Mohs surgery
|
WikiDoc Resources for Mohs surgery |
|
Articles |
|---|
|
Most recent articles on Mohs surgery Most cited articles on Mohs surgery |
|
Media |
|
Powerpoint slides on Mohs surgery |
|
Evidence Based Medicine |
|
Clinical Trials |
|
Ongoing Trials on Mohs surgery at Clinical Trials.gov Clinical Trials on Mohs surgery at Google
|
|
Guidelines / Policies / Govt |
|
US National Guidelines Clearinghouse on Mohs surgery
|
|
Books |
|
News |
|
Commentary |
|
Definitions |
|
Patient Resources / Community |
|
Patient resources on Mohs surgery Discussion groups on Mohs surgery Patient Handouts on Mohs surgery Directions to Hospitals Treating Mohs surgery Risk calculators and risk factors for Mohs surgery
|
|
Healthcare Provider Resources |
|
Causes & Risk Factors for Mohs surgery |
|
Continuing Medical Education (CME) |
|
International |
|
|
|
Business |
|
Experimental / Informatics |
Editors-In-Chief: Martin I. Newman, M.D., FACS, Cleveland Clinic Florida, [1]; Michel C. Samson, M.D., FRCSC, FACS [2]
Overview
Mohs surgery, also known as chemosurgery, created by a general surgeon, Dr. Fredrick E. Mohs, is microscopically controlled surgery that is highly effective for common types of skin cancer, with a cure rate cited by most studies between 97% and 99.8%[1] for primary basal cell carcinoma, the most common type of skin cancer. Mohs procedure is also used for squamous cell carcinoma, but with a lower cure rate. Two isolated studies reported cure rate for primary basal cell cancer as low as 95% and 96% (see discussion on "Why is the Cure Rate so Varied?).[2][3][4] Recurrent basal cell cancer has a lower cure rate with Mohs surgery, more in the range of 94%.[5] It has been used in the removal of melanoma-in-situ (cure rate 77% to 98% depending on surgeon), and certain types of melanoma (cure rate 52%).[6][7] Another study of melanoma-in-situ revealed Mohs cure rate of 95% for frozen section Mohs, and 98 to 99% for fixed tissue Mohs method.[8][9] Other indications for Mohs surgery include dermatofibrosarcoma protuberans, keratoacanthoma, spindle cell tumors, sebaceous carcinomas, microcystic adnexal carcinoma, merkel cell carcinoma, Pagets's disease of the breast, atypical fibroxanthoma, leimyosarcoma, and angiosarcoma.[10] Because the Mohs procedure is micrographically controlled, it provides precise removal of the cancerous tissue, while healthy tissue is spared. Mohs surgery is relatively expensive when compared to other surgical modalities.[11] However, in anatomically important areas (eyelid, nose, lips), tissue sparing and low recurrence rate makes it a procedure of choice by many physicians.
History
Originally, Dr. Mohs used an escharotic agent made of zinc chloride and bloodroot (the root of the plant Sanguinaria canadensis, which contains the alkaloid sanguinarine). The original ingredients were 40.0 gm Stibnite, 10.0 gm Sanguinaria canadensis, and 34.5 ml of saturated zinc chloride solution.[12] This paste is very similar to "Hoxsey's paste" (see Hoxsey Therapy). Harry Hoxsey, a lay cancer specialist was developing a herbal tonic and paste designed to treat internal and external cancers. Hoxsey recommended applying paste to the affected area and within days to weeks, the area would necrose (cell death), separate from surrounding tissue and fall out. Dr. Mohs applied a very similar paste after experimenting with a number of compounds to the wound of his skin cancer patients. They were to leave the paste on the wound overnight, and the following day, the skin cancer and surrounding skin would be anesthetic, and ready to be removed. The specimen was then excised, and the tissue examined under the microscope. If cancer remained, more paste was applied, and the patient would return the following day. Later, local anesthetic and frozen section histopathology applied to fresh tissue allowed the procedure to be performed the same day, with less tissue destruction, and similar cure rate.[13] The term "chemosurgery" remains today, and is used synonymously with Mohs micrographic surgery.
Mohs procedure
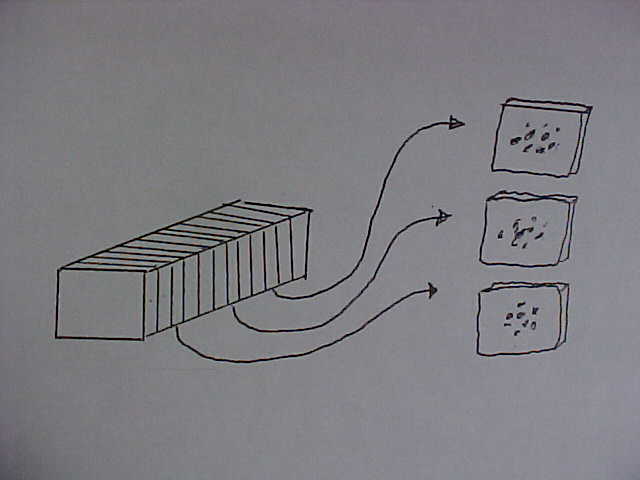
The Mohs procedure is essentially a pathology sectioning method that allows for the complete examination of the surgical margin. It is different from the standard bread loafing technique of sectioning,[14] where random samples of the surgical margin is examined.[15][16]
Mohs surgery is performed in four steps:
- Surgical removal of tissue (Surgical Oncology)
- Mapping the piece of tissue, freezing and cutting the tissue between 5 and 10 micrometers using a cryostat, and staining with hematoxylin and eosin (H&E) or other stains (including T. Blue)
- Interpretation of microscope slides (Pathology)
- Reconstruction of the surgical defect (Reconstructive Surgery)
The procedure is usually performed in a physician's office under local anesthetic. A small scalpel is utilized to cut around the visible tumor. A very small surgical margin is utilized, usually with 1 to 1.5 mm of "free margin" or uninvolved skin. The amount of free margin removed is much less than the usual 4 to 6 mm required for the standard excision of skin cancers.[17] After each surgical removal of tissue, the specimen is processed, cut on the cryostat and placed on slides, stained with H&E and then read by the Mohs surgeon/pathologist who examines the sections for cancerous cells. If cancer is found, its location is marked on the map (drawing of the tissue) and the surgeon removes the indicated cancerous tissue from the patient. This procedure is repeated until no further cancer is found.
