Epirubicin hydrochloride
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]; Associate Editor(s)-in-Chief: Gloria Picoy [2]
WikiDoc MAKES NO GUARANTEE OF VALIDITY. WikiDoc is not a professional health care provider, nor is it a suitable replacement for a licensed healthcare provider. WikiDoc is intended to be an educational tool, not a tool for any form of healthcare delivery. The educational content on WikiDoc drug pages is based upon the FDA package insert, National Library of Medicine content and practice guidelines / consensus statements. WikiDoc does not promote the administration of any medication or device that is not consistent with its labeling. Please read our full disclaimer here.
Black Box Warning
|
WARNING: RISK OF TISSUE NECROSIS, CARDIAC TOXICITY, SECONDARY ACUTE MYELOGENOUS LEUKEMIA, AND MYELOSUPPRESSION
See full prescribing information for complete Boxed Warning.
* Severe local tissue necrosis will occur if there is extravasation during administration. epirubicin hydrochloride must not be given by the intramuscular or subcutaneous route.
|
Overview
Epirubicin hydrochloride is an anthracycline topoisomerase II inhibitor that is FDA approved for the treatment of primary breast cancer with evidence of axillary node tumor involvement. There is a Black Box Warning for this drug as shown here. Common adverse reactions include leukopenia, neutropenia, anemia, thrombocytopenia, amenorrhea, lethargy, mucositis, infection, conjunctivitis, alopecia, nausea, vomiting, diarrhea and rash.
Adult Indications and Dosage
FDA-Labeled Indications and Dosage (Adult)
- Epirubicin hydrochloride is indicated as a component of adjuvant therapy in patients with evidence of axillary node tumor involvement following resection of primary breast cancer.
- Dosage: 100 to 120 mg/m2 for 3 to 4 week cycles
Off-Label Use and Dosage (Adult)
Guideline-Supported Use
There is limited information regarding Off-Label Guideline-Supported Use of Epirubicin hydrochloride in adult patients.
Non–Guideline-Supported Use
- Carcinoma of bladder
- Carcinoma of esophagus
- Gastric cancer
- Hodgkin's disease
- Malignant tumor of nasopharynx
- Metastatic breast cancer
- Non-Hodgkin's lymphoma
- Non-small cell lung cancer
- Ovarian cancer
- Small cell carcinoma of lung
- Soft tissue sarcoma
Pediatric Indications and Dosage
FDA-Labeled Indications and Dosage (Pediatric)
Safety and efficacy have not been established in pediatric patients
Off-Label Use and Dosage (Pediatric)
Guideline-Supported Use
There is limited information regarding Off-Label Guideline-Supported Use of Epirubicin hydrochloride in pediatric patients.
Non–Guideline-Supported Use
There is limited information regarding Off-Label Non–Guideline-Supported Use of Epirubicin hydrochloride in pediatric patients.
Contraindications
Patients should not be treated with epirubicin hydrochloride Injection if they have any of the following conditions:
- Cardiomyopathy and/or heart failure, recent myocardial infarction or severe arrhythmias.
- Previous treatment with maximum cumulative dose of anthracyclines.
- Hypersensitivity to epirubicin hydrochloride, other anthracyclines, or anthracenediones
Warnings
|
WARNING: RISK OF TISSUE NECROSIS, CARDIAC TOXICITY, SECONDARY ACUTE MYELOGENOUS LEUKEMIA, AND MYELOSUPPRESSION
See full prescribing information for complete Boxed Warning.
* Severe local tissue necrosis will occur if there is extravasation during administration. epirubicin hydrochloride must not be given by the intramuscular or subcutaneous route.
|
Administer epirubicin hydrochloride Injection only under the supervision of qualified physicians experienced in the use of cytotoxic therapy. Before beginning treatment with epirubicin hydrochloride, patients should recover from acute toxicities (such as stomatitis, neutropenia, thrombocytopenia, and generalized infections) of prior cytotoxic treatment. Also, precede initial treatment with epirubicin hydrochloride by a careful baseline assessment of blood counts; serum levels of total bilirubin, AST, and creatinine; and cardiac function as measured by left ventricular ejection function (LVEF). Carefully monitor patients during treatment for possible clinical complications due to myelosuppression. Supportive care may be necessary for the treatment of severe neutropenia and severe infectious complications. Monitoring for potential cardiotoxicity is also important, especially with greater cumulative exposure to epirubicin hydrochloride.
