Delayed puberty surgery
|
Delayed puberty Microchapters |
|
Diagnosis |
|---|
|
Treatment |
|
Case Studies |
|
Delayed puberty surgery On the Web |
|
American Roentgen Ray Society Images of Delayed puberty surgery |
|
Risk calculators and risk factors for Delayed puberty surgery |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]; Associate Editor(s)-in-Chief: Eiman Ghaffarpasand, M.D. [2]
Overview
The mainstay of treatment for delayed puberty is medical therapy. Surgery is usually reserved for patients with either pituitary tumors, hypothalamus hamartomas, and Turner syndrome. There are two procedures for excision of pituitary tumors, including endoscopic transsphenoidal surgery and craniotomy. In Turner syndrome with Y chromosome, the chance of becoming malignant is higher . Thus, oophorectomy (even salpingo-oophorectomy) has to be done urgently.
Surgery
The mainstay of treatment for delayed puberty is medical therapy. Surgery is usually reserved for patients with either:
Pituitary tumors
 |
| _fioC34LZeg}} |
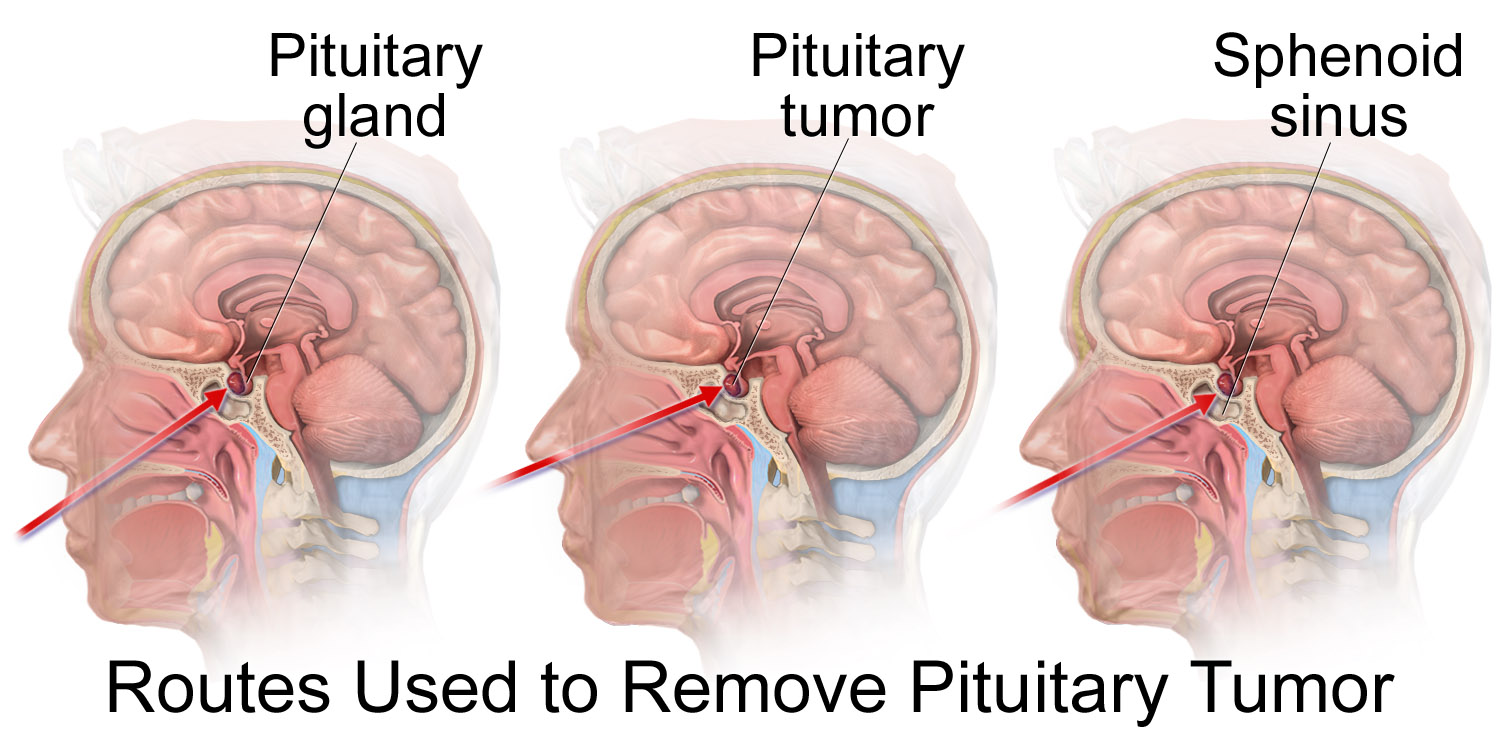
Endoscopic transsphenoidal surgery[2]
- In this method, the pituitary tumor is excised through nostrils by means of a tiny fiber-optic endoscopic tube.