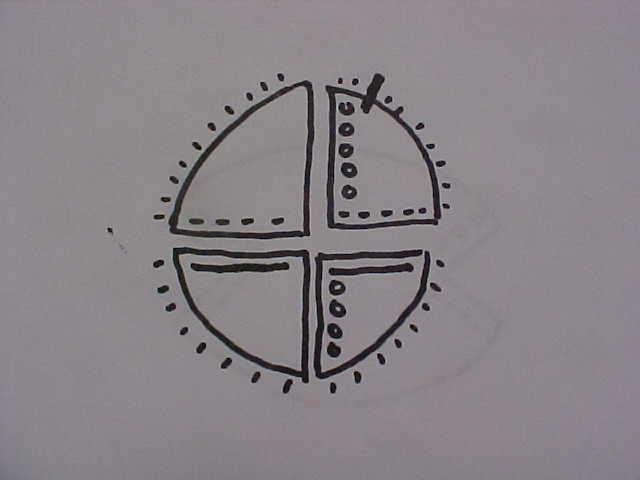
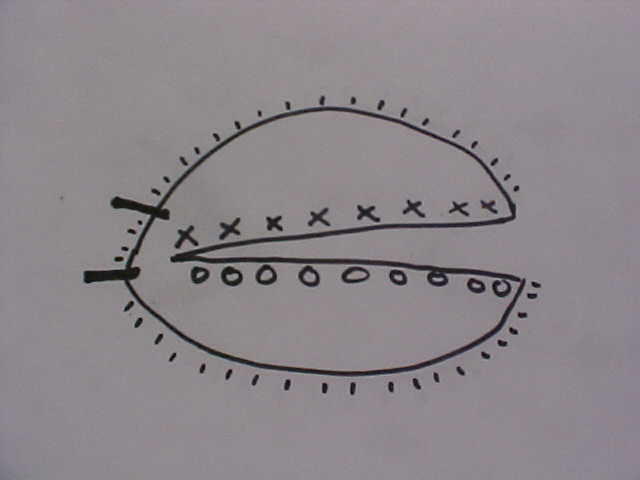
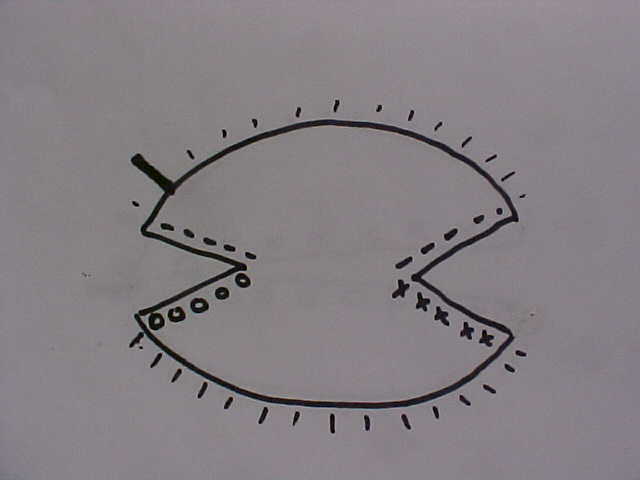
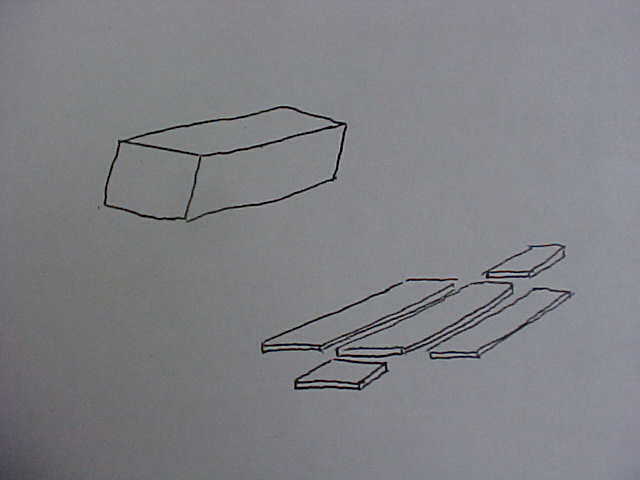
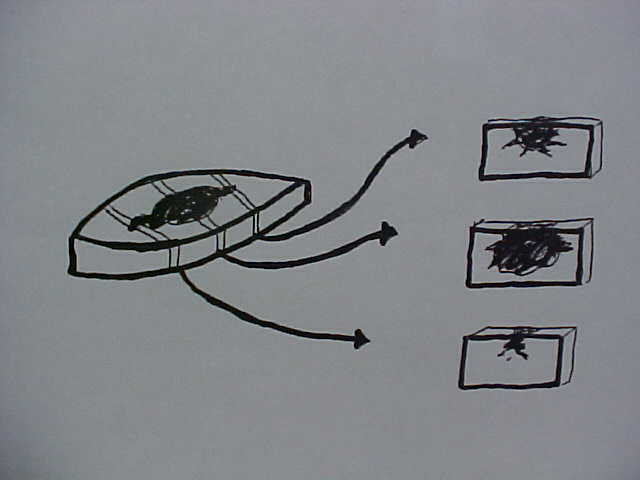
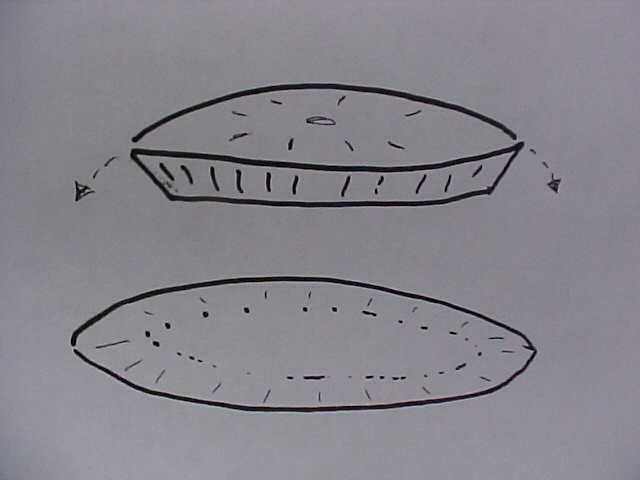
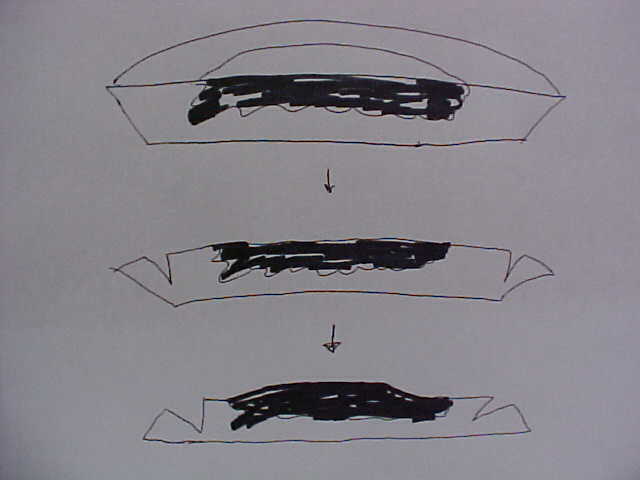
The method is well described in current references.[18][19][20] The mapping combined with the unique "smashing the pie pan" method of processing is the essential of Mohs surgery. If one imagines an aluminum pie pan as the blood covered surgical margin, and the top of the pie is the crust covered surface of the skin - the goal is to flatten the aluminum pie pan into one flat sheet, mark it, stain it, and examine it under the microscope. Another author uses the example of peeling the skin off an orange.[21] Imagine an orange cut in half as the Mohs layer. The peel is the surgical margin. One remove this peel and flatten it out on a glass slide to examine the roots of the invasive cancer. The mapping is simply how one stains and labels the sections for a microscopic examination. The sections can be processed in one piece[22] (using relaxing incisions at multiple points, or hemisectioned like a "Pac-Man" figure),[23] cut in halves, cut in quarters, or cut in multiple pieces. Single piece processing is acceptable for small cancers, and multiple piece sectioning facilitates processing and prevent artifacts. Single piece sectioning prevents errors introduced by soft, hard-to-handle tissue; or from accidental dropping or mislabeling of specimen. Multiple sectioning prevents compression artifacts, separation of tissue, and other logistical problems with handling large thin sheets of frozen skin.
Some physicians believe that frozen section histology is the same as Mohs micrographic surgery, and it is not.[24] Mohs surgery is performed using fresh tissue and frozen section histology. However, standard frozen section histology usually utilizes a random tissue sampling technique called "bread loafing". Bread loafing is a statistical sampling method which exams less than 5% of the total surgical margin (imagine pulling 5 slices of bread out of a whole loaf of sliced bread and examining only those 5 slices to visualize the whole loaf). In Mohs processing, the entire surgical margin is examined (imagine one who examined the entire outside crust of the same loaf of bread). In statistical terms, the more slices of bread one examines, the lower the "false negative" rate will become.[25] False negatives occur when a pathologist reads cancer excision as "free of residual carcinoma", even though cancer might be present in the wound and missed because of the random sampling.