromised.
Administration and Monitoring
Administration
- Intramuscular.
Monitoring
- In the event of overdose, the patient should be medically monitored for symptoms of excessive muscle weakness or muscle paralysis.
- Monitore individuals with peripheral motor neuropathic diseases, amyotrophic lateral sclerosis, or neuromuscular junctional disorders when given botulinum toxin.
IV Compatibility
- There is limited information regarding IV Compatibility.
Overdosage
- Excessive doses of rimabotulinumtoxinb may be expected to produce neuromuscular weakness with a variety of symptoms. Respiratory support may be required where excessive doses cause paralysis of respiratory muscles. In the event of overdose, the patient should be medically monitored for symptoms of excessive muscle weakness or muscle paralysis. Symptomatic treatment may be necessary.
- Symptoms of overdose are likely not to be present immediately following injection. Should accidental injection or oral ingestion occur, the person should be medically supervised for several weeks for signs and symptoms of excessive muscle weakness or muscle paralysis.
- In the event of overdose, antitoxin raised against botulinum toxin is available from the Centers for Disease Control and Prevention (CDC) in Atlanta, GA. However, the antitoxin will not reverse any botulinum toxin-induced effects already apparent by the time of antitoxin administration. In the event of suspected or actual cases of botulinum toxin poisoning, please contact your local or state Health Department to process a request for antitoxin through the CDC.
Pharmacology
There is limited information regarding Rimabotulinumtoxinb Pharmacology in the drug label.
Mechanism of Action
- The seven serologically distinct botulinum neurotoxins, designated A through G, share a common structural organization consisting of one Heavy Chain and one Light Chain polypeptide linked by a single disulfide bond. These toxins inhibit acetylcholine release at the neuromuscular junction via a three stage process: 1) Heavy Chain mediated neurospecific binding of the toxin, 2) internalization of the toxin by receptor-mediated endocytosis, and 3) ATP and pH dependent translocation of the Light Chain to the neuronal cytosol where it acts as a zinc-dependent endoprotease cleaving polypeptides essential for neurotransmitter release. rimabotulinumtoxinb specifically has been demonstrated to cleave synaptic Vesicle Associated Membrane Protein (VAMP, also known as synaptobrevin) which is a component of the protein complex responsible for docking and fusion of the synaptic vesicle to the presynaptic membrane, a necessary step to neurotransmitter release.
Structure
- RimabotulinumtoxinB injection is a sterile liquid formulation of a purified neurotoxin that acts at the neuromuscular junction to produce flaccid paralysis. The neurotoxin is produced by fermentation of the bacterium Clostridium botulinum type B (Bean strain) and exists in noncovalent association with hemagglutinin and nonhemagglutinin proteins as a neurotoxin complex. The neurotoxin complex is recovered from the fermentation process and purified through a series of precipitation and chromatography steps.
- Rimabotulinumtoxinb is provided as a clear and colorless to light-yellow sterile injectable solution in 3.5-mL glass vials. Each single-use vial of formulated rimabotulinumtoxinb contains 5,000 Units of botulinum toxin type B per milliliter in 0.05% human serum albumin, 0.01 M sodium succinate, and 0.1 M sodium chloride at approximately pH 5.6.
- One unit of rimabotulinumtoxinb corresponds to the calculated median lethal intraperitoneal dose (LD50) in mice. The method for performing the assay is specific to Solstice Neurosciences' manufacture of rimabotulinumtoxinb. Due to differences in specific details such as the vehicle, dilution scheme and laboratory protocols for various mouse LD50 assays, units of biological activity of rimabotulinumtoxinb cannot be compared to or converted into units of any other botulinum toxin or any toxin assessed with any other specific assay method. Therefore, differences in species sensitivities to different botulinum neurotoxin serotypes preclude extrapolation of animal dose-activity relationships to human dose estimates. The specific activity of rimabotulinumtoxinb ranges between 70 to 130 Units/ng.
Pharmacodynamics
- There is limited information regarding pharmacodynamics
Pharmacokinetics
- Using currently available analytical technology, it is not possible to detect rimabotulinumtoxinb in the peripheral blood following intramuscular injection at the recommended doses.
Nonclinical Toxicology
- No long-term carcinogenicity studies in animals have been performed.
Clinical Studies
- Two phase 3, randomized, multi-center, double-blind, placebo controlled studies of the treatment of cervical dystonia were conducted. Both studies enrolled only adult patients who had a history of receiving botulinum toxin type A in an open label manner, with a perceived good response and tolerable adverse effects. Study #301 enrolled patients who were perceived as having an acceptable response to type A toxin, while Study #302 enrolled only patients who had secondarily lost responsiveness to type A toxin. Other eligibility criteria common to both studies were that all subjects had moderate or greater severity of cervical dystonia with at least 2 muscles involved, no neck contractures or other causes of decreased neck range of motion, and no history of any other neuromuscular disorder. Subjects in Study #301 were randomized to receive placebo, 5,000 Units or 10,000 Units of rimabotulinumtoxinb, and subjects in Study #302 were randomized to receive placebo or 10,000 Units of rimabotulinumtoxinb. Study agent was administered to subjects in a single treatment session by investigators who selected 2 to 4 muscles per subject from the following: Splenius capitis, Sternocleidomastoid, Levator scapulae, Trapezius, Semispinalis capitis, and Scalene muscles. The total dose was divided between the selected muscles, and from 1 to 5 injections were made per muscle. There were 109 subjects enrolled into Study #301, and 77 into Study #302. Patient evaluations continued for 16 weeks post injection.
- The primary efficacy outcome variable for both studies was the Toronto Western Spasmodic Torticollis Rating Scale (TWSTRS)-Total Score (scale range of possible scores is 0–87) at Week 4. TWSTRS is comprised of three sub-scales which examine 1) Severity—the severity of the patient's abnormal head position; 2) Pain—the severity and duration of pain due to the dystonia; and 3) Disability— the effects of the abnormal head position and pain on a patient's activities. The secondary endpoints were the Patient Global and Physician Global Assessments of change at Week 4. Both Global Assessments used a 100-point visual-analog scale (VAS). The Patient Global Assessment allows patients to indicate how they feel at the time of their evaluation compared to the pre-injection baseline. Likewise, the Physician Global Assessment indicates the physician's assessment of a patient's change from baseline to Week 4. Scores of 50 indicate no change, 0 much worse, and 100 much better. Results of comparisons of the primary and secondary efficacy variables are summarized in Table 1.