- First bilateral nasal septal mucosa is incised in a C-shaped manner. The septal bone is approached through the incisions.
- Then, the sphenoidal rostrum and anterior wall of sphenoid sinus are gradually removed, a bone window is opened through the skull.
- After that, the dura mater is passed and the lesion becomes visualized.
- Finally, the tumor is removed using the curette and basket with suction.
- Advantages
- Disadvantages
- Not for large tumors
- Recurrent sinusitis in the future
- Low cure rate in case of suprasellar adhesion to adjunct tissues
Craniotomy[3]
- Although the preferred procedure to excise the pituitary tumors is a transsphenoidal approach, in some cases (1-4%) the size of the tumor or any suprasellar adhesion is indicative of a transcranial method.
- Some indications for transcranial method include:
- Isolation by a narrow waist at the diaphragma sellae
- Containment within the cavernous sinus lateral to the carotid artery
- Projection anteriorly onto the planum sphenoidal
- Projection laterally into the middle fossa
- Skull base surgical procedure is also an option for pituitary tumor treatment but may encounter the same problems that transsphenoidal method is faced with.
- Advantages
- Resection of large tumors
- Ability to excise the tumors with suprasellar specific conditions
- Disadvantage
- Long duration of post-operation recovery
- Harm to other parts of the brain
Turner syndrome
- Since the dysgenetic ovaries in Turner syndrome have a higher risk of malignancy, they have to be resected whenever the disease is diagnosed.
- In condition that patient with Turner syndrome has Y chromosome, the chance of becoming malignant is higher. Thus, oophorectomy (even salpingo-oophorectomy) has to be done urgently.[4]
References
- ↑ Own work, <"https://commons.wikimedia.org/w/index.php?curid=61131794"> Invalid parameter "puberty" in
<ref>tag. The supported parameters are: dir, follow, group, name. - ↑ Fan YP, Lv MH, Feng SY, Fan X, Hong HY, Wen WP; et al. (2014). "Full Endoscopic Transsphenoidal Surgery for Pituitary Adenoma-emphasized on Surgical Skill of Otolaryngologist". Indian J Otolaryngol Head Neck Surg. 66 (Suppl 1): 334–40. doi:10.1007/s12070-011-0317-4. PMC 3918297. PMID 24533411.
- ↑ Youssef AS, Agazzi S, van Loveren HR (2005). "Transcranial surgery for pituitary adenomas". Neurosurgery. 57 (1 Suppl): 168–75, discussion 168–75. PMID 15987585.
- ↑ Kanakatti Shankar R, Inge TH, Gutmark-Little I, Backeljauw PF (2014). "Oophorectomy versus salpingo-oophorectomy in Turner syndrome patients with Y-chromosome material: clinical experience and current practice patterns assessment". J. Pediatr. Surg. 49 (11): 1585–8. doi:10.1016/j.jpedsurg.2014.06.012. PMID 25475798.