Parasellar and suprasellar disorders
| Parasellar and suprasellar disorders |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]
Cavernous Sinus and Parasellar Pathology
Meningioma
Meningiomas account for 15% of all intracranial tumors and are the most common extra-axial tumor. They originate from the dura or arachnoid and occur in middle-aged adults. Women are affected twice as often as men. Meningiomas are well-differentiated, benign, and encapsulated lesions that indent the brain as they enlarge. Parasellar meningiomas commonly involve the cavernous sinus and produce an ophthalmoplegia. Meningiomas can induce an osteoblastic reaction in the adjacent bone, resulting in a characteristic focal hyperostosis. They are also hypervascular, receiving their blood supply predominantly from dural vessels.
Most meningiomas are isointense to brain on T1- and T2-weighted images. A heterogeneous internal texture is found in all but the smallest meningiomas. The mottled pattern is likely due to a combination of flow void from vascularity, focal calcification, small cystic foci, and entrapped CSF spaces. Hemorrhage is not a common feature. An interface between the brain and lesion is often present, representing a CSF cleft, a vascular rim, or a dural margin. MR has special advantages over CT in assessing cavernous sinus involvement and arterial encasement. Meningiomas show intense enhancement with gadolinium and are sharply circumscribed. They have a characteristic broad base of attachment against a dural surface. Contrast scans are especially helpful for imaging the en plaque meningiomas that occur at the skull base.
Nerve Sheath Tumors
Schwannomas in the parasellar region arise from the trigeminal nerve and rarely from the 3rd, 4th, and 6th cranial nerves. The cisternal, cavernous, or extracranial components of the nerves can be involved. They are well-encapsulated, benign tumors, and their more or less globular shape distinguishes them from the broad-based meningiomas. Schwannomas are isointense on T1 and mildly hyperintense on T2-weighted images. Cystic components may be present, and occasional hemorrhage and calcification can further contribute to a heterogeneous appearance. The solid portions of theses tumors enhance brightly with intravenous contrast. Endnote
Skull Base Tumors
Primary, secondary, and metastatic tumors of the skull base can involve the parasellar region. The primary tumors include chordoma, chondroma, chondrosarcoma, and plasmacytoma. Secondary tumors are most often carcinomas from the nasopharynx and paranasal sinuses. The common metastases are from lung, breast, and prostatic carcinoma, but other tumors can also metastasize to the skull.
Chordoma is a rare neoplasm, but it is the most common primary of the clivus. They arise from notochordal remnants in the clivus, meninges along the prepontine cistern, sphenoid or nasopharynx. The most common site is near the spheno-occipital synchondrosis. Chordomas are slow-growing and erode bone by direct extension. The soft tissue mass readily extends into the sella, perisellar, prepontine cistern, sphenoid sinus and middle fossa. Cartilaginous foci, bone fragments and calcifications are interspersed within the tumor matrix. Chondroma is a benign tumor that arises from cartilage cell rests at the skull base.
Chondrosarcoma is the malignant counterpart that often originates from a preexisting benign lesion. Calcification is common in both tumors. Plasmacytoma is another rare tumor of the skull base that is derived from plasma cells. With time, many evolve to multiple myeloma.
Chordomas and chondrosarcomas can be difficult to identify on T1-weighted axial images alone due to low contrast with the adjacent cortical bone and CSF, but alteration of the normal high signal clival fat is a sensitive indicator of disease. Plasmacytoma also has no distinctive MR features to allow for a definitive diagnosis. Enhancement with gadolinium is helpful to assess the intracranial components of these tumors.