Injection-Related Reactions
epirubicin hydrochloride Injection is administered by intravenous infusion. Venous sclerosis may result from an injection into a small vessel or from repeated injections into the same vein. Extravasation of epirubicin hydrochloride during the infusion may cause local pain, severe tissue lesions (vesication, severe cellulitis), and necrosis. Administer epirubicin hydrochloride slowly into the tubing of a freely running intravenous infusion. Patients receiving initial therapy at the recommended starting doses of 100–120 mg/m2 should generally have epirubicin hydrochloride infused over 15–20 minutes. For patients who require lower epirubicin hydrochloride starting doses due to organ dysfunction or who require modification of epirubicin hydrochloride doses during therapy, the epirubicin hydrochloride infusion time may be proportionally decreased, but should not be less than 3 minutes. If possible, avoid veins over joints or in extremities with compromised venous or lymphatic drainage. Immediately terminate infusion and restart in another vein if a burning or stinging sensation indicates perivenous infiltration. Perivenous infiltration may occur without causing pain. Facial flushing, as well as local erythematous streaking along the vein, may be indicative of excessively rapid administration. It may precede local phlebitis or thrombophlebitis. Give prophylactic antibiotic therapy to patients administered the 120-mg/m2 regimen of epirubicin hydrochloride as a component of combination chemotherapy.
Hematologic
epirubicin hydrochloride can suppress bone marrow function as manifested by leukopenia, thrombocytopenia and anemia, and myelosuppression is usually the dose-limiting toxicity. Patients should be monitored for myelosuppression during therapy.
Cardiac
Cardiotoxicity is a known risk of anthracycline treatment. Anthracycline-induced cardiac toxicity may be manifested by early (or acute) or late (delayed) events. Early cardiac toxicity of epirubicin hydrochloride consists mainly of sinus tachycardia and/or electrocardiogram (ECG) abnormalities such as non-specific ST-T wave changes, but tachyarrhythmias, including premature ventricular contractions and ventricular tachycardia, bradycardia, as well as atrioventricular and bundle-branch block have also been reported. These effects do not usually predict subsequent development of delayed cardiotoxicity, are rarely of clinical importance, and are generally not considered an indication for the suspension of epirubicin hydrochloride treatment. Delayed cardiac toxicity results from a characteristic cardiomyopathy that is manifested by reduced LVEF and/or signs and symptoms of congestive heart failure (CHF) such as tachycardia, dyspnea, pulmonary edema, dependent edema, hepatomegaly, ascites, pleural effusion, gallop rhythm. Life-threatening CHF is the most severe form of anthracycline-induced cardiomyopathy. This toxicity appears to be dependent on the cumulative dose of epirubicin hydrochloride and represents the cumulative dose-limiting toxicity of the drug. If it occurs, delayed cardiotoxicity usually develops late in the course of therapy with epirubicin hydrochloride or within 2 to 3 months after completion of treatment, but later events (several months to years after treatment termination) have been reported.
Given the risk of cardiomyopathy, exceed a cumulative dose of 900 mg/m2 epirubicin hydrochloride only with extreme caution. Risk factors [active or dormant cardiovascular disease, prior or concomitant radiotherapy to the mediastinal/pericardial area, previous therapy with other anthracyclines or anthracenediones, concomitant use of other drugs with the ability to suppress cardiac contractility or cardiotoxic drugs, especially those with long half-lives (e.g., trastuzumab)] may increase the risk of epirubicin hydrochloride cardiotoxicity. Although not formally tested, it is probable that the toxicity of epirubicin hydrochloride and other anthracyclines or anthracenediones is additive. Cardiac toxicity with epirubicin hydrochloride may occur at lower cumulative doses whether or not cardiac risk factors are present.
Although endomyocardial biopsy is recognized as the most sensitive diagnostic tool to detect anthracycline-induced cardiomyopathy, this invasive examination is not practically performed on a routine basis. ECG changes such as dysrhythmias, a reduction of the QRS voltage, or a prolongation beyond normal limits of the systolic time interval may be indicative of anthracycline-induced cardiomyopathy, but ECG is not a sensitive or specific method for following anthracycline-related cardiotoxicity. The risk of serious cardiac impairment may be decreased through regular monitoring of LVEF during the course of treatment with prompt discontinuation of epirubicin hydrochloride at the first sign of impaired function. The preferred method for repeated assessment of cardiac function is evaluation of LVEF measured by multi-gated radionuclide angiography (MUGA) or echocardiography (ECHO). A baseline cardiac evaluation with an ECG and a MUGA scan or an ECHO is recommended, especially in patients with risk factors for increased cardiac toxicity. Perform repeated MUGA or ECHO determinations of LVEF, particularly with higher, cumulative anthracycline doses. The technique used for assessment should be consistent through follow-up. In patients with risk factors, particularly prior anthracycline or anthracenedione use, the monitoring of cardiac function must be particularly strict and the risk-benefit of continuing treatment with epirubicin hydrochloride in patients with impaired cardiac function must be carefully evaluated.