[26] In reality, most pathology labs examine only 3 to 8 sections of the "loaf" in their margin determination. While a diligent pathologist can cut and process a standard excision to get the same margin control as Mohs surgery, it is seldom done since tissue processing is very difficult in practice. The alternative to Mohs surgery is when a pathologist requests the processing to be done by "cutting through the block". Again, this method approaches that of Mohs surgery, but still is not as good. Cutting through the block will result in the random discarding of many slices, but does greatly decrease the incidence of "false negative" reports. Dr. Mohs perfected a simple and efficient way to "flatten" and examine the entire surgical margin.
Staining Convention
Each surgeon has their own convention. A typical convention is as follows[27]
Epidermis l l l l l l l l l l BLUE - - - - - - - - - RED --------------------------------- YELLOW O O O O O O O GREEN X X X X X X X Missing Epidermis V V V V V V V V V V
Differences between histology of transverse sections and vertical sections
Often, for legal purpose, a second opinion will be asked of a pathologist to review pathology slides from Mohs cases. Traditional histology of skin tissue uses vertical sectioning - with the subcutanous tissue at the bottom and the epidermis at the top. Mohs surgery uses tangential or horizontal sectioning, which can confuse the pathologists trained in the traditional method.
First, one has to determine the method of chromacoding or color coding. The orientation of the Mohs map must be able to distinguish between medial, lateral, superior, and inferior.
Next, one has to determine if the surgeon followed the convention of mounting only 2 sections per case; as preferred by some author;[28] or did he/she performed serial sectioning through the block as preferred by some author.[29] If serial sectioning is performed, the distance between sections should be confirmed. Some surgeons utilizes 100 micrometres between each sections, and some utilizes 200 micrometres between the first two sections, and 100 micrometres between subsequent sections (10 crank of tissue set at 6 to 10 micrometre is roughly equal to 100 micrometres if one allow for physical compression due to the blade).
Next, one determine if the entire epidermal border is present. Ideally 100% of the epithelial border should be present. Convention requires at least 95% of the epidermis to be present.[30] However, some surgeon will make an exception for some missing epithelium at the apices of an elliptical excision around the specimen. Ideally, oval sections should be performed. However, for practical purpose on some lesions, a surgeon might cut the Mohs section to approximate the final closure defect. The apexes are often 1 cm or more from the tumor, so clear margins at the apices can be ignored. Not ideal by convention, but appropriate on a case by case basis.
