Midwifery
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]
Template:TOCright Midwifery is the term traditionally used to describe the art of assisting a woman through childbirth. In the modern context, this term is used to describe the activities of those health care providers who are experts in women's health care including giving prenatal care to expecting mothers. They attend the birth of the infant and provide postpartum care to the mother and her infant. Practitioners of midwifery are known as midwives, a term used in reference to both women and men (the term means "with woman").
Midwives are autonomous practitioners who are specialists in normal pregnancy, childbirth and the postpartum. They generally strive to help women have a healthy pregnancy and natural birth experience. Midwives are also primary care givers providing general women's health care. Midwives are trained to recognize and deal with deviations from the norm. Obstetricians, in contrast, are specialists in illness related to childbearing and in surgery. The two professions can be complementary, but often are at odds because obstetricians are taught to "actively manage" labor, while midwives are taught not to intervene unless necessary. [1]
Midwives refer to obstetricians when a woman requires care beyond her or his areas of expertise. In many jurisdictions, these professions work together to provide care to childbearing women. In others, only the midwife is available to provide care. Midwives are trained to handle certain situations that are considered abnormal, including breech birth and posterior position, using non-invasive techniques. In many areas of the world, traditional midwives, renamed "traditional birth attendants" by the World Health Organization (WHO) and other groups, are the only available providers for childbearing women.[citation needed]
Midwives once treated patients for female hysteria.
Defining midwifery
According to the WHO definition, a midwife is a person who, having been regularly admitted to a midwifery educational program that is duly recognised in the country in which it is located, has successfully completed the prescribed course of studies in midwifery and has acquired the requisite qualifications to be registered and/or legally licensed to practice midwifery. The educational program may be an apprenticeship, a formal university program, or a combination.
The midwife is recognised as a responsible and accountable professional who works in partnership with women to give the necessary support, care and advice during pregnancy, labour and the postpartum period, to conduct births on the midwife's own responsibility and to provide care for the infant. This care includes preventive measures, the promotion of normal birth, the detection of complications in mother and child, accessing of medical or other appropriate assistance and the carrying out of emergency measures.
The midwife has an important task in health counselling and education, not only for the woman, but also within the family and community. This work should involve antenatal education and preparation for parenthood and may extend to women's health, sexual or reproductive health and childcare.
A midwife may practice in any setting including in the home, the community, hospitals, clinics or health units.
Adopted by the International Confederation of Midwives, 19 July 2005
This definition is controversial and not everyone agrees with the exclusion of traditional midwives who in developing countries often are the only people available to assist women in birth.
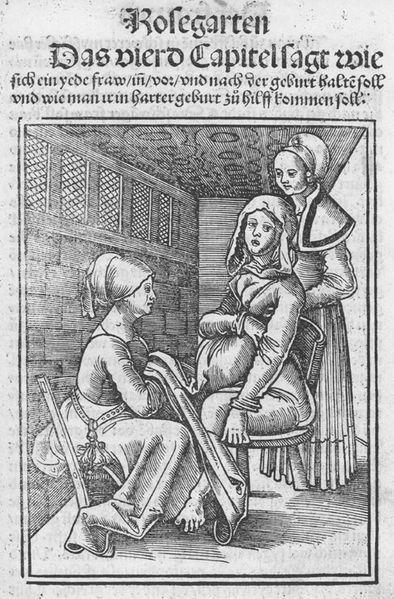
Historical perspective
Historically, midwifery has been one of the few medical practices dominated by female practitioners. From Agnodice in ancient Greece to the 18th century in Europe, the care of mothers and delivery of infants has been regarded, both by patients and by the medical profession, as appropriately carried out by women. In the 18th century, a division between surgeons and midwives arose, as medical men began to assert that their modern scientific processes were better for mothers and infants than the folk-medical midwives. Whether this was a valid claim or not can be seen in the entry for Justine Siegemund, a renowned seventeenth century German midwife, whose Court Midwife (1690) was the first female-authored German medical text.[citation needed]
At the outset of the 18th century in England, most babies were caught by a midwife, but by the onset of the 19th century, the majority of those babies born to persons of means had a surgeon involved. A number of excellent full length studies of this historical shift have been written.
German social scientists Gunnar Heinsohn and Otto Steiger have put forward the theory that midwifery became a target of persecution and repression by public authorities because midwives not only possessed highly specialized knowledge and skills regarding assisting birth, but also regarding contraception and abortion [2]. According to Heinsohn and Steiger's theory, the modern state persecuted the midwives as witches in an effort to repopulate the European continent which had suffered severe loss of manpower as a result of the bubonic plague (also known as the black death) which had swept over the continent in waves, starting in 1348.