Do not administer epirubicin hydrochloride in combination with other cardiotoxic agents unless the patient's cardiac function is closely monitored. Patients receiving epirubicin hydrochloride after stopping treatment with other cardiotoxic agents, especially those with long half-lives such as trastuzumab, may also be at an increased risk of developing cardiotoxicity.
Secondary Leukemia
The occurrence of secondary acute myelogenous leukemia, with or without a preleukemic phase, has been reported in patients treated with anthracyclines. Secondary leukemia is more common when such drugs are given in combination with DNA-damaging antineoplastic agents, when patients have been heavily pretreated with cytotoxic drugs, or when doses of the anthracyclines have been escalated. These leukemias can have a short 1- to 3-year latency period.
epirubicin hydrochloride is mutagenic, clastogenic, and carcinogenic in animals.
Hepatic
The major route of elimination of epirubicin is the hepatobiliary system. Evaluate serum total bilirubin and AST levels before and during treatment with epirubicin hydrochloride. Patients with elevated bilirubin or AST may experience slower clearance of drug with an increase in overall toxicity. Lower doses are recommended in these patients. Patients with severe hepatic impairment have not been evaluated; therefore, do not use epirubicin hydrochloride in this patient population.
Renal
Assess serum creatinine before and during therapy. Dosage adjustment is necessary in patients with serum creatinine >5 mg/dL. Patients undergoing dialysis have not been studied.
Tumor-Lysis Syndrome
As with other cytotoxic agents, epirubicin hydrochloride may induce hyperuricemia as a consequence of the extensive purine catabolism that accompanies drug-induced rapid lysis of highly chemosensitive neoplastic cells (tumor-lysis syndrome). Other metabolic abnormalities may also occur. While not generally a problem in patients with breast cancer, consider the potential for tumor-lysis syndrome in potentially susceptible patients and consider monitoring serum uric acid, potassium, calcium, phosphate, and creatinine immediately after initial chemotherapy administration. Hydration, urine alkalinization, and prophylaxis with allopurinol to prevent hyperuricemia may minimize potential complications of tumor-lysis syndrome.
Immunosuppressant Effects/Increased Susceptibility to Infections
Administration of live or live-attenuated vaccines in patients immunocompromised by chemotherapeutic agents including epirubicin, may result in serious or fatal infections. Avoid vaccination with a live vaccine in patients receiving epirubicin hydrochloride. Killed or inactivated vaccines may be administered; however, the response to such vaccines may be diminished.
Gastrointestinal
epirubicin hydrochloride is emetigenic. Antiemetics may reduce nausea and vomiting; prophylactic use of antiemetics should be considered before administration of epirubicin hydrochloride, particularly when given in conjunction with other emetigenic drugs.
Thrombophlebitis and Thromboembolic Phenomena
As with other cytotoxic agents, thrombophlebitis and thromboembolic phenomena, including pulmonary embolism (in some cases fatal) have been coincidentally reported with the use of epirubicin hydrochloride.
Coadministration with Cimetidine
Cimetidine increased the AUC of epirubicin by 50%. Stop Cimetidine treatment during treatment with epirubicin hydrochloride.
Pregnancy
epirubicin hydrochloride can cause fetal harm when administered to a pregnant woman. Epirubicin was embryolethal and teratogenic in rats and rabbits. There are no adequate and well-controlled studies of epirubicin hydrochloride in pregnant women. If this drug is used during pregnancy, or if the patient becomes pregnant while taking this drug, the patient should be apprised of the potential hazard to a fetus. Women of child-bearing potential should be advised to avoid becoming pregnant during treatment and should use effective contraceptive methods.
Male Fertility and Reproductive Outcomes
Males with female sexual partners of childbearing potential should use contraception during and after cessation of epirubicin hydrochloride therapy. epirubicin hydrochloride may damage testicular tissue and spermatozoa. Possible sperm DNA damage raises concerns about loss of fertility and genetic abnormalities in fetuses. The duration of this effect is uncertain.
Laboratory Testing
Assess blood counts, including absolute neutrophil counts, and liver function before and during each cycle of therapy with epirubicin hydrochloride. Perform repeated evaluations of LVEF during therapy.
Inflammation following Irradiation
As with other anthracyclines, administration of epirubicin hydrochloride after previous radiation therapy may induce an inflammatory recall reaction at the site of the irradiation.
Adverse Reactions
Clinical Trials Experience
Because clinical trials are conducted under widely varying conditions, adverse reactions rates observed in the clinical trials of a drug cannot be directly compared to rates in the clinical trials of another drug and may not reflect the rates observed in practice.
