Copanlisib
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]; Associate Editor(s)-in-Chief: Sonya Gelfand, Anmol Pitliya, M.B.B.S. M.D.[2]
WikiDoc MAKES NO GUARANTEE OF VALIDITY. WikiDoc is not a professional health care provider, nor is it a suitable replacement for a licensed healthcare provider. WikiDoc is intended to be an educational tool, not a tool for any form of healthcare delivery. The educational content on WikiDoc drug pages is based upon the FDA package insert, National Library of Medicine content and practice guidelines / consensus statements. WikiDoc does not promote the administration of any medication or device that is not consistent with its labeling. Please read our full disclaimer here.
Overview
Copanlisib is a kinase inhibitor that is FDA approved for the treatment of adult patients with relapsed follicular lymphoma (FL) who have received at least two prior systemic therapies. Common adverse reactions include hyperglycemia, diarrhea, decreased general strength and energy, hypertension, leukopenia, neutropenia, nausea, lower respiratory tract infections, and thrombocytopenia.
Adult Indications and Dosage
FDA-Labeled Indications and Dosage (Adult)
Indications
- Copanlisib is indicated for the treatment of adult patients with relapsed follicular lymphoma (FL) who have received at least two prior systemic therapies.
- Accelerated approval was granted for this indication based on overall response rate. Continued approval for this indication may be contingent upon verification and description of clinical benefit in a confirmatory trial.
Recommended Dosage
- The recommended dose of Copanlisib is 60 mg administered as a 1-hour intravenous infusion on Days 1, 8, and 15 of a 28-day treatment cycle on an intermittent schedule (three weeks on and one week off). Continue treatment until disease progression or unacceptable toxicity
Dose Modification for Toxicities
- Manage toxicities per Table 1 with dose reduction, treatment delay, or discontinuation of Copanlisib. Discontinue Copanlisib if life-threatening Copanlisib-related toxicity occurs.

Off-Label Use and Dosage (Adult)
Guideline-Supported Use
There is limited information regarding Copanlisib Off-Label Guideline-Supported Use and Dosage (Adult) in the drug label.
Non–Guideline-Supported Use
There is limited information regarding Copanlisib Off-Label Non-Guideline-Supported Use and Dosage (Adult) in the drug label.
Pediatric Indications and Dosage
FDA-Labeled Indications and Dosage (Pediatric)
There is limited information regarding Copanlisib FDA-Labeled Indications and Dosage (Pediatric) in the drug label.
Off-Label Use and Dosage (Pediatric)
Guideline-Supported Use
There is limited information regarding Copanlisib Off-Label Guideline-Supported Use and Dosage (Pediatric) in the drug label.
Non–Guideline-Supported Use
There is limited information regarding Copanlisib Off-Label Non-Guideline-Supported Use and Dosage (Pediatric) in the drug label.
Contraindications
- None.
Warnings
Infections
- Serious, including fatal, infections occurred in 19% of 317 patients treated with Copanlisib monotherapy. The most common serious infection was pneumonia. Monitor patients for signs and symptoms of infection and withhold Copanlisib for Grade 3 and higher infection.
- Serious pneumocystis jiroveci pneumonia (PJP) infection occurred in 0.6% of 317 patients treated with Copanlisib monotherapy. Before initiating treatment with Copanlisib, consider PJP prophylaxis for populations at risk. Withhold Copanlisib in patients with suspected PJP infection of any grade. If confirmed, treat infection until resolution, then resume Copanlisib at previous dose with concomitant PJP prophylaxis.
Hyperglycemia
- Grade 3 or 4 hyperglycemia (blood glucose 250 mg/dL or greater) occurred in 41% of 317 patients treated with Copanlisib monotherapy. Serious hyperglycemic events occurred in 2.8% of patients. Treatment with Copanlisib may result in infusion-related hyperglycemia. Blood glucose levels typically peaked 5 to 8 hours post-infusion and subsequently declined to baseline levels for a majority of patients; blood glucose levels remained elevated in 17.7% of patients one day after Copanlisib infusion. Of 155 patients with baseline HbA1c <5.7%, 16 (10%) patients had HbA1c >6.5% at the end of treatment.