They thus interpret the witch hunts as attacking midwifery and knowledge about birth control with a demographic goal in mind. Indeed, after the witch hunts, the number of children per mother rose sharply, giving rise to what has been called the "European population explosion" of modern times, producing an enormous youth bulge that enabled Europe to colonize large parts of the rest of the world.
While historians specializing in the history of the witch hunts have generally remained critical of this macroeconomic approach and continue to favor micro level perspectives and explanations, prominent historian of birth control John M. Riddle has expressed agreement.[3]
Midwifery in the United States
There are two main divisions of modern midwifery in the US: nurse-midwives and direct-entry midwives.
Nurse-midwives
Nurse-midwives were introduced in the United States in 1925 by Mary Breckinridge for use in the Frontier Nursing Service (FNS). Mrs. Breckinridge chose the nurse-midwifery model used in England and Scotland because she expected these nurse-midwives on horse back to serve the health care needs of the families living in the remote hills of eastern Kentucky. This combination of nurse and midwife was very successful. The Metropolitan Life Insurance Company studied the first seven years of the FNS, and reported a substantially lower maternal and infant mortality rate than for the rest of the country. The report concluded that if this type of care was available to other women in the USA thousands of lives would be saved, and suggested nurse-midwife training should be done in the USA. Mrs. Breckinridge opened the Frontier Graduate School of Midwifery in 1939 the first nurse-midwifery education program in the USA that is still educating nurse-midwives today http://www.frontierschool.edu/. In the United States, nurse-midwives are advanced practice nurses who have specialized in the practice of obstetrical and gynecological care of relatively healthy women. In addition to a registered nursing license, many nurse-midwives have a master's degree in nursing, public health, or midwifery. Nurse-midwives practice in hospitals, medical clinics and private offices and may deliver babies in hospitals, birth centers and at home. They are able to prescribe medications in all 50 states. Nurse-midwives provide care to women from puberty through menopause. Nurse-midwives may work closely with obstetricians, who provide consultation and assistance to patients who develop complications. Often, women with high risk pregnancies can receive the benefits of midwifery care from a nurse-midwife in collaboration with a physician. Currently, 2% of nurse-midwives are men. The American College of Nurse-Midwives accredits nurse-midwifery education programs and serves as the national professional society for the nation's certified nurse-midwives. At present approximately 5500 Certified Nurse-Midwives are practicing in the U.S.[citation needed]
Direct-entry midwives
A direct-entry midwife is educated in the discipline of midwifery in a program or path that does not also require her to become educated as a nurse. Direct-entry midwives learn midwifery through self-study, apprenticeship, a midwifery school, or a college- or university-based program distinct from the discipline of nursing. A direct-entry midwife is trained to provide the Midwives Model of Care to healthy women and newborns throughout the childbearing cycle primarily in out-of-hospital settings.
Under the umbrella of "direct-entry midwife" are several types of midwives:
A Certified Professional Midwife (CPM) is a knowledgeable, skilled and professional independent midwifery practitioner who has met the standards for certification set by the North American Registry of Midwives (NARM) and is qualified to provide the midwives model of care. The CPM is the only US credential that requires knowledge about and experience in out-of-hospital settings. At present, there are approximately 900 CPMs practicing in the US.
A Licensed Midwife is a midwife who is licensed to practice in a particular state. Currently, licensure for direct-entry midwives is available in 24 states.
The term "Lay Midwife" has been used to designate an uncertified or unlicensed midwife who was educated through informal routes such as self-study or apprenticeship rather than through a formal program. This term does not necessarily mean a low level of education, just that the midwife either chose not to become certified or licensed, or there was no certification available for her type of education (as was the fact before the Certified Professional Midwife credential was available). Other similar terms to describe uncertified or unlicensed midwives are traditional midwife, traditional birth attendant, granny midwife and independent midwife. [citation needed]
The American College of Nurse-Midwives (ACNM) also provides accreditation to non-nurse midwife programs, as well as colleges that graduate nurse-midwives. This credential, called the Certified Midwife, is currently recognized in only three states (New York, New Jersey, and Rhode Island). All CMs must pass the same certifying exam administered by the American Midwifery Certification Board for CNMs. At present, there are approximately 50 CMs practicing in the US.[citation needed]
The North American Registry of Midwives (NARM) is a certification agency whose mission is to establish and administer certification for the credential "Certified Professional Midwife" (CPM). CPM certification validates entry-level knowledge, skills, and experience vital to responsible midwifery practice. This certification process encompasses multiple educational routes of entry including apprenticeship, self-study, private midwifery schools, college- and university-based midwifery programs, and nurse-midwifery. Created in 1987 by the Midwives' Alliance of North America (MANA), NARM is committed to identifying standards and practices that reflect the excellence and diversity of the independent midwifery community in order to set the standard for North American midwifery.