Integrated safety data are available from two studies (Studies MA-5 and GFEA-05) evaluating epirubicin hydrochloride-containing combination regimens in patients with early breast cancer. Of the 1260 patients treated in these studies, 620 patients received the higher-dose epirubicin hydrochloride regimen (FEC-100/CEF-120), 280 patients received the lower-dose epirubicin hydrochloride regimen (FEC-50), and 360 patients received CMF. Serotonin-specific antiemetic therapy and colony-stimulating factors were not used in these trials. Clinically relevant acute adverse events are summarized in Table 1.

Delayed Events
Table 2 describes the incidence of delayed adverse events in patients participating in the MA-5 and GFEA-05 trials.

Two cases of acute lymphoid leukemia (ALL) were also observed in patients receiving epirubicin hydrochloride. However, an association between anthracyclines such as epirubicin hydrochloride and ALL has not been clearly established.
Postmarketing Experience
The following adverse reactions have been identified during post-approval use of epirubicin hydrochloride. Because these reactions are reported voluntarily from a population of uncertain size, it is not always possible to reliably estimate their frequency or establish a causal relationship to drug exposure.
- Infections and infestations: sepsis, pneumonia
- Immune system disorders: anaphylaxis
- Metabolism and nutrition disorders: dehydration, hyperuricemia
- Vascular disorders: shock, haemorrhage, embolism arterial, thrombophlebitis, phlebitis
- Respiratory, thoracic and mediastinal disorders: pulmonary embolism
- Gastrointestinal disorders: erosions, ulcerations, pain or burning sensation, bleeding, hyperpigmentation of the oral mucosa
- Skin and subcutaneous tissue disorders: erythema, flushes, skin and nail hyperpigmentation, photosensitivity, hypersensitivity to irradiated skin (radiation-recall reaction), urticaria
- Renal and urinary disorders: red coloration of urine for 1 to 2 days after administration
- General disorders and administration site conditions: fever, chills
- Injury, poisoning and procedural complications: chemical cystitis (following intravesical administration)
Drug Interactions
Cardioactive Compounds
Do not administer epirubicin in combination with other cardiotoxic agents unless the patient's cardiac function is closely monitored. Patients receiving epirubicin after stopping treatment with other cardiotoxic agents, especially those with long half-lives such as trastuzumab, may also be at an increased risk of developing cardiotoxicity.
Concomitant use of epirubicin hydrochloride with other cardioactive compounds that could cause heart failure (e.g., calcium channel blockers), requires close monitoring of cardiac function throughout treatment.
Cimetidine
Cimetidine increases the exposure to epirubicin. Stop Cimetidine during treatment with epirubicin hydrochloride.
Other Cytotoxic Drugs
epirubicin hydrochloride used in combination with other cytotoxic drugs may show on-treatment additive toxicity, especially hematologic and gastrointestinal effects.
Paclitaxel
The administration of epirubicin immediately prior to or after paclitaxel increased the systemic exposure of epirubicin, epirubicinol and 7-deoxydoxorubicin aglycone.
Docetaxel
The administration of epirubicin immediately prior to or after docetaxel did not have an effect on the systemic exposure of epirubicin, but increased the systemic exposure of epirubicinol and 7-deoxydoxorubicin aglycone.
Radiation Therapy
There are few data regarding the coadministration of radiation therapy and epirubicin hydrochloride. In adjuvant trials of epirubicin hydrochloride-containing CEF-120 or FEC-100 chemotherapies, breast irradiation was delayed until after chemotherapy was completed. This practice resulted in no apparent increase in local breast cancer recurrence relative to published accounts in the literature. A small number of patients received epirubicin hydrochloride-based chemotherapy concomitantly with radiation therapy but had chemotherapy interrupted in order to avoid potential overlapping toxicities. It is likely that use of epirubicin hydrochloride with radiotherapy may sensitize tissues to the cytotoxic actions of irradiation. Administration of epirubicin hydrochloride after previous radiation therapy may induce an inflammatory recall reaction at the site of the irradiation.
Concomitant Therapies-Hepatic Function
Epirubicin is extensively metabolized by the liver. Changes in hepatic function induced by concomitant therapies may affect epirubicin metabolism, pharmacokinetics, therapeutic efficacy, and/or toxicity.
Drug/Laboratory Test Interactions
There are no known interactions between epirubicin hydrochloride and laboratory tests.