- Of the twenty patients with diabetes mellitus treated in CHRONOS-1, seven developed Grade 4 hyperglycemia and two discontinued treatment. Patients with diabetes mellitus should only be treated with Copanlisib following adequate glucose control and should be monitored closely.
- Achieve optimal blood glucose control before starting each Copanlisib infusion. Withhold, reduce dose, or discontinue Copanlisib depending on the severity and persistence of hyperglycemia.
Hypertension
- Grade 3 hypertension (systolic 160 mmHg or greater or diastolic 100 mmHg or greater) occurred in 26% of 317 patients treated with Copanlisib monotherapy. Serious hypertensive events occurred in 0.9% of 317 patients. Treatment with Copanlisib may result in infusion-related hypertension. The mean change of systolic and diastolic BP from baseline to 2 hours post-infusion on Cycle 1 Day 1 was 16.8 mmHg and 7.8 mmHg, respectively. The mean BP started decreasing approximately 2 hours post-infusion; BP remained elevated for 6 to 8 hours after the start of the Copanlisib infusion. Optimal BP control should be achieved before starting each Copanlisib infusion. Monitor BP pre- and post-infusion. Withhold, reduce dose, or discontinue Copanlisib depending on the severity and persistence of hypertension.
Non-Infectious Pneumonitis
- Non-infectious pneumonitis occurred in 5% of 317 patients treated with Copanlisib monotherapy. Withhold Copanlisib and conduct a diagnostic examination of a patient who is experiencing pulmonary symptoms such as cough, dyspnea, hypoxia, or interstitial infiltrates on radiologic exam. Patients with pneumonitis thought to be caused by Copanlisib have been managed by withholding Copanlisib and administration of systemic corticosteroids. Withhold, reduce dose, or discontinue Copanlisib depending on the severity and persistence of non-infectious pneumonitis.
Neutropenia
- Grade 3 or 4 neutropenia occurred in 24% of 317 patients treated with Copanlisib monotherapy. Serious neutropenic events occurred in 1.3%. Monitor blood counts at least weekly during treatment with Copanlisib. Withhold, reduce dose, or discontinue Copanlisib depending on the severity and persistence of neutropenia.
Severe Cutaneous Reactions
- Grade 3 and 4 cutaneous reactions occurred in 2.8% and 0.6% of 317 patients treated with Copanlisib monotherapy, respectively. Serious cutaneous reaction events were reported in 0.9%. The reported events included dermatitis exfoliative, exfoliative rash, pruritus, and rash (including maculo-papular rash). Withhold, reduce dose, or discontinue Copanlisib depending on the severity and persistence of severe cutaneous reactions.
Embryo-Fetal Toxicity
- Based on findings in animals and its mechanism of action, Copanlisib can cause fetal harm when administered to a pregnant woman. In animal reproduction studies, administration of Copanlisib to pregnant rats during organogenesis caused embryo-fetal death and fetal abnormalities in rats at maternal doses as low as 0.75 mg/kg/day (4.5 mg/m2/day body surface area) corresponding to approximately 12% the recommended dose for patients. Advise pregnant women of the potential risk to a fetus. Advise females of reproductive potential and males with female partners of reproductive potential to use effective contraception during treatment and for at least one month after the last dose.
Adverse Reactions
Clinical Trials Experience
- Because clinical trials are conducted under widely varying conditions, adverse reaction rates observed in the clinical trials of a drug cannot be directly compared to rates in the clinical trials of another drug and may not reflect the rates observed in the general patient population.
- The safety data reflect exposure to Copanlisib in 168 adults with follicular lymphoma and other hematologic malignancies treated with Copanlisib 60 mg or 0.8 mg/kg equivalent in clinical trials. The median duration of treatment was 22 weeks (range 1 to 206 weeks).
