Crown (dentistry)
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]
Overview
|
WikiDoc Resources for Crown (dentistry) |
|
Articles |
|---|
|
Most recent articles on Crown (dentistry) Most cited articles on Crown (dentistry) |
|
Media |
|
Powerpoint slides on Crown (dentistry) |
|
Evidence Based Medicine |
|
Cochrane Collaboration on Crown (dentistry) |
|
Clinical Trials |
|
Ongoing Trials on Crown (dentistry) at Clinical Trials.gov Trial results on Crown (dentistry) Clinical Trials on Crown (dentistry) at Google
|
|
Guidelines / Policies / Govt |
|
US National Guidelines Clearinghouse on Crown (dentistry) NICE Guidance on Crown (dentistry)
|
|
Books |
|
News |
|
Commentary |
|
Definitions |
|
Patient Resources / Community |
|
Patient resources on Crown (dentistry) Discussion groups on Crown (dentistry) Patient Handouts on Crown (dentistry) Directions to Hospitals Treating Crown (dentistry) Risk calculators and risk factors for Crown (dentistry)
|
|
Healthcare Provider Resources |
|
Causes & Risk Factors for Crown (dentistry) |
|
Continuing Medical Education (CME) |
|
International |
|
|
|
Business |
|
Experimental / Informatics |


Crown refers to the restoration of teeth using materials that are fabricated by indirect methods which are cemented into place. A crown is used to cap or completely cover a tooth.
Traditionally, the teeth to be crowned are prepared by a dentist and records are given to a dental technician to fabricate the crown or bridge, which can then be inserted at another dental appointment. The main advantages of the indirect method of tooth restoration include:
- fabrication of the restoration without the need for having the patient in the chair
- the utilization of materials that require special fabrication methods, such as casting
- the use of materials that require intense heat to be processed into a restoration, such as gold and porcelain.
The restorative materials used in indirect restorations possess superior mechanical properties than do the materials used for direct methods of tooth restoration, and thus produce a restoration of much higher quality.
As new technology and material chemistry has evolved, computers are increasingly becoming a part of crown and bridge fabrication, such as in CAD/CAM technology.
Why restore with a crown?
When decay is first detected in a tooth, the usual action taken by the dentist is to provide the tooth with an intracoronal restoration: a restoration consisting of a dental material that will exist totally within the confines of the remaining tooth structure. The restoration commonly referred to as a "cavity filling", or more colloquially as a "filling", is an intracoronal restoration, and can consist of a number of materials, including silver-colored amalgam, tooth-colored resin or gold. Inlays are also intracoronal restorations.
In a situation where there is not enough remaining solid tooth structure after decay and fragile tooth structure is removed, or the tooth has fractured and is now missing important architectural reinforcements, the tooth might very well require an extracoronal restoration: a restoration consisting of a dental material that will exist around the remaining tooth structure to a varying degree. Restorations that fall into this category include the various types of crowns and onlays, and these can consist of a number of materials as well, including gold, ceramic, or a combination of the two.
The circumstance of the damaged tooth defines the restoration. In other words, based upon factors such as remaining solid tooth structure, aesthetics, the location of the tooth within the dental arch and the consequent forces of function that said tooth will have to deal with once restored, the dentist will then decide on the proper way to treat the tooth.
Things are not always straightforward when it comes to restoring a tooth. An advantage of crowning a tooth over restoring the tooth with an excessively large pin-supported amalgam or composite restoration is that crowns provide much more protection against future fracture or recurrent decay. The indirect techniques of crown fabrication translate into a more adapted tooth-restoration margin, and thus a better seal against the decay-causing bacteria present in saliva.
Other reasons to restore with a crown
There are additional situations in which a crown would be the restoration of choice.
Implants
Dental implants are placed into either the maxilla or mandible as an alternative to partial or complete edentulism. Once placed and properly integrated into the bone, implants may then be fitted with a number of different prostheses:
- crowns or bridges
- precision attachments for either removable partial dentures, complete dentures or a hybrid sort of prosthetic appliance.