Next, one determine if the surgical margin is clear. With serial sectioning, one has to recreate the surgical specimen in a 3 dimensional way. The first section that touches the blade begin the 3 dimensional reconstruction. By using the 3-D reconstruction of the specimen, one can say that all the epithelial margin is present as one progresses from deep to superficial. If only 2 sections are present, ideally, both the sections should be clear. If the deeper sections is positive, one has to ascertain the distance between the section. Convention often call for a clear margin of at least 200 micrometres. For ambiguous structures that resembles both adnexal structure and carcinoma, following the serial sections will allow for one to identify the structure as benign or malignant. With the 2 slides method, this might be impossible to perform, as no 3-D reconstruction is possible with only 2 sections.
Carcinoma appearance under Mohs micrographic sectioning can be deceptively difficult. Tangential cut of squamous cell can mimic squamous cell carcinoma (but without the atypia). Sections through the buds of hair follicles resembles isolated islands of basal cell cancers, often even with retraction artifact. Serial section analysis is best for Mohs surgery. But one will often find cases where only 2 slides are mounted.[31]
It is best to leave the professional evaluation of Mohs section to an expert. The expert should not only be a pathologist who is familiar with one style of Mohs processing (i.e. 2 section mounting), one should also be familiar with all the sectioning protocols (whole tissue, pacman one piece,[32] double pacman one piece,[33] or multiple sections). Each methods has its limitation, but as long as good quality slides are cut - the end result is the same.
The Mohs Surgery Team
The team consists of the Mohs surgeon, histotechnician, pathologist and the reconstructive surgeon. The Mohs surgeon identifies the cancer and its margin, often with the aid of dermatoscopy. He removes the cancer under local anesthetic and prepares it for histology processing. This is accomplished by cutting the specimen (if required), staining the specimen for orientation, and sending it to the lab.
The histotechnician prepares the tissue for Mohs processing by flattening the surgical margin on a flat surface first. Then the flat surgical surface is mounted on a cryostat to be sectioned and prepared for glass slides to be read by the pathologist.
The pathologist examine the slide for residual tumors, and marks the location of the tumor on the pathology report and sends it back to the Mohs surgeon. He informs the Mohs surgeon when the surgery has completely removed the cancer.
The reconstructive surgeon does the plastic repair of the surgical defect in a cosmetic manner. Some Mohs surgeons utilize a plastic or reconstructive surgeon to repair the defect. Most Mohs surgeons perform their own surgical repair, except on exceptional cases.
There are some Mohs surgeons who fulfill all 4 roles - Mohs surgeon, histotechnician, pathologist and reconstructive surgeon. Most Mohs surgeons also perform the duty of pathologist and reconstructive surgeon. Regardless of who performs what procedures, any weakness in the link between these 4 individuals can result in a poor cure rate, or bad cosmetic outcome.
Why is the cure rate so varied?
These are topics for discussion, but errors introduced in the technique can introduce false negative errors. There are numerous reasons why the cure rate is not 100%. Some of Dr. Mohs data revealed a cure rate as low as 96%, but these were often very large tumor, and previously been treated by other modalities. Some authors claim that their 5 year cure rate for primary basal cell cancer exceeded 99% while other noted more conservative cure rate of 97%. The quoted cure rate for Mohs surgery on previously treated basal cell cancer is about 94%.[34]
1. Modern frozen section method. Frozen section histology does not give the added margin of safety by the cytotoxic Mohs paste,[35] originally used by Dr. Mohs. This paste might have destroyed any residual cancer cells not detected by the pathologist.
2. Missing epidermal margins. Ideally, the Mohs section should include 100% of the epidermal margin, but greater than 95% is often accepted.[36] Unfortunately, vigorous scrubbing, poorly controlled initial curettage, poor tissue health, technician's error, and surgeon's error can introduce areas missing epithelial margin. Some surgeon consider 70% epithelial margin acceptable, while other suggests 100% margin. In the ideal situation, 100% of the epithelial margin should be available to be reviewed on serial sectioning of the Mohs specimen.
3. Misreading of the pathology slide. It is difficult to differentiate between a small island of basal cell carcinoma and a hair follicle structure. Many Mohs surgeon limits their tissue processing to include only 2 sections of tissue.[37] This severely hampers their ability to determine if a structure is a hair follicle or a carcinoma. Two histologic sections can not fully distinguish these two nearly identical structures,[38] and can lead to either "false negative" or "false positive" errors by either calling a section clear of tumor, or calling a section positive for tumor, respectively. Serial sectioning of the tumor is preferred by other surgeons.[39] Surgeons who performs serial sectioning through the block of tissue (usually 100 micrometres apart) are assured the contiguous nature of his tumor, the distance of the tumor from the surgical margin, and is familiarized with the nature of the tumor. Serial sectioning also makes it easier to work with three dimensional tumor with difficult to compress margins.
4. Compression artifact, freezing artifact, cautery artifact, tissue folds, crush artifact from forceps, relaxing incision artifact, cartilage dropping out, fat compression, poor staining, dropping of tumor, etc.[40] These can be introduced as the tumor is "flattened". Stain can run from the surgical edge, and stain the surgical margin - giving a false impression that the entire surgical margin is clear, when it is not. While some surgeon unfamiliar with the "whole piece" or "PacMan"[41] methods of processing might suggest that multiple piece sectioning is better than one. The more tissue sections are cut, the more artifacts in staining and tissue malformation will be introduced. It is imperative for the surgeon to be fully familiar with tissue handling and processing; and not simply relying on a trained technologist to perform his sectioning.