Vascular Lesions
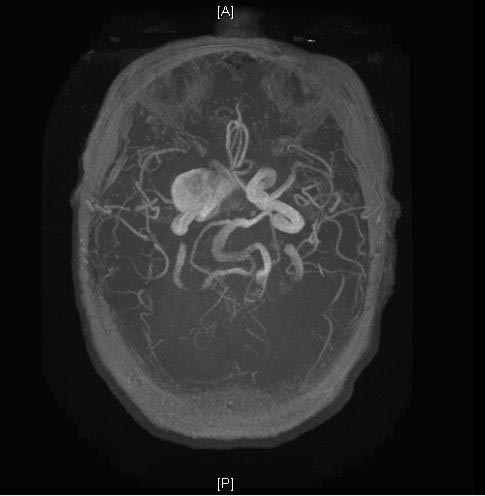
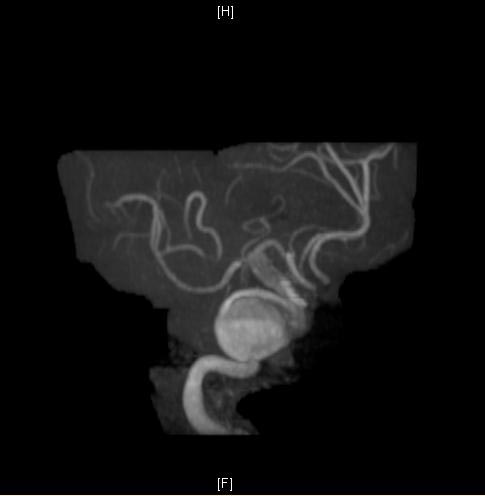
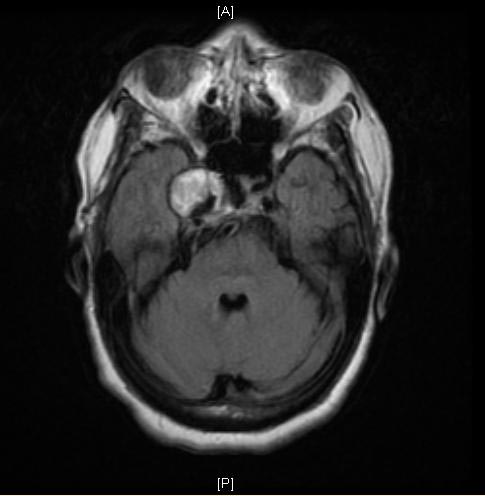
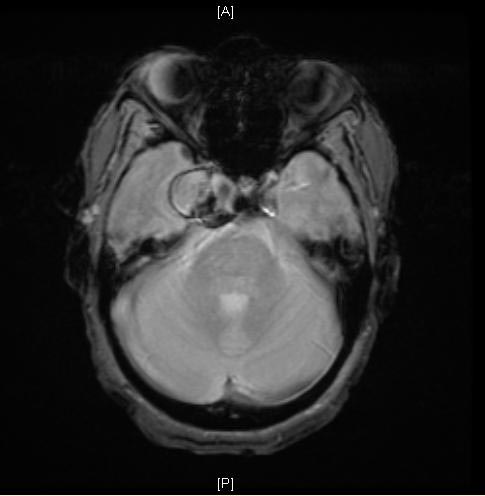
Aneurysm
Aneurysms in the perisellar area arise from the circle of Willis or the intracavernous carotid arteries. A distinctly heterogeneous internal texture on MR images is due to flow effects and thrombus formation. Low signal intensity is caused by high flow and chronic hemorrhage; high signal may represent slow flow or subacute hemorrhage. Flow within the patent lumen may also cause a band of artifact in the phase-encoding direction on spin-echo images. Pneumatization of the anterior clinoid or calcification can simulate the flow void of an aneurysm. MR angiography is helpful to confirm the diagnosis of aneurysm.
Carotid-Cavernous Fistula
The fistulous connection may be directly between the cavernous carotid artery and the cavernous sinus or may be the result of a dural arteriovenous malformation in the parasellar region. Arterial pressures cause expansion of the cavernous sinus and dilatation of parasellar and orbital veins. Patients present with proptosis, chemosis, and visual loss. The presence of flow effects and flow artifacts confirms the diagnosis on MR images.