- Serious adverse reactions were reported in 44 (26%) patients. The most frequent serious adverse reactions that occurred were pneumonia (8%), pneumonitis (5%) and hyperglycemia (5%). The most common adverse reactions (≥20%) were hyperglycemia, diarrhea, decreased general strength and energy, hypertension, leukopenia, neutropenia, nausea, lower respiratory tract infections, and thrombocytopenia.
- Adverse reactions resulted in dose reduction in 36 (21%) and discontinuation in 27 (16%) patients. The most common reasons for dose reduction were hyperglycemia (7%), neutropenia (5%), and hypertension (5%). The most common reasons for drug discontinuation were pneumonitis (2%) and hyperglycemia (2%).
- Table 2 provides the adverse reactions occurring in at least 10% of patients receiving Copanlisib monotherapy, and Table 3 provides the treatment-emergent laboratory abnormalities in ≥20% of patients and ≥4% of Grade ≥3 treated with Copanlisib.


Postmarketing Experience
There is limited information regarding Copanlisib Postmarketing Experience in the drug label.
Drug Interactions
- Strong CYP3A Inducers
- Strong CYP3A Inhibitors
Strong CYP3A Inducers
- Avoid concomitant use of Copanlisib with strong CYP3A inducers. Concomitant use of Copanlisib with strong CYP3A inducers may decrease Copanlisib AUC and Cmax
- Examplesa of strong CYP3A inducers include: carbamazepine, enzalutamide, mitotane, phenytoin, rifampin, St. John’s wortb.
Strong CYP3A Inhibitors
- Concomitant use of Copanlisib with strong CYP3A inhibitors increases the Copanlisib AUC. If concomitant use with strong CYP3A inhibitors cannot be avoided, reduce the Copanlisib dose to 45 mg. An increase in the Copanlisib AUC may increase the risk of adverse reactions.
- Examplesa of strong CYP3A inhibitors include: boceprevir, clarithromycin, cobicistat, conivaptan, danoprevir and ritonavir, diltiazem, elvitegravir and ritonavir, grapefruit juicec, idelalisib, indinavir and ritonavir, itraconazole, ketoconazole, lopinavir and ritonavir, nefazodone, nelfinavir, paritaprevir and ritonavir and (ombitasvir and/or dasabuvir), posaconazole, ritonavir, saquinavir and ritonavir, tipranavir and ritonavir, troleandomycin, voriconazole.
- aThese examples are a guide and not considered a comprehensive list of all possible drugs that may fit this category. The healthcare provider should consult appropriate references for comprehensive information.
- bThe induction potency of St. John’s wort may vary widely based on preparation.
- cThe effect of grapefruit juice varies widely among brands and is concentration-, dose-, and preparation-dependent. Studies have shown that it can be classified as a “strong CYP3A inhibitor” when a certain preparation was used (e.g., high dose, double strength) or as a “moderate CYP3A inhibitor” when another preparation was used (e.g., low dose, single strength).
Use in Specific Populations
Pregnancy
Risk Summary
- Based on findings from animal studies and the mechanism of action, Copanlisib can cause fetal harm when administered to a pregnant woman.
- There are no available data in pregnant women to inform the drug-associated risk. In animal reproduction studies, administration of Copanlisib to pregnant rats during organogenesis resulted in embryo-fetal death and fetal abnormalities at maternal doses approximately 12% of the recommended dose for patients. Advise pregnant women of the potential risk to a fetus.
- Adverse outcomes in pregnancy occur regardless of the health of the mother or the use of medications. The background risk of major birth defects and miscarriage for the indicated population are unknown. In the U.S. general population, the estimated background risk of major birth defects and miscarriage in clinically recognized pregnancies is 2% to 4% and 15% to 20%, respectively.