5. Hard to see tumor in heavy inflammatory infiltrate.[42] This can occur with squamous cell carcinoma, especially when complicated with local infection, or intrinsic lymphoproliferative disorders (chronic lymphocytic leukemia). Because of abnormal peripheral blood profile, response to inflammatory skin conditions with patients with myelomonocytic leukemia can have appearance of atypical cells at sites of inflammation, confusing the Mohs surgeon.[43]
6. Perineural spread, and benign changes simulating perineural spread. Tumor spreading along a nerve can be difficult to visualize, and sometime benign plasma cells can surround the nerve, simulating cancer.[44]
7. Difficult to cut and process anatomical area.[45] Examples would be the ear, and other three dimensional structures like eyelids. The ability to make a scallop shaped incision is increasingly difficult when the surgical surface is no longer a flat plane, but is a three dimensional rigid structure.
8. Recurrent skin cancer with multiple islands of recurrence. This can occur with either previous excision, or after electrodessication and curettage. As these residual skin cancer are often bound in scar tissue, and present in multiple location in the scar of the previous surgical defect - they are no longer contiguous in nature. Some surgeons advocate the removal of the complete scar in the treatment of "recurrent" skin cancers. Others advocate removing only the island of local recurrence, and leaving the previous surgical scar behind. The decision is often made depending on the location of the tumor, and the goal of the patient and physician.
9. Unreported or underreported recurrence. Many patients simply will not return to the original surgeon to report a recurrence. Consulting surgeon on the repeat surgery will often not inform the first surgeon of the recurrence. The time it takes for a recurrent tumor to be visible to the patient might be 5 or more years. Quoted "cure" rates must be looked upon with the understanding that a 5 year cure rate might not necessary be correct. As basal cell carcinoma is a very slowly progressing tumor, a 5 year no recurrence rate might not be adequate. Longer follow up might be needed to detect a slow growing tumor left in the surgical scar.
10. Poor training of the surgeon/pathologist/histotechnologist. While Mohs surgery is essentially a technical method of tissue handling and processing, the skill and training of the surgeon can greatly affect the outcome. The house of card is built with a foundation of good tissue handling, good surgical skill and hemostasis, and the bricks are the tissue processing and staining technique. A surgeon without a good histotechnologist is a house built with straw, and a histotechnologist without a good surgeon can not produce quality slides. While originally, surgeons learned the procedure by spending a few hours to several months with Dr. Mohs;[46] today, surgeons complete residency and fellowship spending hundreds of hours observing and doing Mohs surgery. It is highly encouraged that a physician interested in learning Mohs surgery should spend extended time observing, cutting, processing, and staining Mohs specimens. The histology block should be correctly mounted and cut the first time, as there is no second chances in Mohs histology. It is not a procedure that can be taught or learn in one weekend. Many residency and Mohs fellowship continue to teach the processing of only 2 Mohs sections per tumor.[47]
Irrespective of the problems associated with Mohs surgery, a true cure rate approaching 100% can occur with primary basal cell carcinoma (previously untreated) if proper respect of the physician's limitation, the procedure's limitation, and his laboratory staff's limitation. Conservative approach such as serial sectioning, good staining technique, and conservative Mohs margin (example: tumor at least 200 micrometre from the surgical margin) can assure the lowest recurrence rate.
Comparison to other modalities of treatment

It often occurs in medicine as in real life, "When you go to Midas, you get a muffler". Mohs surgery is not the answer for all skin cancers. Studies comparing the effectiveness of Mohs surgery to other modalities often fail to specify surgical margin, method of processing (bread loafing with 3 or 4 sections, bread loafing with 0.1 mm spacing, margin controlled, frozen section vs. standard histology); leaving little argument one way or another. Once a pathologist understands the simplistic nature of Mohs surgery, and its margin control ability - little need is called for clinical trial comparing Mohs surgery to surgical excision.
In reality, Mohs micrographic surgery is nothing more than frozen section histology using a unique peripheral margin control tissue processing technique. There is nothing magical about its cure rate or why years of training is required. When compared to many other described peripheral margin control tissue processing technique - the end result is the same - allowing for the complete examination of 100% of the surgical margin. The method is unique only in that it is a simple way to handle soft, hard to cut tissue. Once learned, any pathologists currently doing frozen section histology would realize how simple the technique is. It is better than doing serial bread loafing at 0.1 mm interval for improved false negative error rate simply in requiring less time, less tissue handling, and fewer glass slides mounted. Once mounted as tangential or horizontal sections, the pathologist simply has to relearn how to visualize skin structure on a tangential to horizontal view. In absent of a Mohs trained pathologist, peripheral sectioning followed by horizontal sectioning of the remaining center is equivalent to the Mohs method.[48][49]
The clinical quotes for cure rate of Mohs surgery is from 97% to 99.8% after 5 years for newly diagnosed basal cell cancer, decreasing to 94% or less for recurrent basal cell cancer. Radiation oncologists quote cure rate from 90 to 95% for BCC's less than 1 or 2 cm, and 85 to 90% for BCC's larger than 1 or 2 cm. Surgical excision cure rate varies from 99% for wide margin (4 to 6 mm) and small tumor, to as low as 70% for narrow margins applied to large tumors. Here the weakness of the procedure is the histopathological processing, and not the surgeon himself. The fault of the surgeon is lack of understanding pathology laboratory methods, and failing to follow the standard of care for adequate surgical margin. Usually the cure rate using standard bread loafing is very low for narrow surgical margin and a large tumor, and very high for large margins on small tumors.[50][51][52] It is the pathology lab that makes the difference, especially when frozen section is utilized in the operating theater. A randomized study assigning patients with recurrent facial basal cell cancer to either Mohs surgery or standard excision revealed no statistical difference in the treatment of primary basal cell carcinoma. It found a higher cure rate with Mohs surgery in the treatment of recurrent basal cell carcinoma (5 year recurrence rate of 2.4% for Mohs vs 12.1% for standard).[53]
Cosmetic appearance for Mohs surgery is very good, if combined with good reconstructive surgical skills. Some Mohs surgeon utilize a plastic or reconstructive surgeon for the closure, and some Mohs surgeon perform the reconstruction by himself. There are dermatologists who are great reconstructive surgeons, and plastic surgeons who are poor reconstructive surgeons. In certain area, the tip of the nose, and the nasal ala, Mohs surgery can result in significant deformity, and might require multiple staged reconstruction to rebuild the nose cosmetically. Radiation offers a very good non-traumatic option in these difficult to reconstruct areas.