Endodontically treated teeth
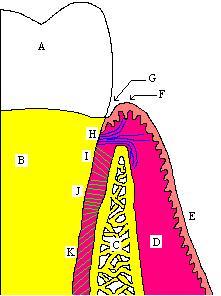
When teeth undergo endodontic treatment, or root canal therapy, they are devitalized when the nerve and blood supply are cut off and the space which they previously filled, known as the "pulp chamber" and "root canal", are thoroughly cleansed and filled with various materials to prevent future invasion by bacteria. Although there may very well be enough tooth structure remaining after root canal therapy is provided for a particular tooth to restore the tooth with an intracoronal restoration, this is not suggested in most teeth. The vitality of a tooth is remarkable in its ability to provide the tooth with the strength and durability it needs to function in mastication. The living tooth structure is surprisingly resilient and can sustain considerable abuse without fracturing. Consequently, after root canal therapy is performed, a tooth becomes extremely brittle and is significantly weaker than its vital neighbors.
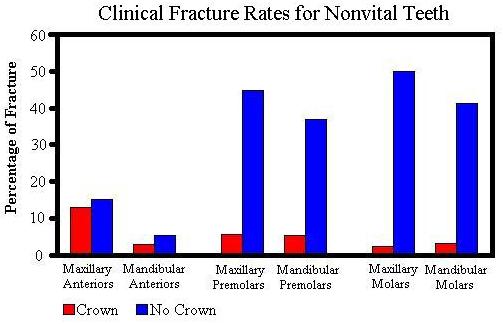
The average person can exert 150-200 lbs. of muscular force on their posterior teeth, which is approximately nine times the amount of force that can be exerted in the anterior. If the effective posterior contact area on a restoration is .1 mm², over 1 million PSI of stress is placed on the restoration. Therefore, posterior teeth (i.e. molars and premolars) should in almost all situations be crowned after undergoing root canal therapy to provide for proper protection against fracture (mandibular premolars, being very similar in crown morphology to canines, may in some cases be protected with intracoronal restorations). Should an endodontically treated tooth not be properly protected, there is a chance of it succumbing to breakage from normal functional forces. This fracture may well be difficult to treat, such as a "vertical root fracture" . Anterior teeth (i.e. incisors and canines), which are exposed to significantly lower functional forces, may effectively be treated with intracoronal restorations following root canal therapy if there is enough tooth structure remaining after the procedure.
Surveyed crown
Another situation in which a crown is the restoration of choice is when a tooth is intended as an abutment tooth for a removable partial denture, but is initially unfavorable for such a task. If the abutment teeth onto which the RPD is supposed to clasp do not possess the proper dimensions or features required, these aspects can be built into what is known as a surveyed crown.
Aesthetics
A fourth possible situation in which a crown would be the restoration of choice is when a patient desires to have his or her smile aesthetically improved but when partial coverage (i.e. a veneer/laminate) is not an option for one or more of a number of reasons. If the patient's occlusion does not permit for a mildly-retentive restoration, or if there is too much decay or a fracture within the tooth structure, a porcelain or composite veneer may not be placed with any adequate guarantee for its durability. Similarly, a bruxer (i.e. someone who grinds his or her teeth) may produce enough force to repeatedly dislodge or irreversibly abrade any veneer a dentist can plan for. In such a case, full coverage crowns can alter the size, shape or shade of a patient's teeth while protecting against failure of the restoration.
Makeover shows such as Extreme Makeover make extensive use of crowns, as the time-frame of the makeover period is too short to allow up to 18 months for orthodontic treatment to treat problems that might otherwise be corrected more conservatively.
Tooth preparation

Preparation of a tooth for a crown involves the irreversible removal of a significant amount of tooth structure. All restorations possess compromised structural and functional integrity when compared to healthy, natural tooth structure. Thus, if not indicated as desirable by an oral health-care professional, the crowning of a tooth would most likely be contraindicated. It should be evident, though, that dentists trained at different institutions in different eras and in different countries might very well possess different methods of treatment planning and case selection, resulting is somewhat diverse recommendations for treatment.
Traditionally more than one visit is required to complete crown and bridge work, and the additional time required for the procedure can be a disadvantage; the increased benefits of such a restoration, however, will generally offset these considerations.
Dimensions of preparation
When preparing a tooth for a crown, the enamel should be totally removed and the finished preparation should, thus, exist entirely in dentin. As elaborated on below, the amount of tooth structure required to be removed will depend on the material(s) being used to restore the tooth. If the tooth is to be restored with a full gold crown, the restoration need only be .5 mm in thickness (as gold is very strong), and therefore, a minimum of only .5 mm of space needs to be made for the crown to be placed. If porcelain is to be applied to the gold crown, an additional minimum of 1 mm of tooth structure needs to be removed to allow for a sufficient thickness of the porcelain to be applied, thus bringing the total tooth reduction to minimally 1.5 mm.
