Upper gastrointestinal bleeding initial resuscitation
|
Upper gastrointestinal bleeding Microchapters |
|
Differentiating Upper Gastrointestinal Bleeding from other Diseases |
|---|
|
Diagnosis |
|
Treatment |
|
Management |
|
Surgery |
|
Case Studies |
|
Upper gastrointestinal bleeding initial resuscitation On the Web |
|
American Roentgen Ray Society Images of Upper gastrointestinal bleeding initial resuscitation |
|
FDA on Upper gastrointestinal bleeding initial resuscitation |
|
CDC on Upper gastrointestinal bleeding initial resuscitation |
|
Upper gastrointestinal bleeding initial resuscitation in the news |
|
Blogs on Upper gastrointestinal bleeding initial resuscitation |
|
Directions to Hospitals Treating Upper gastrointestinal bleeding |
|
Risk calculators and risk factors for Upper gastrointestinal bleeding initial resuscitation |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1] ; Associate Editor(s)-in-Chief: Aditya Ganti M.B.B.S. [2]
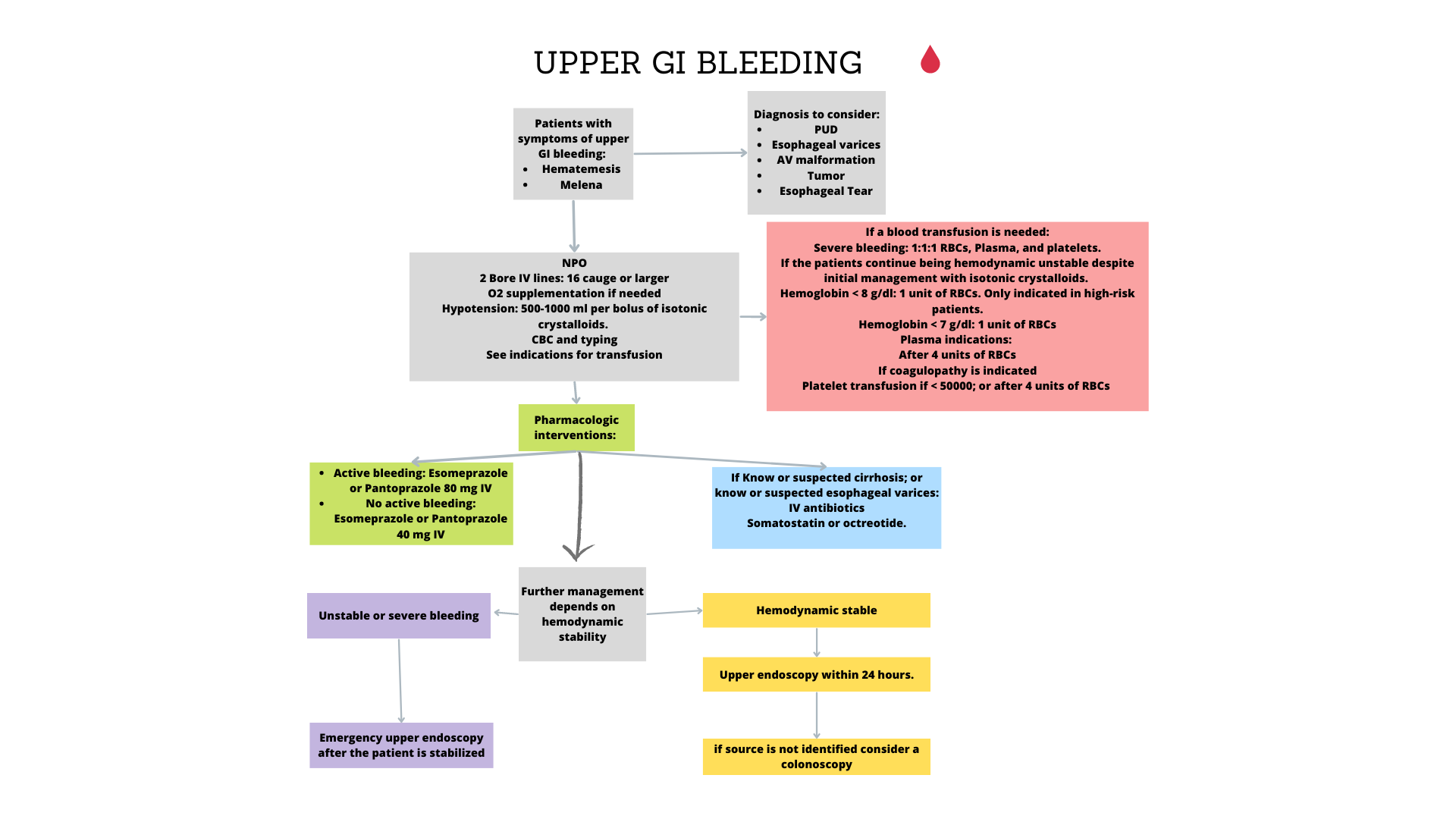
Overview
In patients with acute upper GI bleeding who are unstable rapid assessment and resuscitation should be initiated even before diagnostic evaluation. The initial steps in the management of a patient with UGIB is to assess the severity of bleeding, and then institute fluid and blood resuscitation as needed. Once hemodynamic stability is achieved, a proper clinical history, physical examination, and initial laboratory findings are crucial not only in determining the likely sources of bleeding but also in directing the appropriate intervention. Equilibration between the intravascular and extravascular volumes cannot be achieved until 24 to 72 hours after bleeding has occurred. Nasogastric lavage should be performed if the presence or source of bleeding is unknown. Upper gastrointestinal endoscopy is the primary diagnostic tool, performed for both diagnosis and treatment of active bleeding. The American Society for Gastrointestinal Endoscopy guidelines recommends upper endoscopy within 24 hours of presentation in all patients with UGIB. Angiography and tagged erythrocyte scan are rarely needed but may be used to diagnose active UGIB, particularly in patients where EGD is contraindicated. Also, upper gastrointestinal tract radiographic studies using barium are generally not advised, as they may obscure visualization during EGD.
Initial Management
Management of upper GI bleeding includes:[1][2][3]
Initial resuscitation
- The initial steps in the management of a patient with UGIB is to assess the severity of bleeding, and then institute fluid and blood resuscitation as needed.[4][5][6]
