Embryonal carcinoma pathophysiology
|
Embryonal carcinoma Microchapters |
|
Diagnosis |
|---|
|
Treatment |
|
Case Studies |
|
Embryonal carcinoma pathophysiology On the Web |
|
American Roentgen Ray Society Images of Embryonal carcinoma pathophysiology |
|
Risk calculators and risk factors for Embryonal carcinoma pathophysiology |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1];Associate Editor(s)-in-Chief: Shivali Marketkar, M.B.B.S. [2]
Pathophysiology
Gross Pathology

The gross examination usually shows a two to three centimetre pale grey, poorly defined tumour with associated haemorrhage and necrosis.[1]
Microscopic Pathology
The microscopic features include: indistinct cell borders, mitoses, a variable architecture (tubulopapillary, glandular, solid, embryoid bodies - ball of cells surrounded by empty space on three sides), nuclear overlap, and necrosis. An important key to distinguish it from other tumors, such as seminoma (vacuolated), teratocarcinoma (3 differentiated germ layers), yolk sac tumor (Schiller-Duval bodies), and the Sertoli-Leydig cell tumor (strings of glands), is that the embryonal carcinoma cells are "trying" to evolve into their next stage of development. So in the testicle, they are often observed as blue cells attempting to form primitive tubules.[2] Shown below is an image of embronal carcinoma(H&E stain).
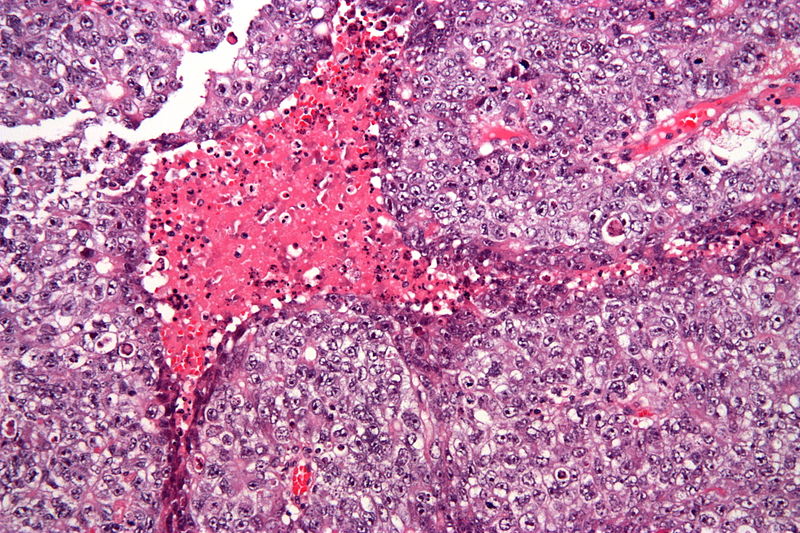
High magnification micrograph of an embryonal carcinoma, a type of germ cell tumour.
Main features:
- Nuclear atypia.
- Nucleoli prominent.
- Necrosis common.
- Nuclei overlap.
Other features:
- Variable architecture:
- Tubulopapillary.
- Glandular.
- Solid.
- Embryoid bodies - ball of cells in surrounded by empty space on three sides.
- Mitoses common.
Video
{{#ev:youtube|Ot3QjXcFim4}}
References
- ↑ Abbas, Fausto, Mitchell (2010). Basic Pathology. Elsevier. pp. 696–697. ISBN 978-81-312-1036-9.
- ↑ http://library.med.utah.edu/WebPath/MALEHTML/MALE092.html