Practice in the United States
Midwives work with women and their families in any number of settings. While the majority of nurse-midwives work in hospitals, some nurse-midwives and many non-nurse-midwives work within the community or home. In many states, midwives form birthing centers where a group of midwives work together. Midwives generally support and encourage natural childbirth in all practice settings. Laws regarding who can practice midwifery and in what circumstances vary from state to state, and some midwives practice outside of the law.
Missouri Controversy
Direct entry midwifery is unlawful in Missouri and practicing without a CNM license is a felony. However, on 26 May 2007 the Missouri Legislature passed a bill which provides tax incentives for those who purchase their own insurance in order to increase private health coverage for the uninsured. Attached to this legislation was a one sentence provision added by Sen. John Loudon which effectively legalizes certain direct entry midwifery. Although such measures had been previously been rejected by the legislature, Loudon was able to attach the provision undetected by use of the word tocology (word of Greek origin that means the practice of obstetrics and childbirth) rather than any reference to midwifery. Despite protests from some members of the legislature, Gov. Matt Blunt signed the bill into law. [4] A circuit judge issued a temporary restraining order on 03 July 2007 barring the implementation of the law, which was to take effect on 28 August 2007. [5] Following a 02 August 2007 hearing, the judge ruled the midwifery law illegal. A Columbia, Missouri-based midwives association plans to appeal the decision to the Missouri Supreme Court. [6]
Midwifery in the United Kingdom
Midwives are practitioners in their own right in the United Kingdom, and take responsibility for the antenatal, intrapartum and postnatal care of women, up until 28 days after the birth, or as required thereafter. Midwives are the lead health care professional attending the majority of births, mostly in a hospital setting, although home birth is a perfectly safe option for many births. There are a variety of routes to qualifying as a midwife. Most midwives now qualify via a direct entry course, which refers to a three- or four-year course undertaken at university that leads to either a degree or a diploma of higher education in midwifery and entitles them to apply for admission to the register. Following completion of nurse training, a nurse may become a registered midwife by completing an eighteen-month post-registration course (leading to a degree qualification), however this route is only available to adult branch nurses, and any child, mental health, or learning disability branch nurse must complete the full three-year course to qualify as a midwife. Midwifery students do not pay tuition fees and are eligible for financial support for living costs while training. Funding varies slightly depending on which country within the UK the student is in and whether the course they are on is a degree or diploma course. For direct entry students funding is in the form of either a non-means-tested bursary or a combination of student loan and means-tested bursary, while post-registration students are normally seconded by their employer and are paid a salary and have their fees paid for them.[citation needed]
All practicing midwives must be registered with the Nursing and Midwifery Council and also must have a Supervisor of Midwives through their local supervising authority. Most midwives work within the National Health Service, providing both hospital and community care, but a significant proportion work independently, providing total care for their clients within a community setting. However, recent government proposals to require insurance for all health professionals is threatening independent midwifery in England. [7]
To be a midwife is to be responsible, at all times, for the woman for whom you are caring, to know when to refer complications to medical staff, to act as the woman's advocate, and to ensure the mother retains choice and control over her childbirth experience. Many midwives are opposed to the so-called "medicalisation" of childbirth, preferring a more normal and natural option, to ensure a more satisfactory outcome for mother and baby.[citation needed]
Midwife training
Midwifery training is considered one of the most challenging and competitive courses amongst other healthcare subjects. Most midwives undergo a 32 month vocational training program, or a 18 month nurse conversion course (on top of the 32 month nurse training course). Thus midwives potentially could have had up to 5 years of total training.
Midwives may train to be community Health Visitors (as may Nurses).
Community midwives
Many midwives also work in the community. The roles of community midwives include the initial appointments of pregnant women, running clinics, postnatal checks in the home, and attending home births.
Midwife phraseology
In the UK there is a common guideline from the Nursing and Midwifery Council outlining a standard set of phrases to encourage and help the woman through labour. These phrases are designed and standardised to make clear the instructions for maximal clarity and effect. From the Midwifery Handbook 2005 published by the Nursing and Midwifery Council, here are a few of the most commonly used phrases:
- "Give me a long push, long push, long push"
- "Big breath, chin down, push out down below"
- "Imagine you are constipated, give me a big push"
- "You can do it, you will do it, I want to see you push"
- "It is almost over (+ name), I can see the baby's head, the hardest part is over"
- "You've done it, congratulations!"
