Plummer-Vinson syndrome laboratory findings
|
Plummer-Vinson syndrome Microchapters |
|
Diagnosis |
|---|
|
Treatment |
|
Case Studies |
|
Plummer-Vinson syndrome laboratory findings On the Web |
|
American Roentgen Ray Society Images of Plummer-Vinson syndrome laboratory findings |
|
Risk calculators and risk factors for Plummer-Vinson syndrome laboratory findings |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1];Associate Editor(s)-in-Chief: Akshun Kalia M.B.B.S.[2]
Overview
Laboratory findings consistent with the diagnosis of Plummer-Vinson syndrome include presence of iron deficiency anemia. Patients suspected of Plummer-Vinson syndrome should be tested with complete blood count (CBC), iron studies, peripheral smear, stool test for occult blood, blood lead levels and bone marrow biopsy for stainable iron.
Laboratory Findings
Laboratory findings consistent with the diagnosis of Plummer-Vinson syndrome include presence of iron deficiency anemia:[1][2][3][4][5][6][7][8]
- Complete blood count (CBC) should be done in patients of Plummer-Vinson syndrome and will have the following findings:
- Low mean corpuscular volume (MCV <80 fl)
- Low mean corpuscular hemoglobin concentration (MCHC)
- Elevated platelet count (platelets > 450,000/µL)
- Normal or elevated white blood cell count
- Iron studies should be done in patients with pallor, dysphagia or esophageal webs to confirm the diagnosis of Plummer-Vinson syndrome. The tests usually done for iron deficiency anemia are:
- Serum iron- Decreased in iron deficiency
- Transferrin- Elevated in iron deficiency
- Total iron binding capacity (TIBC)- Elevated in iron deficiency
- Transferrin saturation- derived by dividing the serum iron by the TIBC. Decreased in iron deficiency.
- Ferritin- Indicator of body iron stores and is low in iron deficiency. However, ferritin also acts as an acute phase reactant and can be unreliable in inflammatory illness.
| Change | Parameter |
|---|---|
| Decrease | Hemoglobin, Ferritin, MCV |
| Increase | TIBC, Transferrin, RDW |
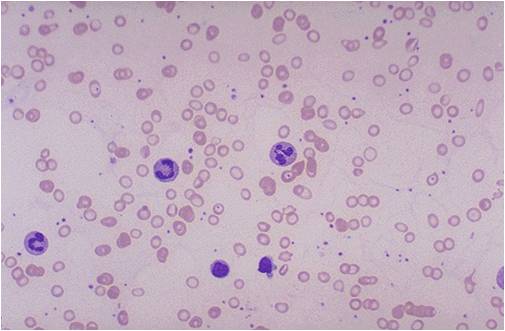
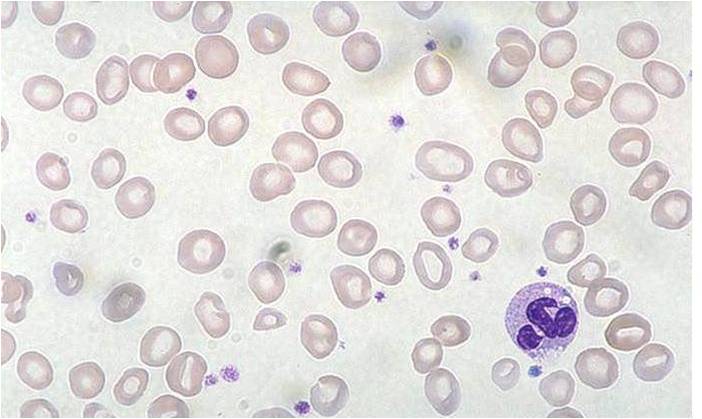
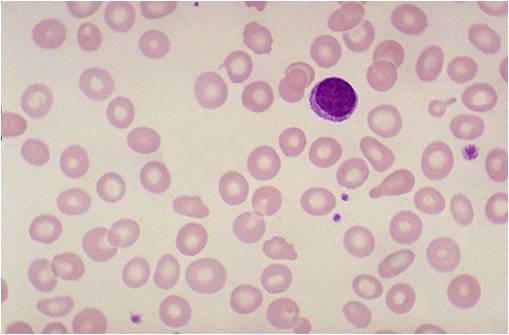
- Peripheral smear:
- RBCs are microcytic and hypochromic
- Increased number of platelets
- Target cells (can be seen in any case of anemia)
(Images shown below are courtesy of Melih Aktan MD, Istanbul Medical Faculty - Turkey)
-
Iron deficiency anemia
-
Iron deficiency anemia
-
Iron deficiency anemia
- Other test includes:
- Stool testing (FOBT): It should be done in all men and postmenopausal women who present with iron deficiency anemia to rule out colonic polyps and malignancy.
- Bone marrow aspiration for stainable iron: This the most accurate test to determine iron deficiency. However, it is not routinely done, since other blood and iron studies are a reliable source to determine the presence of iron deficiency anemia.
- Blood lead levels
References
- ↑ Guyatt G, Patterson C, Ali M, Singer J, Levine M, Turpie I, Meyer R (1990). "Diagnosis of iron-deficiency anemia in the elderly". Am J Med. 88 (3): 205–9. PMID 2178409.
- ↑ Hempel EV, Bollard ER (2016). "The Evidence-Based Evaluation of Iron Deficiency Anemia". Med. Clin. North Am. 100 (5): 1065–75. doi:10.1016/j.mcna.2016.04.015. PMID 27542426.
- ↑ Parkin PC, Maguire JL (2013). "Iron deficiency in early childhood". CMAJ. 185 (14): 1237–8. doi:10.1503/cmaj.130150. PMC 3787170. PMID 23922344.
- ↑ Mazza J, Barr RM, McDonald JW, Valberg LS (1978). "Usefulness of the serum ferritin concentration in the detection of iron deficiency in a general hospital". Can Med Assoc J. 119 (8): 884–6. PMC 1819106. PMID 737638.
- ↑ Thomason RW, Almiski MS (2009). "Evidence that stainable bone marrow iron following parenteral iron therapy does not correlate with serum iron studies and may not represent readily available storage iron". Am. J. Clin. Pathol. 131 (4): 580–5. doi:10.1309/AJCPBAY9KRZF8NUC. PMID 19289594.
- ↑ Kis AM, Carnes M (1998). "Detecting iron deficiency in anemic patients with concomitant medical problems". J Gen Intern Med. 13 (7): 455–61. PMC 1496985. PMID 9686711.
- ↑ Allali S, Brousse V, Sacri AS, Chalumeau M, de Montalembert M (2017). "Anemia in children: prevalence, causes, diagnostic work-up, and long-term consequences". Expert Rev Hematol: 1–6. doi:10.1080/17474086.2017.1354696. PMID 29023171.
- ↑ Liberti ME, Garofalo C, Sagliocca A, Borrelli S, Conte G, De Nicola L, Minutolo R (2017). "[Iron deficiency in ND-CKD: from diagnosis to treatment]". G Ital Nefrol (in Italian). 34 (5): 50–61. PMID 28963827.