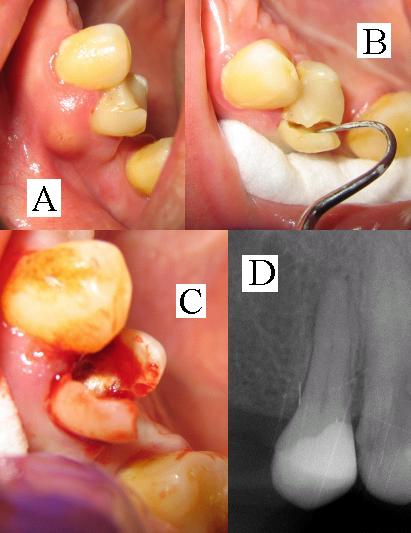
If there is not enough tooth structure to properly retain the prosthetic crown, the tooth requires a build-up material. This can be accomplished with a pin-retained direct restoration, such as amalgam or a resin like fluorocore, or in more severe cases, may require a post and core. Should the tooth require a post and core, endodontic therapy would then be indicated, as the post descends into the devitalized root canal for added retention. If the tooth, because of its relative lack of exposed tooth structure, also requires crown lengthening, the total combined time, effort and cost of the various procedures, together with the decreased prognosis because of the combined inherent failure rates of each procedure, might make it more reasonable to have the tooth extracted and opt to have an implant placed.
Taper
The prepared tooth also needs to possess a certain degree ie 3 to 5 degree of taper to allow for the restoration to be properly placed on the tooth. Fundamentally, there can be no undercuts on the surface of the prepared tooth, as the restoration will not be able to be removed from the die, let alone fit on the tooth (see explanation of lost-wax technique below for understanding of the processes involved in crown fabrication). At the same time, though, too much taper will severely limit the grip that the crown has while on the prepared tooth, thus contributing to failure of the restoration. Generally, 6º of taper around the entire circumference of the prepared tooth, giving a combined taper of 12º at any given sagittal section through the prepared tooth, is appropriate to both allow the crown to fit yet provide enough grip.
Margin

The most coronal position of untouched tooth structure (that is, the continual line of original, undrilled tooth structure at or near the gum line) is referred to as the margin. This margin will be the future continual line of tooth-to-restoration contact, and should be a smooth, well-defined delineation so that the restoration, no matter how it is fabricated, can be properly adapted and not allow for any openings visible to the naked eye, however slight. An acceptable distance from tooth margin to restoration margin is anywhere from 40-100 μm. However, the R.V. Tucker method of gold inlay and onlay restoration produces tooth-to-restoration adaptation of potentially only 2 μm, confirmed by scanning electron microscopy; this is less than the diameter of a single bacterium.
Naturally, the tooth-to-restoration margin is an unsightly thing to have exposed on the visible surface of a tooth when the tooth exists in the aesthetic zone of the smile. In these areas, the dentist would like to place the margin as far apical (towards the root tip of the tooth) as possible, even below the gum line. While there is no issue, per se, with placing the margin at the gumline, problems may arise when placing the margin too subgingivally (below the gumline). First, there might be issues in terms of capturing the margin in an impression to make the stone model of the prepared tooth (see stone model replication of tooth in photographs, above). Secondly, there is the seriously important issue of biologic width. Biologic width is the mandatory distance to be left between the height of the alveolar bone and the margin of the restoration, and if this distance is violated because the margin is placed too subgingivally, serious repercussions may follow. In situations where the margin cannot be placed apically enough to provide for proper retention of the prosthetic crown on the prepared tooth structure, the tooth or teeth involved should undergo a crown lengthening procedure.
There are a number of different types of margins that can be placed for restoration with a crown. There is the chamfer, which is popular with full gold restorations, which effectively removed the smallest amount of tooth structure. There is also a shoulder, which, while removing slightly more tooth structure, serves to allow for a thickness of the restoration material, necessary when applying porcelain to a PFM coping or when restoring with an all-ceramic crown (see below for elaboration on various types of crowns and their materials). When using a shoulder preparation, the dentist is urged to add a bevel; the shoulder-bevel margin serves to effectively decrease the tooth-to-restoration distance upon final cementation of the restoration.