In choosing a Mohs surgeon or reconstructive surgeon, it is mandatory that a patient request to see pictorial representation of his/her previous work. Then one can proceed to make a decision whether the Mohs surgeon should also be the reconstructive surgeon.
Controversy About Mohs Surgery
Few individuals argue about the cure rate for Mohs, especially pathologists familiar with the procedure.[54] However, in recent years, a few surgeons attempted to throw the baby out with the bath water by claiming that Mohs surgery is no better than standard excision based on one study.[55][56] The author in this study did not conclude the adequacy of the study as it is limited in size and short duration of the study (30 months). Extensive studies performed by Dr. Mohs involving thousands of patients with both fixed tissue and fresh tissue cases have been reported in the literature.[57] Other surgeons repeated the studies with also thousands of cases, with nearly the same results.[58]
Clinical 5 year cure rates with Mohs surgery: 1. 4085 cases of primary and recurrent cancer of face, scalp, and neck. Cure rate of 96.6%.[59] 2. 1065 cases of squamous cell carcinoma of face, scalp, and neck - cure rate 94.8%[60] 3. 2075 cases of basal cell cancer of the nose both primary and recurrent, cure rate 99.1%.[61] 4. Cure rate for basal cell cancer of the ear, less than 1 cm, 124 cases, cure rate 100%.[62] 5. Cure rate of basal cell cancer of the ear, 1 to 2 cm, 170 cases, 100%. One needs to keep in mind that the cases performed by Dr. Mohs were for large and extensive tumors, often treated numerous times before by other surgeons. Regardless, his cure rate for small primary tumors either were 100% or near 100% when separated out from larger or recurrent tumors.
Experienced Mohs surgeons have reported cure rates for melanoma-in-situ from 95% to 98% (depending on if it is small MIS, or lentigo maligna variant), much higher than previously reported by Dr. Mikhail of 77%.[63]
These are only a small number of cases reported by Dr. Mohs, and numerous other articles by other authors have shown tremendous cure rates for primary basal cell carcinoma. However, with studies by Smeet, et al. showing a Mohs cure rate of about 95%, and another study in Sweden showing Mohs cure rate of about 94%;[64] we really have to question if methodology practiced by Mohs surgeons around the world is of the same standard. We also will have to question if the standard 2 sections performed by some Mohs surgeons is adequate to control for false negative Mohs reports.
Where Mohs surgery is allowed
An example where clinical guidelines are issued by insurance companies; these guidelines are not indication that Mohs is the best method for the cancers described. These guidelines are subjective (why is younger than 40 years old a criterion?), and might not have any clear objective basis. Clinical guidelines currently adapted by Medicare insurance of the United States:[65]
Medicare will cover reimbursement for Mohs micrographic surgery for accepted diagnoses and indications as listed below.
1. Basal Cell, Squamous Cell, or Basalosquamous Cell Carcinomas in anatomic locations where they are prone to recur:
- Central facial areas, periauricular, nose, and temple areas of the face (the so-called "mask area" of the face)
- Lips, cutaneous and vermilion
- Eyelids and periorbital areas
- Auricular helix and canal
- Chin and mandible
2. Other Skin lesions: -Angiosarcoma of the skin -Keratoacanthoma, recurrent -Dermatofibrosarcoma protuberans -Malignant fibrous histiocytoma -Sebaceous gland carcinoma -Microcystic adnexal carcinoma -Extramammary Paget's disease -Bowenoid papulosis -Merkel cell carcinoma -Bowen's disease (squamous cell carcinoma in situ) -Adenoid type of squamous cell carcinoma -Rapid growth in a squamous cell carcinoma -Longstanding duration of a squamous cell carcinoma -Verrucous carcinoma -Atypical Fibroxanthoma -Leiomyosarcoma or other spindle cell neoplasms of the skin -Adenocystic carcinoma of the skin -Erythroplasia of Queryrat -Oral and central facial, paranasal sinus neoplasm -Apocrine carcinoma of the skin -Malignant melanoma (facial, auricular, genital and digital) when anatomical or technical -difficulties do not allow conventional excision with appropriate margins.
-Basal Cell carcinomas, squamous cell carcinomas, or basalosquamous carcinomas that have one or more of the following features:
- o Recurrent
- o Aggressive pathology in the following areas: Hands and feet, Genitalia, and Nail unit/periungual
- o Large size (2.0 cm or greater)
- o Positive margins on recent excision
- o Poorly defined borders
- o In the very young (<40 years age)
- o Radiation-induced
- o In patients with proven difficulty with skin cancers or who are immunocompromised
- o Basal cell nevus syndrome
- o In an old scar (e.g., a Marjolin's ulcer)
- o Associated with xeroderma pigmentosum
- o Perineural invasion on biopsy
- o Deeply infiltrating lesion or difficulty estimating depth of lesion
3. Laryngeal Carcinoma
Future applications of Mohs surgery
Mohs surgery can be applied to any relatively non-aggressive locally invasive tumors with contiguous growth pattern (i.e. no skipped growth, or metastasis). Today, most Mohs procedures are performed by dermatologists. However, pathologists, plastic surgeons, and otolaryngologists[66] have been trained and are ulitizing Mohs surgery in their practice as well. Hopefully, as more physicians are trained in the method, Mohs surgery can be applied to other organs systems beside the skin. The limitation of this application to other tumors (i.e. prostate cancer, cervical cancer, laryngeal cancer) is that the tumor must be in the earliest stages and no metastasis has occur. The second problem with Mohs surgery is the prolonged procedural time, which might require prolonged general anesthesia.