Use in Specific Populations
Pregnancy
Pregnancy Category (FDA): D Epirubicin hydrochloride can cause fetal harm when administered to a pregnant woman. Administration of 0.8 mg/kg/day intravenously of epirubicin to rats (about 0.04 times the maximum recommended single human dose on a body surface area basis) during Days 5 to 15 of gestation was embryotoxic (increased resorptions and post-implantation loss) and caused fetal growth retardation (decreased body weight), but was not teratogenic up to this dose. Administration of 2 mg/kg/day intravenously of epirubicin to rats (about 0.1 times the maximum recommended single human dose on a body surface area basis) on Days 9 and 10 of gestation was embryotoxic (increased late resorptions, post-implantation losses, and dead fetuses; and decreased live fetuses), retarded fetal growth (decreased body weight), and caused decreased placental weight. This dose was also teratogenic, causing numerous external (anal atresia, misshapen tail, abnormal genital tubercle), visceral (primarily gastrointestinal, urinary, and cardiovascular systems), and skeletal (deformed long bones and girdles, rib abnormalities, irregular spinal ossification) malformations. Administration of intravenous epirubicin to rabbits at doses up to 0.2 mg/kg/day (about 0.02 times the maximum recommended single human dose on a body surface area basis) during Days 6 to 18 of gestation was not embryotoxic or teratogenic, but a maternally toxic dose of 0.32 mg/kg/day increased abortions and delayed ossification. Administration of a maternally toxic intravenous dose of 1 mg/kg/day epirubicin to rabbits (about 0.1 times the maximum recommended single human dose on a body surface area basis) on Days 10 to 12 of gestation induced abortion, but no other signs of embryofetal toxicity or teratogenicity were observed. When doses up to 0.5 mg/kg/day epirubicin were administered to rat dams from Day 17 of gestation to Day 21 after delivery (about 0.025 times the maximum recommended single human dose on a body surface area basis), no permanent changes were observed in the development, functional activity, behavior, or reproductive performance of the offspring.
There are no adequate and well-controlled studies of epirubicin hydrochloride in pregnant women. Two pregnancies have been reported in women taking epirubicin. A 34-year-old woman, 28 weeks pregnant at her diagnosis of breast cancer, was treated with cyclophosphamide and epirubicin every 3 weeks for 3 cycles. She received the last dose at 34 weeks of pregnancy and delivered a healthy baby at 35 weeks. A second 34-year-old woman with breast cancer metastatic to the liver was randomized to FEC-50 but was removed from study because of pregnancy. She experienced a spontaneous abortion. If this drug is used during pregnancy, or if the patient becomes pregnant while taking this drug, the patient should be apprised of the potential hazard to the fetus. Women of childbearing potential should be advised to avoid becoming pregnant.
Pregnancy Category (AUS): D
There is no Australian Drug Evaluation Committee (ADEC) guidance on usage of Epirubicin hydrochloride in women who are pregnant.
Labor and Delivery
There is no FDA guidance on use of Epirubicin hydrochloride during labor and delivery.
Nursing Mothers
Epirubicin was excreted into the milk of rats treated with 0.50 mg/kg/day of epirubicin during peri- and postnatal periods. It is not known whether this drug is excreted in human milk. Because many drugs, including other anthracyclines, are excreted in human milk and because of the potential for serious adverse reactions in nursing infants from epirubicin hydrochloride, a decision should be made whether to discontinue nursing or to discontinue the drug, taking into account the importance of the drug to the mother.
Pediatric Use
Safety and effectiveness of epirubicin hydrochloride have not been established in pediatric patients. Pediatric patients may be at greater risk for anthracycline-induced acute manifestations of cardiotoxicity and for chronic CHF. The pharmacokinetics of epirubicin in pediatric patients have not been evaluated.
Geriatic Use
Although a lower starting dose of epirubicin hydrochloride was not used in trials in elderly female patients, particular care should be taken in monitoring toxicity when epirubicin hydrochloride is administered to female patients ≥ 70 years of age.
Gender
In patients ≤ 50 years of age, mean clearance values in adult male and female patients were similar. The clearance of epirubicin is decreased in elderly women.
Race
The influence of race on the pharmacokinetics of epirubicin has not been evaluated.
Renal Impairment
No significant alterations in the pharmacokinetics of epirubicin or its major metabolite, epirubicinol, have been observed in patients with serum creatinine < 5 mg/dL. Consider lower doses in patients with severe renal impairment (serum creatinine > 5 mg/dL), as a reduction in plasma clearance was reported in these patients. Patients on dialysis have not been studied.
Hepatic Impairment
Epirubicin is eliminated by both hepatic metabolism and biliary excretion and clearance is reduced in patients with hepatic dysfunction. Do not treat patients with severe hepatic impairment with epirubicin hydrochloride. Reduce the starting dose for patients with less severe hepatic impairment.