Ferrule effect
The single most important consideration when restoring with a crown is, undeniably, the incorporation of the ferrule effect. As with the bristles of a broom, which are grasped by a ferrule when attached to the broomstick, the crown should envelop a certain height of tooth structure to properly protect the tooth from fracture after being prepared for a crown. This has been established through multiple experiments as a mandatory continuous circumferential height of 2 mm; any less provides for a significantly higher failure rate of endodontically-treated crown-restored teeth. When a tooth is not endodontically treated, the remaining tooth structure will invariably provide the 2 mm height necessary for a ferrule, but endodontically treated teeth are notoriously decayed and are often missing significant solid tooth structure. Because they are extremely brittle after being devitalized, endodontically treated teeth require proper protection against vertical root fracture. Contrary to what some dentists believe, a bevel is not at all suitable for implementing the ferrule effect, and beveled tooth structure may not be included in the 2 mms of required tooth structure for a ferrule. Some have speculated that a shoulder preparation on an all ceramic crown that will be bonded in place may have the same effect as a ferrule.
Adequate and appropriate restoration of tooth structure
Because crowns are fabricated in a laboratory or with CAD/CAM technology (computer-assisted design/computer-assisted manufacture), they can be made to a much higher level of precision and accuracy of things such as marginal adaptations than any direct restoration could ever potentially be made. And because crowns are considerably harder and stronger than any direct restoration could ever be (gold and/or porcelain vs. amalgam or plastic), they can be constructed to reproduce the original functional dimensions of the tooth they are restoring, including the cusp heights and slopes, whereas direct restorations are always too soft or weak, at least upon initial insertion, to properly produce these features without leading to failure of the restoration. Almost undoubtedly, a damaged tooth which really should have had a crown placed on it but which is instead restored with a direct restoration for one reason or another will fail, thus necessitating a crown at that point anyway, but now with an even poorer prognosis. In fact, sometimes an improperly restored tooth will fail beyond repair, and require extraction.
3/4 and 7/8 crowns
There are even restorations that fall between an onlay and a full crown when it comes to preservation of natural tooth structure. In the past, it was somewhat common to find dentists who prepared teeth for 3/4 and 7/8 crowns. Such restorations would generally be fabricated for maxillary second premolars or first molars, which might only be slightly visible when a patient smiled. Thusly, the dentist would preserve healthy natural tooth structure that existed on the mesiobuccal corner of the tooth for aesthetic purposes, the remainder of the tooth would be enclosed in restorative material. Even when porcelain-fused-to-metal and all-ceramic crowns were developed, preserving any amount of tooth structure adds to the overall strength of the tooth. As one can imagine, though, those dentists who took issue with the increased marginal length of the onlay restoration would surely take issue with the purported advantages of increased remaining tooth structure when it translated into the enormously increased marginal length of a 3/4 or 7/8 crown.
All-ceramic restorations
Inlays, onlays and all varieties of crowns can also be fabricated out of ceramic materials, such as in CAD/CAM technology. Although tooth-colored and thus perhaps more aesthetic than gold, and obtained with less time spent at the dentist's office (CAD/CAM technology allows for immediate, same day delivery of the restoration), ceramic restorations cannot be finished, polished or burnished at the margin as gold can, and thus possess a significantly lower level of marginal adaptation than does gold. Additionally, the mechanical properties of gold that make its restorations superior to that of amalgam or composite, including but not limited to the properties of stress, strain, fatigue, creep, compressive and tensile strengths, modulus of elasticity, biocompatibility, elastic and plastic deformation, resilience and toughness, also make it superior to the ceramics utilized in CAD/CAM technology as well as the other all-ceramic restorations that will be listed and elaborated on below. Superficially, all-ceramic restorations may appear to be more beneficial than gold, but long term benefits are certainly restricted to that of aesthetic concerns, which is a subjective issue that should be seriously weighed against the considerable benefits of gold.
Longevity
Although no dental restoration lasts forever, the average lifespan of a crown is around 10 years. While this is considered comparatively favorable to direct restorations, they can actually last up to the life of the patient (50 years or more) with proper care. One reason why a 10 year mark is given is because a dentist can usually provide patients with this number and be confident that a crown he or she makes will last at least this long. It should be noted that many dental plans in North America will allow for a crown to be replaced after only five years.
