Sandbox:Lina Alatta
Gastroenterology
Celiac Disease
Overview
Celiac disease is an immune-mediated sensitivity to gluten in genetically suspected individuals that mainly affects the small intestinal mucosa. [1]
Historical Perspectives
Celiac disease was first discovered by Dutch pediatricians in late 1940, as a disease caused by gluten. After that, main changes were done in realizing the disease pathogenesis, diagnosis and treatment.[2]
Classification
There is no classification system established for Celiac disease.
Pathophysiology
The exact pathogenesis of celiac disease is not fully understood. It is thought that celiac disease is produced by combination of genetics, environmental and immunological triggers.[3]
Genetics Factors
Celiac disease has a known genetic factor as evidenced by its increased familial recurrence (~ 10–15%) and the common concordance of the disease in monozygotic twins (75–80%). The role of HLA class II heterodimers, chiefly DQ2 and DQ8, in the genetics of celiac disease. HLA-DQ2 homozygosis has an increased risk (25–30%) of acquiring early-onset CD in infants with a first-degree family member affected by the disease. Since HLA-DQ2/HLA-DQ8 is more common (25–35%), and only 3% of these HLA-compatible persons will be diagnosed with celiac disease, it is not surprising that genome-wide association studies have discovered greater than 100 non-HLA-related genes linked to celiac disease. The significant of these additional genes in proving genetic factor for celiac disease is rather limited, but they may lead to the discovery of main pathways strongly involved in disease pathogenesis.[4]
Environmental Factors
Not all genetic suspected individuals will be symptomatic, another non-genetic environmental factors may contribute in developing the disease. For example, amylase trypsin inhibitors (ATIs) which is found in gluten-containing grains, because this can initiate a Toll-like receptor 4-dependent innate immune response in the small intestine. Furthermore, viral infections (by rotaviruses, adenovirus, enteroviruses and hepatitis C virus) are linked to greater incidence of celiac disease. Moreover, a high number of celiac-associated genetic loci has transcription factor binding elements for gene products of the Epstein-Barr virus, that's show the virus can regulate celiac disease pathways. some experimental studies which were done on mice's having HLA-DQ8 on their genes proved that reovirus infection can affect their tolerance to gluten along with other antigens.[5]
Immunological Factors
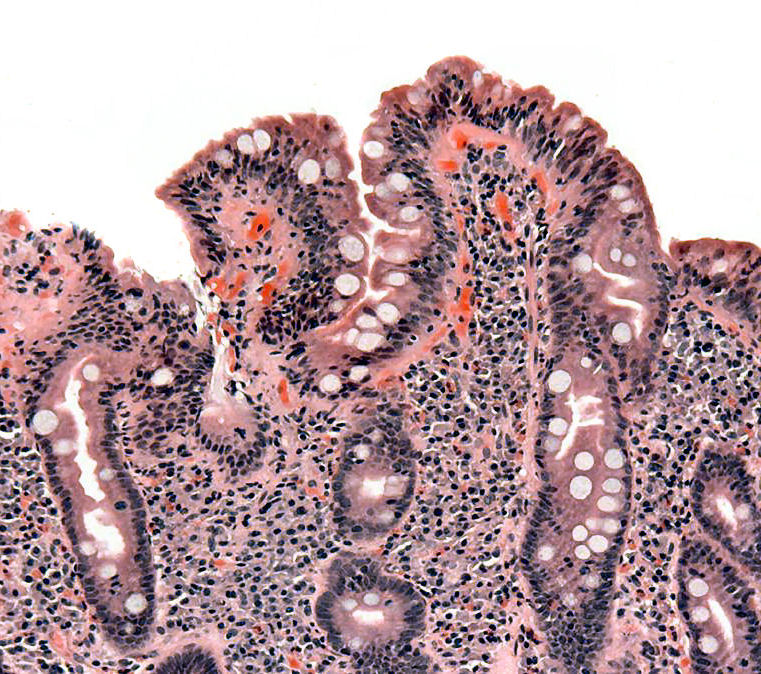
The immune response in gluten-sensitive enteropathy mainly include plasma cells that's produce IgG and IgA, there's minimum or no contribution of IgE . Recent studies demonstrate that ingested a part of gluten called α-gliadin and related peptides bind with tissue transglutaminase (a ubiquitous intracellular enzyme) in enterocytes. The α-gliadin is contain high level of gultamine; transglutaminaseas foreign by host cell–mediated immunity. Plasma cells produce IgA and IgG that attack number of antigens, including transglutaminase, endomysium, gliadin, and reticulin. Locally elaborated lymphokines attract inflammatory cells. This strong local inflammatory reaction produces the villous flattening characteristic of gluten-sensitive enteropathy.[6]
Causes
- Genetics causes
- Consumption of :
- Wheat
- Gluten containing products.
Signs and Symptoms
| system | signs and symptoms |
|---|---|
| GIT | Malabsorption |
| Dermatological | dermatitis herpetiforms |
References
- ↑ Freeman HJ (2015). "Celiac disease: a disorder emerging from antiquity, its evolving classification and risk, and potential new treatment paradigms". Gut Liver. 9 (1): 28–37. doi:10.5009/gnl14288. PMC 4282854. PMID 25547088.
- ↑ Murray JA, Frey MR, Oliva-Hemker M (2018). "Celiac Disease". Gastroenterology. 154 (8): 2005–2008. doi:10.1053/j.gastro.2017.12.026. PMC 6203336. PMID 29550590.
- ↑ Kupfer SS, Jabri B (2012). "Pathophysiology of celiac disease". Gastrointest Endosc Clin N Am. 22 (4): 639–60. doi:10.1016/j.giec.2012.07.003. PMC 3872820. PMID 23083984.
- ↑ Caio G, Volta U, Sapone A, Leffler DA, De Giorgio R, Catassi C; et al. (2019). "Celiac disease: a comprehensive current review". BMC Med. 17 (1): 142. doi:10.1186/s12916-019-1380-z. PMC 6647104 Check
|pmc=value (help). PMID 31331324. - ↑ Moerkens R, Mooiweer J, Withoff S, Wijmenga C (2019). "Celiac disease-on-chip: Modeling a multifactorial disease in vitro". United European Gastroenterol J. 7 (4): 467–476. doi:10.1177/2050640619836057. PMC 6488795. PMID 31065364.
- ↑ Molberg Ø, Solheim Flaete N, Jensen T, Lundin KE, Arentz-Hansen H, Anderson OD; et al. (2003). "Intestinal T-cell responses to high-molecular-weight glutenins in celiac disease". Gastroenterology. 125 (2): 337–44. doi:10.1016/s0016-5085(03)00890-4. PMID 12891534.