Females of Reproductive Potential and Males
In fertility studies in rats, males were given epirubicin daily for 9 weeks and mated with females that were given epirubicin daily for 2 weeks prior to mating and through Day 7 of gestation. When 0.3 mg/kg/day (about 0.015 times the maximum recommended human single dose on a body surface area basis) was administered to both sexes, no pregnancies resulted. No effects on mating behavior or fertility were observed at 0.1 mg/kg/day, but male rats had atrophy of the testes and epididymis, and reduced spermatogenesis. The 0.1 mg/kg/day dose also caused embryolethality. An increased incidence of fetal growth retardation was observed in these studies at 0.03 mg/kg/day (about 0.0015 times the maximum recommended human single dose on a body surface area basis). Multiple daily doses of epirubicin to rabbits and dogs also caused atrophy of male reproductive organs. Single 20.5 and 12 mg/kg doses of intravenous epirubicin caused testicular atrophy in mice and rats, respectively (both approximately 0.5 times the maximum recommended human dose on a body surface area basis). A single dose of 16.7 mg/kg epirubicin caused uterine atrophy in rats.
Immunocompromised Patients
There is no FDA guidance one the use of Epirubicin hydrochloride in patients who are immunocompromised.
Administration and Monitoring
Administration
Intravenous
Monitoring
There is limited information regarding Epirubicin hydrochloride Monitoring in the drug label.
IV Compatibility
There is limited information regarding the compatibility of Epirubicin hydrochloride and IV administrations.
Overdosage
There is no known antidote for overdoses of epirubicin hydrochloride. A 36-year-old man with non-Hodgkin's lymphoma received a daily 95 mg/m2 dose of epirubicin hydrochloride Injection for 5 consecutive days. Five days later, he developed bone marrow aplasia, grade 4 mucositis, and gastrointestinal bleeding. No signs of acute cardiac toxicity were observed. He was treated with antibiotics, colony-stimulating factors, and antifungal agents, and recovered completely. A 63-year-old woman with breast cancer and liver metastasis received a single 320 mg/m2 dose of epirubicin hydrochloride. She was hospitalized with hyperthermia and developed multiple organ failure (respiratory and renal), with lactic acidosis, increased lactate dehydrogenase, and anuria. Death occurred within 24 hours after administration of epirubicin hydrochloride. Additional instances of administration of doses higher than recommended have been reported at doses ranging from 150 to 250 mg/m2. The observed adverse events in these patients were qualitatively similar to known toxicities of epirubicin. Most of the patients recovered with appropriate supportive care.
If an overdose occurs, provide supportive treatment (including antibiotic therapy, blood and platelet transfusions, colony-stimulating factors, and intensive care as needed) until the recovery of toxicities. Delayed CHF has been observed months after anthracycline administration. Observe patients carefully over time for signs of CHF and provided with appropriate supportive therapy.
Pharmacology
Mechanism of Action
Epirubicin is an anthracycline cytotoxic agent. Although it is known that anthracyclines can interfere with a number of biochemical and biological functions within eukaryotic cells, the precise mechanisms of epirubicin's cytotoxic and/or antiproliferative properties have not been completely elucidated.
Epirubicin forms a complex with DNA by intercalation of its planar rings between nucleotide base pairs, with consequent inhibition of nucleic acid (DNA and RNA) and protein synthesis.
Such intercalation triggers DNA cleavage by topoisomerase II, resulting in cytocidal activity. Epirubicin also inhibits DNA helicase activity, preventing the enzymatic separation of double-stranded DNA and interfering with replication and transcription. Epirubicin is also involved in oxidation/reduction reactions by generating cytotoxic free radicals. The antiproliferative and cytotoxic activity of epirubicin is thought to result from these or other possible mechanisms.
Epirubicin is cytotoxic in vitro to a variety of established murine and human cell lines and primary cultures of human tumors. It is also active in vivo against a variety of murine tumors and human xenografts in athymic mice, including breast tumors.
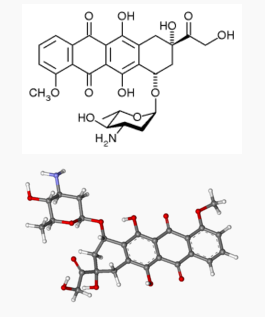
Structure
Empirical formula C27 H29 NO11 HCl and a molecular weight of 579.95. The structural formula is as follows:

Pharmacodynamics
There is limited information regarding Epirubicin hydrochloride Pharmacodynamics in the drug label.
Pharmacokinetics
Epirubicin pharmacokinetics are linear over the dose range of 60 to 150 mg/m2 and plasma clearance is not affected by the duration of infusion or administration schedule. Pharmacokinetic parameters for epirubicin following 6- to 10-minute, single-dose intravenous infusions of epirubicin hydrochloride at doses of 60 to 150 mg/m2 in patients with solid tumors are shown in Table 4. The plasma concentration declined in a triphasic manner with mean half-lives for the alpha, beta, and gamma phases of about 3 minutes, 2.5 hours, and 33 hours, respectively.