All who are familiar with dentistry will agree that the most important factor affecting the lifespan of any restorative is the continuing oral hygiene performed by the patient. Similar to almost anything, a poorly-made object can last way past its predicted lifetime if it is properly cared for, and even a well-made item can last only a day if handled improperly. Other factors depend on the skill of the dentist and his lab technician, the material used and appropriate treatment planning and case selection.
Full gold crowns last the longest, as they are fabricated as a single piece of gold. PFMs, or porcelain-fused-to-metal crowns possess an additional dimension in which they are prone to failure, as they incorporate brittle porcelain into their structure. Although incredibly strong in compression, porcelain is terribly fragile in tension, and fracture of the porcelain increased the risk of failure, which rises as the amount of surfaces covered with porcelain in increased. A traditional PFM with occlusal porcelain (i.e. porcelain applied to the biting surface of a posterior tooth) has a 7% higher chance of failure per year than a corresponding full gold crown.
When crowns are used to restore endodontically treated teeth, they increase the life of the tooth not only by preventing fracture of the brittle devitalized tooth but also by providing a better seal against invading bacteria. Although the inert filling material within the root canal blocks against microbial invasion of the internal tooth structure, it is actually a superior coronal seal, or marginal adaptation of the restoration in or on the crown of the tooth, which prevents reinvasion of the root canal.
Advantages and disadvantages
Whenever considering any irreversible process, especially in the field of surgery, one must conduct a thorough cost-benefit analysis.
The main disadvantages of restoration with a crown are extensive irreversible tooth preparation and higher costs than for direct restorations such as amalgam or Dental composite. The benefits, as described above, include long-term durability and evidence-based success as compared to other restorations or no treatment.
It is important to bear in mind that it is usually the damage to a tooth that dictates the need for a crown, and alternative treatments are usually less effective. However, it is also important to realise that even if risks and benefits are objectively analysed, their significance depends on the priorities of the patient. An example of this occurs when a patient would like to restore an edentulous area between healthy adjacent teeth. Before implants, there were three options:
- Fixed partial denture (bridge)
- Removable partial denture
- No treatment
Those who could afford it were usually told by their dentists that a bridge was their best choice, because it is much sturdier than removable dentures and requires less looking after. When implants became available, however, they were recommended as the best possible treatment, because the virgin teeth adjacent to the edentulous area no longer needed to be cut in order to fit the bridge. The affluent are thus told that a fixed partial denture is no longer desirable, now that implants are available.
Cost
Finally, crowns have a relatively much higher fee when compared to direct fillings. As mentioned above, the higher costs are associated with the additional chairtime and lab work that are required to fabricate a crown, in addition to the more expensive materials being used to do so. However, patients can expect increased longevity, strength and sometimes a more aesthetic result from a crown, and this should be factored in when weighing one's options.
The cost of a crown in the U.S. and Canada can range frasdc specialist is performing the procedure. However, dental care provided by students at U.S. and Canadian dental schools can often be obtained for as low as $300. Porcelain may cost about 20% more than full gold crowns, and the time-consuming processes of the operation is one reason for this high cost. Cost seems to be the limiting factor that precludes greater use of the procedure.
Types and materials
There are many different methods of crown fabrication, each using a different material. Some methods are quite similar, and utilize either very similar or identical materials.
Metal-containing restorations
Full gold crown
Full gold crowns (FGCs) consist entirely of a single piece of alloy. Although referred to as a gold crown, this type of crown is actually composed of many different types of elements, including but not limited to gold, platinum, palladium, silver, copper and tin. The first three elements listed are noble metals, while the last three listed are base metals. Full gold crowns are of better quality when they are high in noble content. According to the American Dental Association, full gold crown alloys can only be labeled as high noble when they contain at least 75% noble metal.
