Diastasis symphysis pubis
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]
Overview
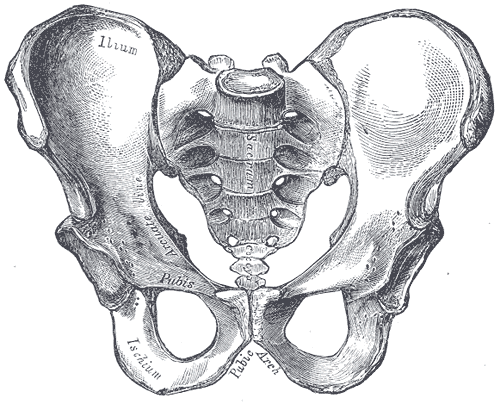
Diastasis symphysis pubis is the separation of normally joined pubic bones, as in the dislocation of the bones, without a fracture.
Diagnosis
This abnormally wide gap can be diagnosed by radiologic studies such as x-ray, MRI, CT scan or Bone scan. Manual testing by a Healthcare Professional can also be used. The patient is placed in various positions and pressure is applied in such a way that it provokes pain and maybe movement in the pubis.
X-ray
An x-ray film will show a marked gap between the pubic bones, normally there is a 4-5 mm gap but in pregnancy, hormonal influences cause relaxation of the connecting ligaments and the bones separate up to 9 mm. To demonstrate instability of the joint the patient is required to stand in the "flamingo" position, (standing with weight on one leg and the other bent)[1]. A vertical displacement of 1cm> is an indicator of symphysis pubis instability. [2]. Displacemnt 2cm> usually indicates involvement of the sacroiliac joints.
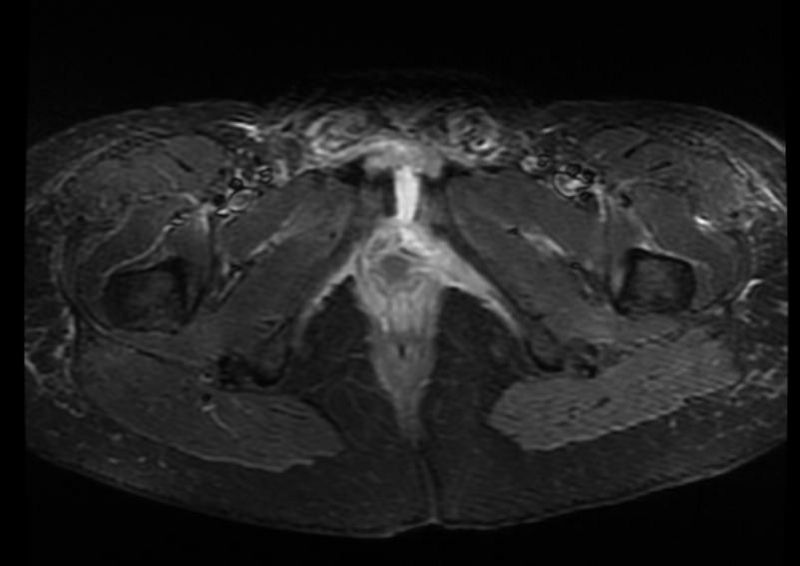
CT scan and MRI
Both diagnostic machines can produce detailed cross sections of the pelvic area. Images will show degrees soft tissue injury, inflammation of the subchondral region and the bone marrow [3] and any abnormal posturing of the pelvic joints.
Bone Scan
A bone scan is able to determine areas of bone inflammation.
Patient#1:Plain film and CT images demonstrate diastasis of the pubic symphysis
Patient #2: Plain film and MR images demonstrate diastasis of the pubic symphysis
External forces
External forces such as falling from a horse or a car accident can result in this type of injury to the symphysis pubis.
Pregnancy
The non-pregnant gap is 4-5mm but in pregnancy there will be an increase of at least 2-3mm due the ligaments which surround and insert into the joint as they remodel under the influence of hormones. Therefore, it is considered that a total width of up to 9mm between the two bones is normal for a pregnant woman. This natural extra gapping decreases within days following the delivery, although the supporting ligaments will take three to five months to fully return to their normal state. An abnormal gap is considered to be 1cm or more, sometimes with the two bones being slightly out of alignment. If there is a complete separation, that is, a traumatic tear, and the joint will be completely unstable. This tear can be felt and sometimes heard by the woman. There will be intensive pain followed by swelling and inflammation. The woman is unable to move her back, trunk, hips and legs without causing severe pain. When laying on her back her legs involuntary move apart and without the ability to close them together. This type of pelvic fracture needs to be treated as such and investigations into possible involvement of the sacroiliac joints should be addressed. It is important to note that the same can happen to the sacroiliac joints, and could lead to laxity and even inflammation. This involvement could involve one or both sacroiliac joint(s). A separation or diastasis can also be the result of traumatic forces from either an incident during the pregnancy or delivery. A diastasis of the symphysis pubis is a condition of Pelvic girdle pain.
References
- ↑ An Analysis of Pubis Symphysis Misalignment Using Plain Film Radiography Ruch WJ, Ruch BM. J Manipulative Physiol Ther. 2005;28(5):330-335
- ↑ Vertically Unstable Pelvic Fractures Fixed with Percutaneous Iliosacral Screws:Does Posterior Injury Predict Fixation Failure? Damian R. Griffin, MA, FRCS (Orth); Adam J. Starr, MD; Charles M. Reinert , MD; Alan L. Jones, MD; Shelly Whitlock, CCRA; University of Texas Southwestern Medical Center, Dallas, TX
- ↑ Magnetic resonance imaging changes of sacroiliac joints in patients with recent-onset inflammatory back pain: inter-reader reliability and prevalence of abnormalities. Arthritis Research & Therapy 2006, 8:R11 doi:10.1186/ar1859. Liesbeth Heuft-Dorenbosch1, René Weijers, Robert Landewé1, Sjef van der Linden1, Désirée van der Heijde1