- There were no statistically significant differences in results between the 5,000 Units and 10,000 Units doses in Study #301. Exploratory analyses of these two studies suggested that the majority of patients who showed a beneficial response by Week 4 had returned to their baseline status between Weeks 12 to 16 post injection. Although there was a rimabotulinumtoxinb associated decrease in pain, there remained many patients who experienced an increase in dystonia-related neck pain irrespective of treatment group. TWSTRS Total Score at Week 4 and Patient Global Assessment among subgroups by gender or age showed consistent treatment-associated effects across these subgroups. There were too few non-Caucasian patients enrolled to draw any conclusions regarding relative efficacy in racial subsets.
- Rimabotulinumtoxinb was studied in two phase 2 dose ranging studies, Studies #08 and #09, which preceded the phase 3 studies. Studies #08 and #09 had a study design similar to the phase 3 studies, including eligibility criteria. Study #08 enrolled 85 subjects randomized between doses of placebo, 400 Units, 1,200 Units, or 2,400 Units (21 or 22 subjects per group). Study #09 enrolled 122 subjects and randomized between doses of placebo, 2,500 Units, 5,000 Units, and 10,000 Units (30 or 31 subjects per group). These studies demonstrated efficacy on the TWSTRS-Total, baseline to Week 4, at doses of 2,400 Units, 2,500 Units, 5,000 Units, and 10,000 Units. Study #08 showed mean improvement from baseline on the Week 4 TWSTRS for placebo and 2,400 Units of 2.0 and 8.5 points respectively (from baselines of 42.0 and 42.4 points). Study #09 showed mean improvement from baseline to Week 4 for placebo, 2,500 Units, 5,000 Units, and 10,000 Units of 3.3, 11.6, 12.5, and 16.4 points, respectively (from baselines of 45.5, 45.6, 45.2, and 47.5 points). Study #08 also indicated there is less response for doses below 2,400 Units.
- Study #352 was an open label, intrapatient dose-escalation study of 3 treatment sessions where each patient with cervical dystonia sequentially received 10,000 Units, 12,500 Units, and 15,000 Units, at periods of 12 to 16 weeks between treatment sessions irrespective of their response to their previous dose. This study enrolled 145 patients, of whom 125 received all three treatments. Although this was an open label design where investigators and patients knew the dose at each treatment session, there were similar mean improvements on the TWSTRS-Total, from baseline to Week 4, for all three doses.
- In the rimabotulinumtoxinb injected patients (n=112) of the phase 3 studies, 19% had 2 muscles injected, 48% had 3 muscles injected, and 33% had 4 muscles injected. Table 2 indicates the frequency of use for each of the permitted muscles, and the fraction of the total dose of the treatment injected into each muscle, for those patients in whom the muscle was injected.

How Supplied
- MYOBLOC is provided as a clear and colorless to light-yellow sterile injectable solution in single-use 3.5-mL glass vials. Each single-use vial of formulated MYOBLOC contains 5,000 Units1 of botulinum toxin type B per milliliter in 0.05% human serum albumin, 0.01 M sodium succinate, 0.1 M sodium chloride at approximately pH 5.6.
- MYOBLOC is available in the following three presentations.
Storage
- Store under refrigeration at 2°- 8°C (36°- 46°F).
- DO NOT FREEZE. DO NOT SHAKE.
- Protect from light. No U.S. Standard of Potency.
- Ready to use; no reconstitution required. The recommended storage condition for MYOBLOC is refrigeration at 2°-8°C.
Images
Drug Images
{{#ask: Page Name::Rimabotulinumtoxinb |?Pill Name |?Drug Name |?Pill Ingred |?Pill Imprint |?Pill Dosage |?Pill Color |?Pill Shape |?Pill Size (mm) |?Pill Scoring |?NDC |?Drug Author |format=template |template=DrugPageImages |mainlabel=- |sort=Pill Name }}
Package and Label Display Panel




{{#ask: Label Page::Rimabotulinumtoxinb |?Label Name |format=template |template=DrugLabelImages |mainlabel=- |sort=Label Page }}
Patient Counseling Information
- The physician should provide a copy of the FDA-Approved Patient Medication Guide and review the contents with the patient. Patients should be advised to inform their doctor or pharmacist if they develop any unusual symptoms (including difficulty with swallowing, speaking or breathing), or if any existing symptom worsens.
- Patients should be counseled that if loss of strength, muscle weakness, or impaired vision occur, they should avoid driving a car or engaging in other potentially hazardous activities.
Precautions with Alcohol
- Alcohol-Rimabotulinumtoxinb interaction has not been established. Talk to your doctor about the effects of taking alcohol with this medication.
Brand Names
- MYOBLOC ®[1]
Look-Alike Drug Names
- There is limited information regarding Look-Alike Drug Names.
Drug Shortage Status
Price
References
The contents of this FDA label are provided by the National Library of Medicine.