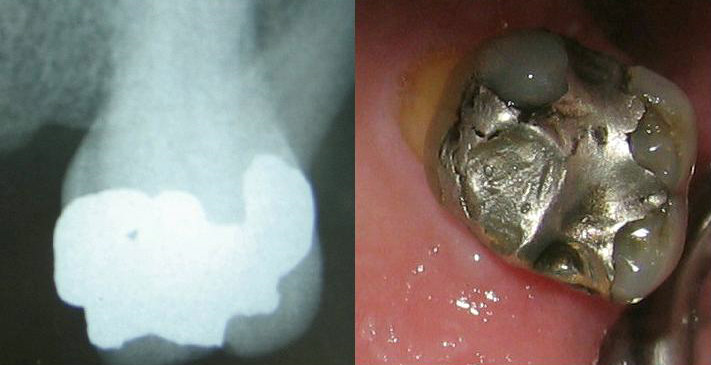
Full gold crowns are cast metal restorations that are made using the lost-wax technique. After the dentist prepares a tooth for a crown, he or she will take an impression of the prepared tooth, the adjacent teeth in the same arch and the opposing teeth in the opposing arch. With all of the necessary boundaries of the future cast crown defined in three dimensions within the impression material (i.e. the necessary height, width and depth of the crown is now recorded in impression material), the impression(s) are sent to a dental laboratory where they will be poured up in various types of dental stone or plaster. After the stone models are formed, they are ditched, died and articulated so that the laboratory technician can see how the two arches meet and properly access the tooth replicates to perform his tasks. (See photographs at the beginning of the article to see the stone model dies and the completed crown on the die.) The lab technician will then apply wax to the die (analog of the prepared tooth) and manipulate and craft the wax until he or she has built it up into what appears like and conforms to the specific dimensions of the tooth being restored. Prior to applying the wax, though, a die spacer is applied to the die. This is a thin coat of material that is painted onto the die to provide a space between the gold crown and the actual tooth structure to be filled with cement upon final cementation. A lubricant is also applied so that the wax pattern, as the wax-up of the crown is referred to, can be easily removed when completed.
The wax pattern, is removed from the die and invested in a sort of plaster while connected to a short plastic stick, called a "sprue former", which will stick out of the investing plaster. The investment, as it is called now, is placed in a furnace, which will completely burn off the wax and plastic that formed the wax pattern/sprue complex. What is left is a hollow within the investment material, known as an "investment pattern". Because the sprue former stuck out a little bit from the investment material, there is a communication between the outside and the investment pattern. The investment pattern is then placed in a sort of simple centrifuge where pennyweights of gold are melted down and rapidly shot through the communication in the investment pattern, through the sprue that was formed by the sprue former, and into the hollow that used to be inhabited by the wax pattern of the crown waxed-up by the technician, thus called the lost-wax technique. After properly cooling, the single piece crown-and-sprue of gold is sectioned, and the sprue can be recycled in another casting. The crown is touched-up in the location of the sprue attachment, finished and polished to a high shine, and delivered to the dentist so that he or she can try it in the mouth, make certain it has all of the proper contacts with the adjacent and opposing teeth, and cement it to the prepared tooth.
Porcelain-fused-to-metal crowns

Porcelain-fused-to-metal (PFM) crowns consist of a metal coping that is made with the same lost-wax technique used for a full gold crown, that then is primed for an application of feldspathic porcelain. The coping may conform to the proper dimensions of the restored tooth except for the facial surface of the tooth; it may be a thin shell on the prepared tooth designed to be covered entirely with porcelain; it may also be somewhere in the middle, such as cut back so as to provide space for porcelain only on the facial and occlusal surfaces of the crown.
The alloy used for PFMs is of a different variety for those used for FGCs. This is because the alloy for a PFM must be able to withstand the intense temperatures of the ceramic furnace necessary to properly bake the porcelain without deforming or slumping, which would alter the structural architecture of the metal coping, effectively ruining it.
Sometimes the dentist sees if the coping fits on the tooth prior to having the porcelain applied, while other times, the lab continues to complete the PFM and returns it to the dentist only after applying the porcelain. A coping try-in is more common in situations of multiple attached units or long-span bridges, where there might be a need to section the single-unit coping if the fit does not properly match the prepared teeth.
The strength afforded by cast metal restorations is a tremendous advantage. Whether the restoration is fabricated completely out of metal or has some porcelain affixed to it, the surfaces consisting entirely of metal can be as thin as 0.5 mm, which aids significantly in conservation of tooth structure. When porcelain is to added to the occlusal surfaces of posterior teeth or proximal surfaces of anterior teeth, at least 1 mm must be left for porcelain, in addition to the .5 mm for the coping thickness. The only reason to incorporate porcelain into a restoration is for aesthetics; its involvement otherwise serves only to undermine the strength and endurance of the crown.