Inflammation
Tolosa-Hunt syndrome
Patients present with painful ophthalmoplegia and visual deficits. Similar to orbital pseudotumor pathologically, Tolosa-Hunt syndrome is also characterized by occasional spontaneous remission, recurrent attacks, and prompt response to steroids. The granulomatous inflammation can lead to cavernous sinus thrombosis and secondary arteritis of the cavernous carotid artery. MRI reveals enlargement of the cavernous sinus and enhancement of the inflammatory tissue. Endnote
Sphenoid sinus infections
Inflammatory and infectious diseases of the sphenoid sinus can secondarily involve the sella and parasellar regions. Pyogenic and fungal infections can extend through the thin bone at the skull base to produce an epidural abscess. Extension into the cavernous sinus can lead to cranial nerve palsies, cavernous sinus thrombosis and carotid artery occlusion. Some of the fungal infections, such as aspergillosis and mucormycosis, are particularly aggressive and have a propensity to extend along vascular structures, leading to cerebral infarction and abscess formation. The combination of sphenoid sinus and intracranial involvement on plain and contrast-enhanced scans is the key to making the diagnosis.
Suprasellar Pathology
Craniopharyngioma
Craniopharyngiomas originate from epithelial remnants of Rathke's pouch, usually at the junction of the infundibulum and the pituitary gland. They are benign slow-growing tumors composed of both solid epithelial tissue and cystic components. The cysts contain variable amounts of cholesterol, keratin, necrotic debris, proteinaceous fluid and hemorrhage. Calcification is present in 75 to 85% of cases.
Craniopharyngiomas have a variable appearance on MR, depending on their solid or cystic nature and the specific cyst contents. The solid lesions are hypointense on T1-weighted images and hyperintense on T2-weighted images. The cysts also have a long T2, but if they have a high cholesterol content or methemoglobin, shortening of T1 results in high signal intensity on T1-weighted images. Other features of craniopharyngioma include truncation of the dorsum sellae and upward growth into the third ventricle. Calcification is not reliably detected with MR, a disadvantage for differential diagnosis. Endnote
Rathke's Cleft Cyst
These benign cysts arise from remnants of Rathke's cleft in the region of the pars intermedia. They are lined by a single layer of ciliated columnar or cuboidal epithelium, often containing goblet cells. Initially intrasellar, they enlarge and extend into the suprasellar region as they accumulate fluid, mucous, and cellular debris.
Rathke's cleft cysts are smoothly marginated and well-defined lesions. The MR signal characteristics are variable, depending on the cyst contents. The cyst capsule may enhance, but the lack of nodular enhancement helps distinguish these lesions from craniopharyngiomas. Endnote
Chiasmatic & Hypothalamic Gliomas
Chiasmatic gliomas occur primarily in children and young adults. Patients with neurofibromatosis are particularly at risk for developing optic and chiasmatic gliomas. These tumors are usually low grade but have a propensity to infiltrate along the visual pathways. Hypothalamic gliomas tend to behave more aggressively and produce symptoms earlier. They present with hypothalamic syndromes, such as diabetes insipidus, inappropriate ADH secretion, Fröhlich's syndrome, or disturbances of temperature, appetite, or metabolism.
Chiasmatic gliomas are usually isointense or slightly hypointense on T1-weighted images and hyperintense on T2-weighted images. Expansion of the chiasm and optic tracts is seen best on coronal images. The sagittal plane often provides a longitudinal view of the proximal optic nerves. Posterior extension to the lateral geniculate body and beyond into the optic radiations is displayed best on axial T2-weighted or gadolinium enhanced images. Endnote Cystic components may be present, and occasionally exophytic growth extends into the suprasellar and interpeduncular cisterns.