Data (Animal)
- In an embryo-fetal development study in rats, pregnant animals received intravenous doses of Copanlisib of 0, 0.75, or 3 mg/kg/day during the period of organogenesis. Administration of Copanlisib at the dose of 3 mg/kg/day resulted in maternal toxicity and no live fetuses. Copanlisib administration at the dose of 0.75 mg/kg/day was maternally toxic and resulted in embryo-fetal death (increased resorptions, increased post-implantation loss, and decreased numbers of fetuses/dam). The dose of 0.75 mg/kg/day also resulted in increased incidence of fetal gross external (domed head, malformed eyeballs or eyeholes), soft tissue (hydrocephalus internus, ventricular septal defects, major vessel malformations), and skeletal (dysplastic forelimb bones, malformed ribs and vertebrae, and pelvis shift) abnormalities. The dose of 0.75 mg/kg/day (4.5 mg/m2 body surface area) in rats is approximately 12% of the recommended dose for patients.
- Following administration of radiolabeled Copanlisib to pregnant rats approximately 1.5% of the radioactivity (Copanlisib and metabolites) reached the fetal compartment.
Pregnancy Category (AUS):
There is no Australian Drug Evaluation Committee (ADEC) guidance on usage of Copanlisib in women who are pregnant.
Labor and Delivery
There is no FDA guidance on use of Copanlisib during labor and delivery.
Nursing Mothers
Risk Summary
- There are no data on the presence of Copanlisib and/or metabolites in human milk, the effects on the breastfed child, or on milk production. Following administration of radiolabeled Copanlisib to lactating rats, approximately 2% of the radioactivity was secreted into milk; the milk to plasma ratio of radioactivity was 25-fold. Because of the potential for serious adverse reactions in a breastfed child from Copanlisib, advise a lactating woman not to breastfeed during treatment with Copanlisib and for at least 1 month after the last dose.
Pediatric Use
- Safety and effectiveness have not been established in pediatric patients.
Geriatic Use
- No dose adjustment is necessary in patients ≥65 years of age. Of 168 patients with follicular lymphoma and other hematologic malignancies treated with Copanlisib, 48% were age 65 or older while 16% were age 75 or older. No clinically relevant differences in efficacy were observed between elderly and younger patients. In patients ≥65 years of age, 30% experienced serious adverse reactions and 21% experienced adverse reactions leading to discontinuation. In the patients <65 years of age, 23% experienced serious adverse reactions and 11% experienced adverse reactions leading to discontinuation.
Gender
There is no FDA guidance on the use of Copanlisib with respect to specific gender populations.
Race
There is no FDA guidance on the use of Copanlisib with respect to specific racial populations.
Renal Impairment
There is no FDA guidance on the use of Copanlisib in patients with renal impairment.
Hepatic Impairment
There is no FDA guidance on the use of Copanlisib in patients with hepatic impairment.
Females of Reproductive Potential and Males
Pregnancy Testing
- Copanlisib can cause fetal harm when administered to a pregnant woman. Conduct pregnancy testing prior to initiation of Copanlisib treatment.
Contraception
Females
- Advise female patients of reproductive potential to use highly effective contraception (contraception with a failure rate <1% per year) during treatment with Copanlisib and for at least one month after the last dose.
Males
- Advise male patients with female partners of reproductive potential to use highly effective contraception during treatment with Copanlisib and for at least one month after the last dose.
Infertility
- There are no data on the effect of Copanlisib on human fertility. Due to the mechanism of action of Copanlisib, and findings in animal studies, adverse effects on reproduction, including fertility, are expected.
Immunocompromised Patients
There is no FDA guidance one the use of Copanlisib in patients who are immunocompromised.
Administration and Monitoring
Administration
Preparation and Administration
- For intravenous infusion only.
- Administer Copanlisib as a single agent, following reconstitution and dilution. Mix only with 0.9% sodium chloride (NaCl) solution. Do not mix or inject Copanlisib with other drugs or other diluents.
Reconstitution Instructions
- Reconstitute Copanlisib with 4.4 mL of sterile 0.9% NaCl solution leading to a concentration of 15 mg/mL.
- Withdraw 4.4 mL of sterile 0.9% NaCl solution by using a 5 mL sterile syringe with needle.