Metal-free restorations
In-ceram
Introduced in 1989, In-ceram, by Vita, infused the fragile new "all-ceramic crown" with glass to produce what was then thought to be a superior product.
Procera
Procera AllCeram, owned by Nobel Biocare, is a CAD/CAM based method which produces a crown by overlaying a very durable ceramic coping of either alumina or zirconia, referred to as a "core", with Vitadur Alpha porcelain. Introduced in 1991, Procera can now be used to produce crowns, bridges and veneers.
Empress
The Empress system is superficially similar to a lost-wax technique in that a hollow investment pattern is made, but the similarities stop there. A specially designed pressure-injected leucite-reinforced ceramic is then pressed into the mold, as though the final all-ceramic restoration has been "cast." The Empress can be utilized for anything the lost-wax technique can be used for, in addition to veneers (which would not be made of cast metal).
CEREC
The current leader in CAD/CAM crown manufacturing in the U.S. and Canada is CEREC, by Sirona Dental. The CEREC method of fabricating all-ceramic restorations is by electronically capturing and storing a photographic image of the prepared tooth and, using computer technology, crafting a 3D restoration design that conforms to all the necessary specifications of the proposed inlay, onlay or single-unit crown; there is no impression. After selecting the proper features and making various decisions on the computerized model, the dentist directs the computer to send the information to a local milling machine. This machine will then use its specially designed diamond burs to mill the restoration from a solid ingot of a ceramic of pre-determined shade to match the patient's tooth. After about 20 minutes, the restoration is complete, and the dentist sections it from the remainder of the unmilled ingot and tries it in the mouth. If the restoration fits well, the dentist can cement the restoration immediately. A CEREC machine costs roughly $100,000, with continued purchase of ceramic ingots and milling burs.
Typically, over 95% of the restorations made using CEREC and Vita Mark I and Mark II blocks are still clinically successful after 5 years.[2] [3] Further, at least 90% of restorations still function successfully after 10 years.[2] [3] Advantages of the Mark II blocks over ceramic blocks include: they wear down as fast as natural teeth,[4] [3], their failure loads are very similar to those of natural teeth, [5] [3] and the wear pattern of Mark II against enamel is similar to that of enamel against enamel.[6] [7] [3]
References
- ↑ Torbjorner A, Karlsson S, Syverud M, Hensten-Petterson, A: Carbon fiber reinforced root canal posts. Mechanical and cytoxic properties, Eur J Oral Sci 104:605, 1996.
- ↑ 2.0 2.1 [Reiss, B., Walther, W. “Clinical long-term results and 10-year Kaplan-Meier analysis of CEREC Restorations” Int. Journal of Computerized Dentistry 2000 Sep; 3:8]
- ↑ 3.0 3.1 3.2 3.3 3.4 http://www.vident.com/assets/downloads_cloak/Bloc%20Talk%20Book.pdf
- ↑ [Abozenada, B, Pober, R, Giordano, R. “In-vitro wear of restorative dental materials” J. Dent. Res., Special Issue, VOL 81, MAR 2002, Abstract #1693]
- ↑ [Bremer BD, Geurtsen W.J “Molar fracture resistance after adhesive restoration with ceramic inlays or resin-based composites” Dent 2001 Aug;14(4):216-20]
- ↑ [Krejci, I., Wear of ceramic and other restorative materials. International Symposium on Computer Restorations. Quintessence, 245-251, 1991.]
- ↑ [Krejci, I. (German translation) Wear of enamel and amalgam and their enamel antagonists in a computer-simulated chewing simulation. Schweiz Monatsschr Zahnmed 100: 1285, 1990]
Additional Resources
- Herbert T. Shillingburg. FUNDAMENTALS OF FIXED PROSTHODONTICS, 1979.
- Fermin A. Carranza. CARRANZA'S CLINICAL PERIODONTOLOGY, 9th edition, 2002.
See also
External links
zh-min-nan:Khí-lông da:Krone og bro de:Zahnkrone it:Corona (odontoiatria) he:כתר (רפואת שיניים) hu:Korona (fogászat) nl:Kroon (tandheelkunde)