Many midwives rote learn these phrases as they are designed by psychologists to be most effective for promoting labour and enhancing patient birthing experience.
Midwifery in Canada
Midwifery was reborn as a profession in Canada in the 1960s, along with other aspects of health care reform that trace their roots to that decade of societal ferment and change. After several decades of intensive political lobbying by midwives and consumers, regulated midwifery has become part of the health system in the provinces of British Columbia, Alberta, Manitoba, Ontario, and Quebec, and in the Northwest Territories and Nunavut. Alberta does not publicly fund midwifery. Saskatchewan has legislation but has not integrated midwifery yet. Midwifery is not yet legally recognised in the Atlantic provinces of New Brunswick, Prince Edward Island, Newfoundland and Labrador, or Nova Scotia. The governments of Nova Scotia and New Brunswick have introduced midwifery legislation but have yet to commit to funding midwifery services if and when the bills pass.
Midwives in Canada have come from a variety of backgrounds, including nurse-midwifery, lay midwifery and direct-entry midwifery. However, they are all simply known as 'midwives', regardless of their original training. From the original 'alternative' style of midwifery in the 1960s and 1970s, midwifery practice has become somewhat standardized in all of the regulated provinces: midwives offer continuity of care within small group practices, choice of birthplace, and a focus on the woman as the primary decision-maker in her maternity care. When women experience deviations from normal in their pregnancies, midwives consult with other health care professionals. The women's care may continue with the midwife, in collaboration with an obstetrician or other health care specialist; her care may be transferred to an obstetrician or other health care specialist, temporarily or for the remainder of her pregnancy and birth. Woman as primary decision maker, informed choice, and choice of birth place are primary tenets of midwifery care in Canada.
Three provinces now offer midwifery education, which consists of a four year university baccalaureate degree in midwifery. In British Columbia, the program is offered at the University of British Columbia. In Ontario, the Midwifery Education Program is offered by a consortium of McMaster University, Ryerson University and Laurentian University. In Quebec, the programme is offered at the Université du Québec à Trois-Rivières. In northern Quebec, Inuit women are being educated to be midwives in their own communities. A program for First Nations midwifery students will open soon in Manitoba.
The legislation of midwifery has brought midwives into the mainstream of health care with universal funding for services (except in Alberta), hospital privileges, rights to prescribe medications commonly needed during pregnancy and birth, and rights to order blood work and ultrasounds for their own clients. To protect the tenets of midwifery and keep midwives providing woman-centered care, the regulatory bodies and professional associations have legislation and standards in place to provide protection, particularly for choice of birth place (see home birth), informed choice about care, and continuity of care. Midwives in Ontario have had malpractice insurance since prior to legislation, and all other legislated midwives also have malpractice insurance.
Prior to legislative changes, very few Canadian women had access to midwifery care (in part because it was not funded by the health care system). Legislating midwifery has made midwifery services available to a wide and diverse population of women.
Midwifery in New Zealand
Midwifery regained its status as an autonomous profession in New Zealand in 1990. The Nurses Amendment Act restored the professional and legal separation of midwifery from nursing, and established midwifery and nursing as separate and distinct professions. Nearly all midwives gaining registration now are direct entry midwives who have not undertaken any nursing training. Registration requires a Bachelor of Midwifery degree. this is currently a three year full time programme but is in the process of being reviewed by the New Zealand midwifery regulatory authority..
Women must choose one of a midwife, a General Practitioner or an Obstetrician to provide their maternity care. About 78 percent choose a midwife (8 percent GP, 8 percent Obstetrician, 6 percent unknown. [8]). Midwives provide maternity care from early pregnancy to 6 weeks postpartum. The midwifery scope of practise covers normal pregnancy and birth. The midwife will either consult or transfer care where there is a departure from normal. Antenatal and postnatal care is normally provided in the woman’s home. Birth can be in the home, a primary birthing unit, or a hospital. Midwifery care is fully funded by the Government. (GP care is fully funded. Obstetric care will incur a fee in addition to the government funding.)
References
- ↑ Wagner, Marsden. Welcoming Baby, or Not: Are men, machines, and hospitals really necessary for a healthy childbirth? American Sexuality Magazine. Accessed 3-27-07.