Currently, the American College of Mohs Surgery has limited training to physicians who have done a dermatology residency.[67] The American Society for Mohs Surgery continues to encourage the training of physicians of all specialties to learn and apply the method invented by Dr. Frederick Mohs. The argument against physicians of other specialties than dermatology gaining Mohs training is that they are not adequately trained in dermatopathology. The argument for training other physicians beside dermatologists is that most Mohs surgeon do not make the initial diagnosis of the skin cancer - thus misdiagnosis can be avoided. The pathology of Mohs sections are then limited to a few easily identifiable cancers; and the pathology of normal skin is simple enough to gain in a short preceptorship; even if you are not a dermatologist or a pathologist.
Dr. Mohs, a general surgeon, encouraged physicians of all surgical specialties to learn and apply his technique to the treatment of skin cancer; it is understood that he never intended to limit his method to be utilized by dermatologists alone. In countries where dermatology is not well developed, the Mohs procedure can easily be learned by any surgeon or pathologist after a short preceptorship - the same way Dr. Mohs taught many current Mohs surgeons.
This is a direct quote of Dr. Frederick Mohs in his book's preface:
"The book should be useful to physicians who may be called on to treat or advise regarding treatment of skin cancers and other conditions that are described. This includes dermatologists, surgeons, plastic surgeons, otolaryngologists, gynecologists, urologists, proctologists, pathologists, internists, and general practitioners."
From: Frederic E. Mohs, B.Sc., M.D. Clinical Professor of Surgery, University of Wisconsin. CHEMOSURGERY, Microscopically Controlled Surgery For Skin Cancer, Charles C. Thomas, Publisher, 1956. p. vii.
Associations
The American College of Mohs Surgery is the organization that sets standards of care for fellowship trained Mohs surgeons who perform Mohs surgery as a primary function of their practice.
The American Society of Mohs Surgery is an organization of dermatologists who perform dermatology and Mohs surgery in their practice. ASMS Mohs surgeons are certified by a written and practical exam, and are required to submit to yearly peer review of their cases.
The American Board of Medical Subspecialities is in the process of reviewing Mohs micrographic surgery as a separate subspecialty. Mohs surgery has not been recognized as a separate subspeciality and there is no certifying board for Mohs Surgery at this time.
The American Academy of Dermatology is the largest organization of board certified dermatologists, many of whom perform dermatologic and Mohs micrographic surgery. With a membership of over 15,000, it represents virtually all practicing dermatologists in the United States and Canada and has specific member information regarding those performing Mohs micrographic surgery.
The American Osteopathic College of Dermatology is the only organization that recognized Mohs surgery as a separate subspecialty. The organization offers board certification exam through the auspice of the American Osteopathic Association. The recipient of the board certification receives a certificate of added qualification (CAQ) to the primary board certification of dermatology. Currently American Osteopathic College of Dermatology is the only organization offer this credential to mohs surgeons.[68]
The American Society for Dermatologic Surgery founded in 1970 is the largest organization of board certified dermasurgeons with over 5000 members who perform dermatologic surgeries including Mohs micrographic surgery.
The Association of Academic Dermatologic Surgeons has board certified dermasurgeon professors who have faculty appointments at major teaching hospitals and universities and are engaged in training medical students and residents in the practice of dermatologic surgery and Mohs micrographic surgery.
Mohs Surgery Case Studies
Photos courtesy of Dr. B. Cowan
CASE STUDY 1: Left Nasal Rim Skin Cancer
CASE STUDY 2: Right Lower Lip Skin Cancer
CASE STUDY 3: Left Temple Basal Cell Cancer
References
- ↑ George, R. Mohs Micrographic Surgery. 1991, W.B. Saunders Co., p. 13.
- ↑ Smeets NW, et al. Surgical excision vs Mohs' micrographic surgery for basal-cell carcinoma of the face: randomised controlled trial. Lancet. November 13, 2004-19;364(9447):1766-72.
- ↑ http://www.ncbi.nlm.nih.gov/pubmed/15541449?dopt=Abstract
- ↑ Wennberg, AM., et al. Five-year results of Mohs' micrographic surgery for aggressive facial basal cell carcinoma in Sweden. Acta Derm Venereol. 1999 Sep;79(5):370-2.
- ↑ George, R. Mohs Micrographic Surgery. 1991, W.B. Saunders Co., p. 7.
- ↑ Mikhail, G. Mohs Micrographic Surgery. 1991, W.B. Saunders. p 4.
- ↑ Gross, K.G., et al. Mohs Surgery, Fundamentals and Techniques. 1999, Mosby. pp.211-220
- ↑ Bene, NI, et al. Mohs micrographic surgery is accurate 95.1% of the time for melanoma in situ: a prospective study of 167 cases Dermatol Surg. 2008 May;34(5):660-4.
- ↑ Am J Clin Dermatol. 2005;6(3):151-64.Links Lentigo maligna: prognosis and treatment options. Stevenson O, Ahmed I.
- ↑ Gross, K.G., et al. Mohs Surgery, Fundamentals and Techniques. 1999, Mosby. pp. 193-203.
- ↑ http://www.cancer.org/docroot/CRI/content/CRI_2_4_4X_Treatment_of_Basal_Cell_Carcinoma_51.asp
- ↑ Mohs, F. Chemosurgery, Microscopically Controlled Surgery for Skin cancer. 1978, Charles C. Thomas Publisher. ISBN 0-398-03725-6. pp. 3-6.
- ↑ Mikhail, G. Mohs Micrographic Surgery. 1991, Saunders. pp. 3-4.
- ↑ Maloney, M.E. et. al. Surgical Dermatopathology. Blackwell Science, 1999. p. 112-113.
- ↑ Mikhail, G. Mohs Micrographic Surgery. 1991, Saunders, pp. 13-14.
- ↑ Bowen G, White G, Gerwels J, = Mohs micrographic surgery. Am Fam Physician. 2005. 72(5) pages = 845–8.Full text
- ↑ http://www.bccancer.bc.ca/HPI/CancerManagementGuidelines/Skin/NonMelanoma/ManagementPolicies/start.htm
- ↑ Maloney, M.E. et. al. Surgical Dermatopathology. Blackwell Science, 1999. p. 1111-117.
