Pulseless electrical activity electrocardiogram
| Resident Survival Guide |
|
Pulseless electrical activity Microchapters |
|
Differentiating Pulseless Electrical Activity from other Diseases |
|---|
|
Diagnosis |
|
Treatment |
|
Case Studies |
|
Pulseless electrical activity electrocardiogram On the Web |
|
American Roentgen Ray Society Images of Pulseless electrical activity electrocardiogram |
|
Directions to Hospitals Treating Pulseless electrical activity |
|
Risk calculators and risk factors for Pulseless electrical activity electrocardiogram |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]
Overview
The appearance of the electrocardiogram in the setting of PEA varies, but several common patterns exist. There may be a normal sinus rhythm or sinus tachycardia, with discernible P waves and QRS complexes. Sometimes there is a bradycardia, with or without P waves, and often there is a wide QRS complex.[1] The presence of a QRS interval > 0.20 seconds is associated with a poorer prognosis. The EKG should be carefully evaluated for signs of Hyperkalemia, ST segment elevation MI, hypothermia, QRS interval prolongation suggests tricyclic antidepressant overdose
Electrocardiogram
The appearance of the electrocardiogram in the setting of PEA varies, but several common patterns exist. There may be a normal sinus rhythm or sinus tachycardia, with discernible P waves and QRS complexes. Sometimes there is a bradycardia, with or without P waves, and often there is a wide QRS complex. The presence of a QRS interval > 0.20 seconds is associated with a poorer prognosis. The EKG should be carefully evaluated for signs of:[2][3][1][4][5]
- Hyperkalemia (peaked T waves, complete heart block, a ventricular escape rhythm)
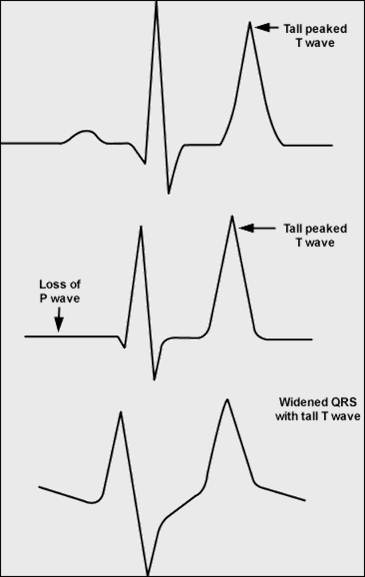
Shown below is an EKG demonstrating peaked T waves, loss of P wave and wide QRS complex depicting hyperkalemia [6].
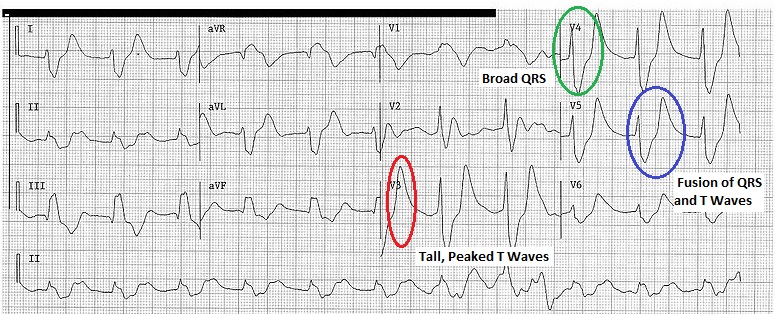
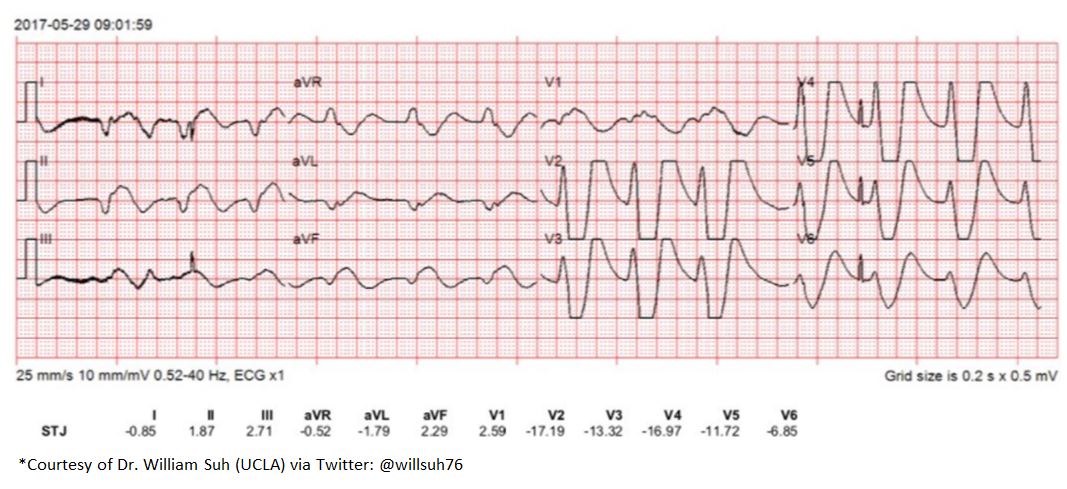
Shown below is an EKG demonstrating wide QRS complexes, tall peaked T waves an fusion of the QRS complex and the T wave.