MR is especially good for detecting and delineating hypothalamic gliomas. Subtle deformity of the inferior recesses of the third ventricle can be visualized on coronal and sagittal views. These tumors have a tendency to infiltrate the adjacent thalamus and upper brain stem. Signal characteristics are similar to the chiasmatic gliomas, and they may also exhibit exophytic features. As a rule, both tumors enhance to a moderate degree and in a homogeneous fashion, except for the cystic portions.
Hamartoma of the Tuber Cinereum
These benign tumors consist of hyperplastic hypothalamic glial and neural tissue. Patients present with precocious puberty due to disruption of the normal hypothalamic inhibition of gonadotropin production during the prepuberty years. These lesions grow very slowly and often appear unchanged on serial imaging studies.
Hamartomas are sessile or pedunculated masses positioned between the infundibulum and mamillary bodies. They are usually isointense to brain on T1-weighted images and mildly hyperintense on T2-weighted images. The lack of contrast enhancement distinguishes these tumors from hypothalamic glioma and germinoma. Endnote
Lymphoma
Primary malignant lymphoma is a non-Hodgkin's lymphoma that occurs in the brain in the absence of systemic involvement. These tumors are highly cellular and grow rapidly. The hypothalamus and cavernous sinuses are favorite sites in the perisellar region. Most occur in patients who are immunocompromised secondary to chemotherapy, HIV infection, or in organ transplant recipients who are on immunosuppressant drugs. Lymphomas typically appear as homogeneous, slightly hyperintense masses on T2-weighted images. Intratumoral cysts, hemorrhage, or necrosis are unusual. Most lymphomas show bright homogeneous contrast enhancement.
Germinoma
This germ cell tumor occurs in children and young adults, most commonly in the pineal and suprasellar regions. Germinomas have a propensity to invade the hypothalamus and grow into the third ventricle, resulting in endocrine dysfunction. Dissemination through the CSF pathways is a known complication of germinoma.
Germinomas are most often isointense with the brain on T1- and T2-weighted images. A few lesions exhibit long T1 and T2, which may correlate with embryonal cell elements. These tumors are well defined and enhance to a moderate degree, usually without central necrosis, cystic change, or hemorrhage. Enhanced scans are essential to assess CSF spread of tumor. In young patients with germinoma, the difficulty of visualizing calcium is a disadvantage of MR, as this may be the only evidence of tumor.
Arachnoid Cyst, Epidermoid, Dermoid
Arachnoid cyst
Arachnoid cysts are CSF-containing cysts that are found in the middle fossa, posterior fossa, suprasellar cistern, or near the vertex. They are benign but slowly grow as they accumulate fluid, compressing normal brain structures. Arachnoid cysts are smoothly marginated and homogeneous. They are not calcified and do not enhance. The diagnosis is supported by the cyst fluid being isointense with CSF on all pulse sequences. Endnote
Epidermoid cyst
Epidermoid cysts are referred to as "pearly tumors" because of their glistening white appearance at surgery. They arise from epithelial cell rests in the basal cisterns. They are benign and grow slowly along the subarachnoid spaces and into the various crevices found at the base of the brain.
Intradural epidermoids are usually quite large with lobulated outer margins and an insinuating pattern of growth. They have a heterogeneous texture and variable signal intensity on MR. Endnote Most are slightly higher signal than CSF on both T1 and T2-weighted images. An occasional epidermoid has a very short T1 and appears bright on T1-weighted images. The heterogeneous signal pattern is likely related to varying concentrations of keratin, cholesterol, and water within the cyst, as well as the proportion of cholesterol and keratin in crystalline form. Calcification is sometimes present. Epidermoid tumors do not enhance with contrast.
Dermoid cyst
Dermoid cysts have both dermal and epidermal derivatives, accounting for their more varied histologic and MR appearance. They are primarily midline lesions, occurring in the pineal and suprasellar regions. Dermoids have some distinctive features on MR. They tend to be heterogeneous owing to the multiple cell types within them. Fatty components are common, producing high signal on T1-weighted images. Axial and sagittal scans may reveal a fat-fluid level, or a level between fat and matted hair within the cyst. Rupture of a dermoid and leakage of cyst contents into a ventricle or subarachnoid space may produce an ependymitis or meningitis, respectively.