- Inject the measured volume through the disinfected stopper surface into the vial of ALIQOPA.
- Dissolve the lyophilized solid by gently shaking the injection vial for 30 seconds.
- Allow to stand for one minute to let bubbles rise to the surface.
- Check if any undissolved substance is still seen. If yes, repeat the gentle shaking and settling procedure.
- Inspect visually for discoloration and particulate matter. After reconstitution, the solution should be colorless to slightly yellowish.
- Once the solution is free of visible particles, withdraw the reconstituted solution for further dilution.
Dilution Instructions for Intravenous Use
- Further dilute the reconstituted solution in 100 mL sterile 0.9% NaCl solution for injection. With a sterile syringe, withdraw the required amount of the reconstituted solution for the desired dosage:
- 60 mg: Withdraw 4 mL of the reconstituted solution with a sterile syringe.
- 45 mg: Withdraw 3 mL of the reconstituted solution with a sterile syringe.
- 30 mg: Withdraw 2 mL of the reconstituted solution with a sterile syringe.
- Inject the contents of the syringe into the patient infusion bag of 100 mL sterile 0.9% NaCl solution. Mix the dose well by inverting.
- Discard any unused reconstituted or diluted solution appropriately.
- Use reconstituted and diluted Copanlisib immediately or store the reconstituted solution in the vial or diluted solution in the infusion bag at 2°C to 8°C (36°F to 46°F) for up to 24 hours before use. Allow the product to adapt to room temperature before use following refrigeration. Avoid exposure of the diluted solution to direct sunlight.
Monitoring
- Evidence of disease response or stabilization is indicative of efficacy
- CBC: Including absolute neutrophil count, at least weekly during treatment
- Blood pressure (BP): Pre- and post-infusion; in clinical trials BP remained elevated for 6 to 8 hours after the start of the infusion and started decreasing approximately 2 hours post-infusion
- Glucose control: Closely in patients with diabetes mellitus
- Signs or symptoms of infection
IV Compatibility
There is limited information regarding the compatibility of Copanlisib and IV administrations.
Overdosage
There is limited information regarding Copanlisib overdosage. If you suspect drug poisoning or overdose, please contact the National Poison Help hotline (1-800-222-1222) immediately.
Pharmacology
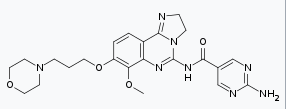
Mechanism of Action
- Copanlisib is an inhibitor of phosphatidylinositol-3-kinase (PI3K) with inhibitory activity predominantly against PI3K-α and PI3K-δ isoforms expressed in malignant B cells. Copanlisib has been shown to induce tumor cell death by apoptosis and inhibition of proliferation of primary malignant B cell lines. Copanlisib inhibits several key cell-signaling pathways, including B-cell receptor (BCR) signaling, CXCR12 mediated chemotaxis of malignant B cells, and NFκB signaling in lymphoma cell lines.
Structure

Pharmacodynamics
- At 60 mg (or 0.8 mg/kg) of Copanlisib dose, the elevation of plasma glucose was associated with higher Copanlisib exposure.
Pharmacokinetics
- The area under the plasma concentration-time curve (AUC) and maximum plasma concentration (Cmax) of Copanlisib increase dose-proportionally over 5 to 93 mg (0.08 to 1.55 times the approved recommended dose) absolute dose range and exhibit linear pharmacokinetics. There is no time-dependency and no accumulation in the pharmacokinetics of Copanlisib.
- The geometric mean (range) steady state Copanlisib exposure at 0.8 mg/kg (approximately the approved recommended dose of 60 mg) are 463 (range: 105 to 1670; SD: 584) ng/mL for Cmax and 1570 (range: 536 to 3410; SD: 338) ng.hr/mL for AUC0-25h.
Distribution
- The in vitro human plasma protein binding of Copanlisib is 84.2%. Albumin is the main binding protein. The in vitro mean blood-to-plasma ratio is 1.7 (range: 1.5 to 2.1). The geometric mean volume of distribution is 871 (range: 423 to 2150; SD: 479) L.