- Any patient with hemodynamic instability or who is actively bleeding should be admitted to the ICU for monitoring and resuscitation
- The patient’s hemodynamic status is of great importance in determining the degree of severity and triage status.
| Criteria for Admission of patient |
|---|
Supportive Therapy
- Supportive care includes administration of supplemental oxygen, IV fluid administration, and monitoring of urine output.[6]
- Two large caliber (16-gauge) peripheral catheters or a central venous line should be inserted in patients who are hemodynamically unstable.[6]
- The rate of fluid resuscitation is proportional to the severity of bleeding with the goal of restoring and maintaining the patient’s blood pressure.[6]
- Infusion of 500 mL of normal saline or lactated Ringer's solution over 30 minutes is preferred treatment for patients with active bleeding before blood type matching and blood transfusion.[6]
- Intensive monitoring with a pulmonary artery catheter is recommended to monitor the response of initial resuscitation efforts and any falls in blood pressure:[6]
| Correlation between physical signs and the severity of upper gastrointestinal bleeding | |||
|---|---|---|---|
| Physical signs | Bleeding severity | ||
| Mild | Moderate | Severe | |
| Blood loss | <1L | 1-2L | >2L |
| Systolic blood pressure | <120 | 100-119 | <99 |
| Orthostasis | - | - | + |
| Tachycardia | <100 | 101-120 | >140 |
| Skin | Warm, well perfused | Diaphoretic | Cool–cold, clammy |
| Urine output(ml/hour) | >25 | 10-25 | Negligible |
| Respiratory rate | 14-20 | 20-30 | >35 |
| Sensorium | Alert | Anxious | Confused/Drowsy |
Blood transfusion
| Indications for transfusion
Based on the patient’s age and presence of comorbid conditions. | |
|---|---|
| AGE | Target Hematocrit |
| Elderly patient ( >45) | 30% |
| Younger patient (<45) | 25% |
| patients with portal hypertension | 28% |
- Fresh frozen plasma, platelets, or both should be given to patients with coagulopathy who are actively bleeding and to those who have received more than 10 units of packed erythrocytes:
| WORKUP AND INITIAL TREATMENT Initial Resuscitation | |
|---|---|
| Initial Evaluation |
|
| Supportive Therapy |
|
| Blood transfusion |
|
National Institute for Health and Care Excellence (NICE) guidline
The National Institute for Health and Care Excellence (NICE) guidline on blood product management in upper GI bleeding:[9]
- Platelets should only be given if the patient is actively bleeding or hemodynamically unstable and has a platelet count of <50×109/L.