- ↑ Gunnar Heinsohn/Otto Steiger: "Witchcraft, Population Catastrophe and Economic Crisis in Renaissance Europe: An Alternative Macroeconomic Explnanation.", University of Bremen 2004 (download); Gunnar Heinsohn/Otto Steiger: "The Elimination of Medieval Birth Control and the Witch Trials of Modern Times", International Journal of Women's Studies, 3, May 1982, 193-214; Gunnar Heinsohn/Otto Steiger: "Birth Control: The Political-Economic Rationale Behind Jean Bodin's "Démonomanie"", in: History of Political Economy, 31, No. 3, 423-448
- ↑ see John M. Riddle: "The Great Witch-Hunt and the Suppression of Birth Control: Heinsohn and Steiger's Theory from the Perspective of an Historian", Appendix to: Gunnar Heinsohn/Otto Steiger: "Witchcraft, Population Catastrophe and Economic Crisis in Renaissance Europe: An Alternative Macroeconomic Explanation.", University of Bremen 2004(download); also see John M. Riddle: Eve's Herbs: A History of Contraception and Abortion in the West, Princeton: Harvard University Press 1999, ISBN-10: 0674270266, esp. Chapters 5-7
- ↑ Midwife law lacks clarity (STLToday)
- ↑ Judge temporarily bars Missouri midwives law (Columbia Daily Tribune)
- ↑ Midwifery law illegal, judge says (Columbia Daily Tribune)
- ↑ Threat to Independent Midwifery (BBC News)
- ↑ New Zealand Health Information Service: "Report on Maternity - Maternal and Newborn Information 2003."
See also
- Childbirth
- Natural childbirth
- Doula
- Nurse midwife
- Pregnancy
- Obstetrics
- Traditional birth attendant
- Justine Siegemund
- MIDIRS Midwifery Digest
- International Confederation of Midwives
External links
Midwifery Organizations
International:
- MIDIRS (Midwives Information and Resource Service)
- International Confederation of Midwives
- International Alliance of Midwives
Australia:
Canada:
- Association of Ontario Midwives (Canada)
- College of Midwives of Ontario (Canada)
- Canadian Association of Midwives
New Zealand:
United Kingdom:
- MIDIRS (Midwives Information and Resource Service)
- Nursing Y Midwifery Council - overseers of UK midwifery, by mandate of Parliament
United States:
- American College of Nurse-Midwives
- Midwives Alliance of North America (MANA)
- Midwifery Education Accreditation Council
- National Association of Certified Professional Midwives
- The North American Registry of Midwives - Certification agency for direct-entry midwives.
Articles / Presentations
- Reclaiming Midwives: Backdrop to the Future Linda Janet Holmes speaks at the University of Wisconsin Health Sciences Learning Center
- MIDIRS (Midwives Information and Resource Service) is an educational charity. Our mission is: 'To be the leading international information resource relating to childbirth and infancy, disseminating this information as widely as possible to assist in the improvement of maternity care'.
- MidwifeInfo is an independent US site with articles about midwifery, becoming a midwife, pain relief, evidence-based midwifery practice, drugs, herbs and other information relevant to midwives and consumers.
- EFN.org - 'The role of social support in midwifery practice and research', Melinda Cook, BHS, Hunter Valley Midwives Association Journal, vol. 2, no. 6 (November, 1994).
- MidwiferyToday.com - 'Midwifery Today, the Heart and Science of Birth'Many articles and news stories related to birth and midwifery
- MyMidwife.org - '...everything you need to know about midwifery, pregnancy, and women's health', American College of Nurse-Midwives
- Rogue Midwifery: Birthing On The Sly An article on Modern Day Rogue Midwifery/Underground Birthing and Barter for Birth
- Home Birth Video & Story Home Birth by Midwife
- http://www.davis-floyd.com contains a number of articles by anthropologist Robbie Davis-Floyd about American and international midwifery, including "Intuition as Authoritative Knowledege in Midwifery and Home Birth," "The Ups, Downs, and Interlinkages of Nurse- and Direct-Entry Midwifery in the US," "Types of Midwifery Training: An Anthropological Interview," "Home Birth Emergencies in the US and Mexico: The Trouble with Transport," "La Partera Profesional: A New Kind of Midwife in Mexico," and "Mutual Accommodation or Biomedical Hegemony? Anthropological Perspectives on Global Issues in Midwifery."
- Birth Ecology Project the online journal publishes articles for and about midwives, midwifery care, and natural birth
zh-min-nan:Sán-pô ca:Infermeria obstètrico-ginecològica da:Jordemoder de:Hebamme eu:Emagin it:Ostetrica nl:Verloskunde no:Jordmor fi:Kätilö sv:Barnmorska th:หมอตำแย