Granulomatous Disease
Langerhan's cell histiocytosis
Formerly called histiocytosis X and eosinophilic granuloma, this disease is a multisystem disorder involving the skin, bones, orbit, lungs, and the CNS. Proliferation of histiocytes form granulomas in and around the hypothalamus and infundibulum. Diabetes insipidus is the most common presentation, but patients can also develop other endocrine dysfunctions or visual impairment. MRI typically shows a thickened infundibulum or a hypothalamic mass that is isointense on T1, hyperintense on T2-weighted images, and enhances with contrast material. The normal posterior pituitary bright spot is frequently absent. Endnote
Sarcoid
Sarcoidosis is a granulomatous disease of unknown etiology. In approximately 5% of cases, the CNS is involved as a granulomatous infiltration of the meninges and underlying parenchyma, most notably at the base of the brain. Cranial nerve palsies, chronic meningitis and hypothalamic-pituitary dysfunction are frequent manifestations. Sarcoidosis is generally a multifocal process. MR is well suited to imaging the focal pituitary and hypothalamic lesions. The basal cisterns may enhance diffusely in patients with meningeal sarcoidosis, but a nodular pattern usually distinguishes it from the infectious varieties. Endnote
Tuberculosis
Tuberculous meningitis remains an important disease, becoming more common as an infectious agent in AIDS patients. As a rule, the evolution is less rapid than in pyogenic infections. Vasculitis and cerebral infarction, caused by inflammatory changes in the basal cisterns, are more prevalent. The MR features of tuberculous meningitis are similar to the bacterial agents, but the chronic inflammation induces thick granulation tissue that produces a more striking enhancement pattern. A basal meningeal process associated with lacunar infarcts should suggest the diagnosis of tuberculosis.
Image Gallery
MRI
-
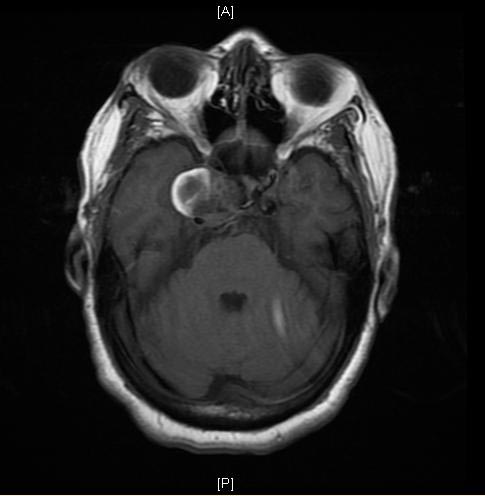
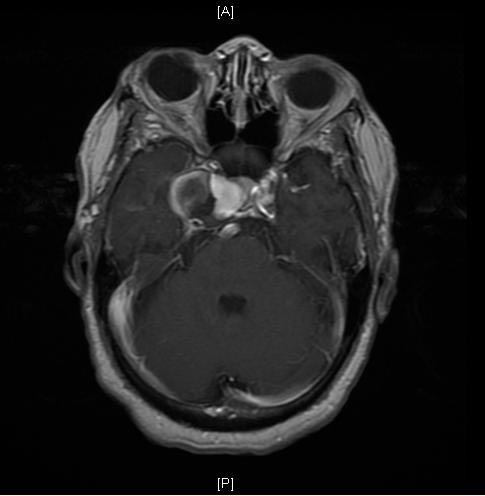
Cavernous sinus aneurysm
-
Cavernous sinus aneurysm
-
Cavernous sinus aneurysm
-
Cavernous sinus aneurysm
-
Cavernous sinus aneurysm
-
Cavernous sinus aneurysm
-
Cavernous sinus aneurysm