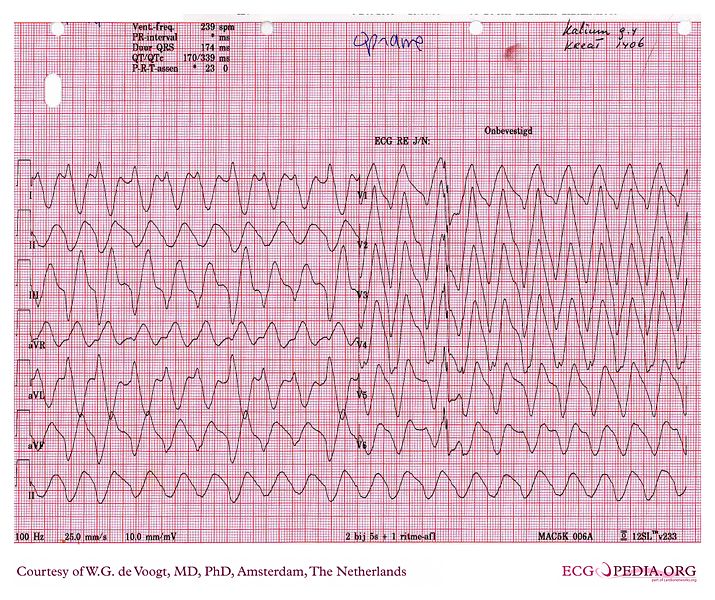
Shown below is an EKG demonstrating sine wave pattern depicting severe hyperkalemia.[7]
- Osborne waves suggest hypothermia
- Osborn waves are positive deflections occurring at the junction between the QRS complex and the ST segment, where the S point, also known as the J joint, has a myocardial infarction-like elevation.Osborn waves are more prominent in the left precordial leads. They increases in size with decreasing temperature. They are caused by a current of injury, delayed ventricular depolarization, or early repolarization.Osborn waves may first appear on the ECG for temperatures less than 91.4 degrees Fahrenheit (33 degrees Celsius), and consistently appear when when the temperature falls below 25 degrees Centigrade.There is variability in the morphology of Osborn waves as all J wave deflections do not look alike. Some Osborn waves are merely elevations of ST segments in leads V1 and V2, whereas others are of the "spike-and-dome" variety. Given the variability in morphology, a variety of mechanisms may be responsible for the size and shape of J wave deflections.
Shown below is an example of the "spike and dome" variant of the Osborn wave:

Shown below is an Osborn wave in an 81-year-old male with a core temperature 89.5 degrees F (31.94 C):

- ST segment elevation MI should be ruled out
- QRS interval prolongation suggests tricyclic antidepressant overdose
References
- ↑ 1.0 1.1 Foster B, Twelve Lead Electrocardiography, 2nd edition, 2007
- ↑ Mehta C, Brady W (2012). "Pulseless electrical activity in cardiac arrest: electrocardiographic presentations and management considerations based on the electrocardiogram". Am J Emerg Med. 30 (1): 236–9. doi:10.1016/j.ajem.2010.08.017. PMID 20970286.
- ↑ Luong DH, Cheung PY, O'Reilly M, Lee TF, Schmolzer GM (2018). "Electrocardiography vs. Auscultation to Assess Heart Rate During Cardiac Arrest With Pulseless Electrical Activity in Newborn Infants". Front Pediatr. 6: 366. doi:10.3389/fped.2018.00366. PMC 6277703. PMID 30538976.
- ↑ Varga C, Kálmán Z, Szakáll A, Drubits K, Koch M, Bánhegyi R, Oláh T, Pozsgai É, Fülöp N, Betlehem J (May 2019). "ECG alterations suggestive of hyperkalemia in normokalemic versus hyperkalemic patients". BMC Emerg Med. 19 (1): 33. doi:10.1186/s12873-019-0247-0. PMC 6814982 Check
|pmc=value (help). PMID 31151388. - ↑ Atkinson PR, Keyes AW, O'Donnell K, Beckett N, Banerjee A, Fraser J, Lewis D (November 2018). "Do Electrocardiogram Rhythm Findings Predict Cardiac Activity During a Cardiac Arrest? A Study from the Sonography in Cardiac Arrest and Hypotension in the Emergency Department (SHoC-ED) Investigators". Cureus. 10 (11): e3624. doi:10.7759/cureus.3624. PMC 6347444. PMID 30697500.
- ↑ Bashour T, Hsu I, Gorfinkel HJ, Wickramesekaran R, Rios JC (1975). "Atrioventricular and intraventricular conduction in hyperkalemia". Am J Cardiol. 35 (2): 199–203. PMID 1119378.
- ↑ Patton KK, Ellinor PT, Ezekowitz M, Kowey P, Lubitz SA, Perez M; et al. (2016). "Electrocardiographic Early Repolarization: A Scientific Statement From the American Heart Association". Circulation. 133 (15): 1520–9. doi:10.1161/CIR.0000000000000388. PMID 27067089.