Distribution
Following intravenous administration, epirubicin is rapidly and widely distributed into the tissues. Binding of epirubicin to plasma proteins, predominantly albumin, is about 77% and is not affected by drug concentration. Epirubicin also appears to concentrate in red blood cells; whole blood concentrations are approximately twice those of plasma.
Metabolism
Epirubicin is extensively and rapidly metabolized by the liver and is also metabolized by other organs and cells, including red blood cells. Four main metabolic routes have been identified: (1) reduction of the C-13 keto-group with the formation of the 13(S)-dihydro derivative, epirubicinol; (2) conjugation of both the unchanged drug and epirubicinol with glucuronic acid; (3) loss of the amino sugar moiety through a hydrolytic process with the formation of the doxorubicin and doxorubicinol aglycones; and (4) loss of the amino sugar moiety through a redox process with the formation of the 7-deoxy-doxorubicin aglycone and 7-deoxy-doxorubicinol aglycone. Epirubicinol has in vitro cytotoxic activity one-tenth that of epirubicin. As plasma levels of epirubicinol are lower than those of the unchanged drug, they are unlikely to reach in vivo concentrations sufficient for cytotoxicity. No significant activity or toxicity has been reported for the other metabolites.
Excretion
Epirubicin and its major metabolites are eliminated through biliary excretion and, to a lesser extent, by urinary excretion. Mass-balance data from 1 patient found about 60% of the total radioactive dose in feces (34%) and urine (27%). These data are consistent with those from 3 patients with extrahepatic obstruction and percutaneous drainage, in whom approximately 35% and 20% of the administered dose were recovered as epirubicin or its major metabolites in bile and urine, respectively, in the 4 days after treatment.
Nonclinical Toxicology
Carcinogenesis
Conventional long-term animal studies to evaluate the carcinogenic potential of epirubicin have not been conducted, but intravenous administration of a single 3.6 mg/kg epirubicin dose to female rats (about 0.2 times the maximum recommended human dose on a body surface area basis) approximately doubled the incidence of mammary tumors (primarily fibroadenomas) observed at 1 year. Administration of 0.5 mg/kg epirubicin intravenously to rats (about 0.025 times the maximum recommended human dose on a body surface area basis) every 3 weeks for ten doses increased the incidence of subcutaneous fibromas in males over an 18-month observation period. In addition, subcutaneous administration of 0.75 or 1.0 mg/kg/day (about 0.015 times the maximum recommended human dose on a body surface area basis) to newborn rats for 4 days on both the first and tenth day after birth for a total of eight doses increased the incidence of animals with tumors compared to controls during a 24-month observation period.
Mutagenesis
Epirubicin was mutagenic in vitro to bacteria (Ames test) either in the presence or absence of metabolic activation and to mammalian cells (HGPRT assay in V79 Chinese hamster lung fibroblasts) in the absence but not in the presence of metabolic activation. Epirubicin was clastogenic in vitro (chromosome aberrations in human lymphocytes) both in the presence and absence of metabolic activation and was also clastogenic in vivo (chromosome aberration in mouse bone marrow).
Clinical Studies
Adjuvant Treatment of Breast Cancer
Two randomized, open-label, multicenter studies evaluated the use of epirubicin hydrochloride Injection 100 to 120 mg/m2 in combination with cyclophosphamide and fluorouracil for the adjuvant treatment of patients with axillary-node positive breast cancer and no evidence of distant metastatic disease (Stage II or III). Study MA-5 evaluated 120 mg/m2 of epirubicin hydrochloride per course in combination with cyclophosphamide and fluorouracil (CEF-120 regimen). This study randomized premenopausal and perimenopausal women with one or more positive lymph nodes to an epirubicin hydrochloride-containing CEF-120 regimen or to a CMF regimen. Study GFEA-05 evaluated the use of 100 mg/m2 of epirubicin hydrochloride per course in combination with fluorouracil and cyclophosphamide (FEC-100). This study randomized pre- and postmenopausal women to the FEC-100 regimen or to a lower-dose FEC-50 regimen. In the GFEA-05 study, eligible patients were either required to have ≥ 4 nodes involved with tumor or, if only 1 to 3 nodes were positive, to have negative estrogen- and progesterone-receptors and a histologic tumor grade of 2 or 3. A total of 1281 women participated in these studies. Patients with T4 tumors were not eligible for either study. Table 5 shows the treatment regimens that the patients received. Relapse-free survival was defined as time to occurrence of a local, regional, or distant recurrence, or disease-related death. Patients with contralateral breast cancer, second primary malignancy, or death from causes other than breast cancer were censored at the time of the last visit prior to these events.

In the MA-5 trial, the median age of the study population was 45 years. Approximately 60% of patients had 1 to 3 involved nodes and approximately 40% had ≥ 4 nodes involved with tumor. In the GFEA-05 study, the median age was 51 years and approximately half of the patients were postmenopausal. About 17% of the study population had 1 to 3 positive nodes and 80% of patients had ≥ 4 involved lymph nodes. Demographic and tumor characteristics were well-balanced between treatment arms in each study.