- Fresh frozen plasma should be given if the fibrinogen level is <1 g/L or the prothrombin time (PT) or activated partial thromboplastin time is >1.5 times normal.
- Prothrombin complex should be provided to those on warfarin and actively bleeding.
- Recombinant factor VIIa should only be used when all of the above measures have failed.
| Acute GI bleeding | |||||||||||||||||||||||||||||||||||||||||||||||
| Initial evaluation and resuscitation | |||||||||||||||||||||||||||||||||||||||||||||||
| Uppe GI endoscopy | |||||||||||||||||||||||||||||||||||||||||||||||
| Source found | Undiagnostic | ||||||||||||||||||||||||||||||||||||||||||||||
| Specific Treatment | |||||||||||||||||||||||||||||||||||||||||||||||
| Unstable | Stable | ||||||||||||||||||||||||||||||||||||||||||||||
| Urgent CT | Repeat Endoscopy/Angiograpghy | ||||||||||||||||||||||||||||||||||||||||||||||
| No source identified | |||||||||||||||||||||||||||||||||||||||||||||||
| Angioembolization | Endoscopic intervention | TIPS | Surgery | ||||||||||||||||||||||||||||||||||||||||||||
| Surgery (Laprotomy) | |||||||||||||||||||||||||||||||||||||||||||||||
| Sclerotherapy | Banding | Injection | Thermocoagulation | Clips | |||||||||||||||||||||||||||||||||||||||||||
References
- ↑ Beales I (2017). "Recent advances in the management of peptic ulcer bleeding". F1000Res. 6: 1763. doi:10.12688/f1000research.11286.1. PMC 5621101. PMID 29043071.
- ↑ Bethea ED, Travis AC, Saltzman JR (2014). "Initial assessment and management of patients with nonvariceal upper gastrointestinal bleeding". J. Clin. Gastroenterol. 48 (10): 823–9. doi:10.1097/MCG.0000000000000194. PMID 25090451.
- ↑ Klein A, Gralnek IM (2015). "Acute, nonvariceal upper gastrointestinal bleeding". Curr Opin Crit Care. 21 (2): 154–62. doi:10.1097/MCC.0000000000000185. PMID 25692808.
- ↑ Wassef W (2004). "Upper gastrointestinal bleeding". Curr. Opin. Gastroenterol. 20 (6): 538–45. PMID 15703679.
- ↑ Kovacs TO (2008). "Management of upper gastrointestinal bleeding". Curr Gastroenterol Rep. 10 (6): 535–42. PMID 19006607.
- ↑ 6.0 6.1 6.2 6.3 6.4 6.5 Gralnek IM, Dumonceau JM, Kuipers EJ, Lanas A, Sanders DS, Kurien M, Rotondano G, Hucl T, Dinis-Ribeiro M, Marmo R, Racz I, Arezzo A, Hoffmann RT, Lesur G, de Franchis R, Aabakken L, Veitch A, Radaelli F, Salgueiro P, Cardoso R, Maia L, Zullo A, Cipolletta L, Hassan C (2015). "Diagnosis and management of nonvariceal upper gastrointestinal hemorrhage: European Society of Gastrointestinal Endoscopy (ESGE) Guideline". Endoscopy. 47 (10): a1–46. doi:10.1055/s-0034-1393172. PMID 26417980.
- ↑ Al-Jaghbeer M, Yende S (2013). "Blood transfusion for upper gastrointestinal bleeding: is less more again?". Crit Care. 17 (5): 325. doi:10.1186/cc13020. PMC 4056793. PMID 24063362.
- ↑ Villanueva C, Colomo A, Bosch A, Concepción M, Hernandez-Gea V, Aracil C, Graupera I, Poca M, Alvarez-Urturi C, Gordillo J, Guarner-Argente C, Santaló M, Muñiz E, Guarner C (2013). "Transfusion strategies for acute upper gastrointestinal bleeding". N. Engl. J. Med. 368 (1): 11–21. doi:10.1056/NEJMoa1211801. PMID 23281973.
- ↑ "Acute upper gastrointestinal bleeding in over 16s: management | Guidance and guidelines | NICE".
- ↑ Laine L, Barkun AN, Saltzman JR, Martel M, Leontiadis GI (2021) ACG Clinical Guideline: Upper Gastrointestinal and Ulcer Bleeding. Am J Gastroenterol 116 (5):899-917. DOI:10.14309/ajg.0000000000001245 PMID: 33929377