- ↑ Gross, K.G., et al. Mohs Surgery, Fundamentals and Techniques. 1999, Mosby. pp.49-66
- ↑ Mikhail, G.R., Mohs Micrographic Surgery. 1991, WB Saunders. pp. 13-15.
- ↑ Maloney, et al. Surgical Dermatopathology. p. 113
- ↑ Gross, et al. Mohs Surgery. p. 83-84.
- ↑ Gross, et. al. Mohs Surgery. p. 86-89.
- ↑ Maloney, M.E. et. al. Surgical Dermatopathology. Blackwell Science, 1999. p. 116.
- ↑ Maloney, M.E. et. al. Surgical Dermatopathology. Blackwell Science, 1999. p. 114.
- ↑ Maloney, M.E. et. al. Surgical Dermatopathology. Blackwell Science, 1999. p. 118.
- ↑ Mikhail, et al. p 21
- ↑ Mikhail, G.R. et al. Mohs Micrographic Surgery. p. 307, first paragraph
- ↑ Gross, et al. Mohs surgery. p. 62
- ↑ Gross, et al. Mohs Surgery. p. 62.
- ↑ Mikhail, GR., et al. Mohs Micrographic Surgery. p. 307
- ↑ Gross KG, et al. Mohs Surgery. p. 87
- ↑ American Society for Mohs Surgery, teaching file of glass slides
- ↑ (Mikhail, G.R. Mohs Micrographic Surgery. pp. 6-7
- ↑ http://www.jtbaker.com/msds/englishhtml/z2280.htm
- ↑ Gross, et al. Mohs Surgery. p. 62
- ↑ Mikhail, GR., et al. Mohs Micrographic Surgery. p. 307
- ↑ Maloney, M.E. et. al. Surgical Dermatopathology. Blackwell Science, 1999. p. 134, and p. 453
- ↑ Gross, KG. et al, Mohs Surgery. p. 62 and 272.
- ↑ Maloney, M.E. et. al. Surgical Dermatopathology. Blackwell Science, 1999. p. 149-162.
- ↑ Gross, et. al. Mohs Surgery. p. 86-89.
- ↑ Maloney, M.E. et. al. Surgical Dermatopathology. Blackwell Science, 1999. p. 446.
- ↑ Maloney, M.E. et. al. Surgical Dermatopathology. Blackwell Science, 1999. p. 446.
- ↑ Maloney, M.E. et. al. Surgical Dermatopathology. Blackwell Science, 1999. p. 446-447.
- ↑ Mohs, F.E. CHEMOSURGERY, Microscopically Controlled Surgery For Skin Cancer, Charles C. Thomas, Publisher, 1956, p. 16
- ↑ Gross, et al. Mohs Surgery. p. 4
- ↑ Mikhail, GR., et al. Mohs Micrographic Surgery. p. 307
- ↑ Maloney, M.E. et. al. Surgical Dermatopathology. Blackwell Science, 1999. p. 113 and 116.
- ↑ Gross DA, et al. Cooperative frozen section surgery. J Dermatol Surg Oncol 1987;13:1085-1088.
- ↑ Maloney,ME et al. Surgical Dermatopathology. p. 110
- ↑ ARASH KIMYAI-ASADI, et al. Margin Involvement after the Excision of Melanoma In Situ: The Need for Complete En Face Examination of the Surgical Margins. Lancet Oncol. 2008 Dec;9(12):1149-56.
- ↑ Kimyai-Asadi A, et al. Accuracy of Serial Transverse Cross-Sections in Detecting Residual Basal Cell Carcinoma at the Surgical Margins of an Elliptical Excision Specimen. J Am Acad Dermatol vol. 53, 469 - 474, 2005
- ↑ Steijlen et al. Surgical excision versus Mohs' micrographic surgery for primary and recurrent basal-cell carcinoma of the face: a prospective randomised controlled trial with 5-years' follow-up.
- ↑ Maloney, et al. Surgical Dermatopathology. p. 116
- ↑ Smeets NW, et al. Surgical excision vs Mohs' micrographic surgery for basal-cell carcinoma of the face: randomised controlled trial. Lancet. November 13, 2004-19;364(9447):1766-72.
- ↑ http://www.ncbi.nlm.nih.gov/pubmed/15541449?dopt=Abstract
- ↑ Mohs,FE. Chemosurgery. Charles Thomas, 1978.
- ↑ Mikhail, et. al. Mohs Micrographic Surgery. WB Saunders, 1991.
- ↑ Mohs,FE. Chemosurgery. Charles Thomas, 1978. p.55
- ↑ Mohs,FE. Chemosurgery. Charles Thomas, 1978. p. 57
- ↑ Mohs,FE. Chemosurgery. Charles Thomas, 1978. p. 79
- ↑ Mohs,FE. Chemosurgery. Charles Thomas, 1978. p. 101
- ↑ Bene, NI, et al. Mohs micrographic surgery is accurate 95.1% of the time for melanoma in situ: a prospective study of 167 cases Dermatol Surg. 2008 May;34(5):660-4.
- ↑ Wennberg, AM., et al. Five-year results of Mohs' micrographic surgery for aggressive facial basal cell carcinoma in Sweden. Acta Derm Venereol. 1999 Sep;79(5):370-2.
- ↑ https://www.oxhp.com/secure/policy/derm_procedures_oma.html
- ↑ Gross, et al. Mohs surgery. pp. 248-260.
- ↑ http://www.mohscollege.org/acms/membership/fellowtrain.php
- ↑ DO-Online. "MOHS micrographic surgery is a subspecialty of dermatology that utilizes a modified type of surgical excision combined with a modified frozen section technique which offers the highest available cure rates for both primary and recurrent skin cancers.", DO-ONLINE, January 1, 2009.
External links
- American cancer society statement about Mohs surgery
- American Society of Mohs Surgery
- American College of Mohs Surgery
- "Mohs math – where the error hides"
- American Melanoma Foundation information