Relapse-free survival (RFS) and overall survival (OS) were analyzed using Kaplan-Meier methods in the intent-to-treat (ITT) patient populations in each study. Results were initially analyzed after up to 5 years of follow-up and these results are presented in the text below and in Table 6. Results after up to 10 years of follow-up are presented in Table 6. In Study MA-5, epirubicin hydrochloride-containing combination therapy (CEF-120) showed significantly longer RFS than CMF (5-year estimates were 62% versus 53%, stratified logrank for the overall RFS p=0.013). The estimated reduction in the risk of relapse was 24% at 5 years. The OS was also greater for the epirubicin hydrochloride-containing CEF-120 regimen than for the CMF regimen (5-year estimate 77% versus 70%; stratified logrank for overall survival p=0.043; non-stratified logrank p=0.13). The estimated reduction in the risk of death was 29% at 5 years.
In Study GFEA-05, patients treated with the higher-dose epirubicin hydrochloride regimen (FEC-100) had a significantly longer 5-year RFS (estimated 65% versus 52%, logrank for the overall RFS p=0.007) and OS (estimated 76% versus 65%, logrank for the overall survival p=0.007) than patients given the lower dose regimen (FEC-50). The estimated reduction in risk of relapse was 32% at 5 years. The estimated reduction in the risk of death was 31% at 5 years. Results of follow-up up to 10 years (median follow-up = 8.8 years and 8.3 years, respectively, for Study MA-5 and Study GFEA-05) are presented in Table 6.
Although the trials were not powered for subgroup analyses, in the MA-5 study, improvements in favor of CEF-120 vs. CMF were observed, in RFS and OS both in patients with 1–3 node positive and in those with ≥4 node positive tumor involvement. In the GFEA-05 study, improvements in RFS and OS were observed in both pre- and postmenopausal women treated with FEC-100 compared to FEC-50.

The Kaplan-Meier curves for RFS and OS from Study MA-5 are shown in Figures 3 and 4 and those for Study GFEA-05 are shown in Figures 5 and 6.

How Supplied
- Epirubicin hydrochloride 50 mg/25 mL single-use vial (NDC 0009-5091-01)
- Epirubicin hydrochloride 200 mg/100 mL single-use vial (NDC 0009-5093-01)
Storage
Store refrigerated between 2ºC and 8ºC (36ºF and 46ºF).
Images
Drug Images
{{#ask: Page Name::Epirubicin hydrochloride |?Pill Name |?Drug Name |?Pill Ingred |?Pill Imprint |?Pill Dosage |?Pill Color |?Pill Shape |?Pill Size (mm) |?Pill Scoring |?NDC |?Drug Author |format=template |template=DrugPageImages |mainlabel=- |sort=Pill Name }}
Package and Label Display Panel


{{#ask: Label Page::Epirubicin hydrochloride |?Label Name |format=template |template=DrugLabelImages |mainlabel=- |sort=Label Page }}
Patient Counseling Information
- Inform patients of the expected adverse effects of epirubicin hydrochloride, including gastrointestinal symptoms (nausea, vomiting, diarrhea, and stomatitis), alopecia and potential neutropenic complications.
- Patients should understand that there is a risk of irreversible myocardial damage associated with treatment with epirubicin hydrochloride, as well as a risk of treatment-related leukemia.
- Patients should consult their physician if vomiting, dehydration, fever, evidence of infection, symptoms of CHF, or injection-site pain occurs following therapy with epirubicin hydrochloride.
- Advise patients that their urine may appear red for 1 to 2 days after administration of epirubicin hydrochloride and that they should not be alarmed.
- Because epirubicin hydrochloride may induce chromosomal damage in sperm, advise men undergoing treatment with epirubicin hydrochloride to use effective contraceptive methods. Women treated with epirubicin hydrochloride may develop irreversible amenorrhea, or premature menopause.
Precautions with Alcohol
Alcohol-Epirubicin hydrochloride interaction has not been established. Talk to your doctor about the effects of taking alcohol with this medication.
Brand Names
- Ellence [1]
Look-Alike Drug Names
There is limited information regarding Epirubicin hydrochloride Look-Alike Drug Names in the drug label.
Price
References
The contents of this FDA label are provided by the National Library of Medicine.
{{#subobject:
|Label Page=Epirubicin hydrochloride |Label Name=Epirubicin hydrochloride 50 mg.png
}}
{{#subobject:
|Label Page=Epirubicin hydrochloride |Label Name=Epirubicin hydrochloride 200 mg.png
}}