Elimination
- The geometric mean terminal elimination half-life of Copanlisib is 39.1 (range: 14.6 to 82.4; SD: 15.0) hours. The geometric mean clearance is 17.9 (range: 7.3 to 51.4; SD: 8.5) L/hr.
Metabolism
- Approximately >90% of Copanlisib metabolism is mediated by CYP3A and <10% by CYP1A1. The M-1 metabolite accounts for 5% of total radioactivity AUC and its pharmacological activity is comparable to the parent compound Copanlisib for the tested kinases PI3KandPI3K.
Excretion
- Copanlisib is excreted approximately 50% as unchanged compound and 50% as metabolites in humans. Following a single intravenous dose of 12 mg (0.2 times the recommended approved dose) radiolabeled Copanlisib, approximately 64% of the administered dose was recovered in feces and 22% in urine within 20 to 34 days. Unchanged Copanlisib represented approximately 30% of the administered dose in feces and 15% in urine. Metabolites resulting from CYP450-mediated oxidation metabolism accounted for 41% of the administered dose.
Specific Populations
- Copanlisib pharmacokinetic differences in the subpopulations listed below are assessed using population pharmacokinetic analyses.
- Age (20 to 90 years), gender, race (White, Asian, Hispanic, and Black), smoking status, body weight (41 to 130 kg), mild hepatic impairment [total bilirubin (TB) ≤ upper limit of normal (ULN) and aspartate aminotransferase (AST) > ULN, or TB < 1-1.5 x ULN and any AST], and mild to moderate renal impairment [CLcr ≥ 30 mL/min as estimated by Cockcroft-Gault (C-G) equation] had no clinically significant effect on the pharmacokinetics of Copanlisib. The pharmacokinetics of Copanlisib in patients with moderate to severe hepatic impairment (TB ≥ 1.5 x ULN, any AST), severe renal impairment (CLcr = 15-29 mL/min by C-G equation), or end stage renal disease (CLcr < 15 mL/min by C-G equation) with or without dialysis is unknown.
Drug Interaction Studies
Clinical Studies
Effect of CYP3A and P-gp Inducers on Copanlisib
- Rifampin, a strong CYP3A and a P-glycoprotein (P-gp) transporter inducer, administered at a dose of 600 mg once daily for 12 days with a single intravenous dose of 60 mg Copanlisib in patients with cancer resulted in a 63% decrease in the mean AUC and a 15% decrease in Cmax of Copanlisib.
Effect of CYP3A, P-gp and BCRP Inhibitors on Copanlisib
- Itraconazole, a strong CYP3A inhibitor and a P-gp and Breast Cancer Resistance Protein (BCRP) transporter inhibitor, administered at a dose of 200 mg once daily for 10 days increased the mean AUC of a single intravenous dose of 60 mg Copanlisib by 53% (or 1.53-fold) with no effect on Cmax (1.03-fold) in patients with cancer.
In Vitro Studies
Effect of Transporters on Copanlisib:
- Copanlisib is a substrate of P-gp and BCRP, but not a substrate for organic cation transporter (OCT) 1, OCT2, and OCT3, organic anion transporter (OAT) 1 and OAT3, organic anion-transporting polypeptide (OATP) 1B1 and OATP1B3, multidrug and toxin extrusion protein 1(MATE1) or MATE2-K.
Effect of Copanlisib on CYP and non-CYP Enzymes
- Copanlisib is not an inhibitor of the metabolism of drugs that are substrates of the major CYP isoforms (CYP1A2, 2A6, 2B6, 2C8, 2C9, 2C19, 2D6, 2E1, and 3A4) or uridine diphosphate-glucuronosyltransferase isoforms (UGT) or dihydropyrimidine dehydrogenase (DPD) at therapeutic 60 mg dose plasma concentrations. Copanlisib is not an inducer of CYP1A2, CYP2B6 and CYP3A.
Effect of Copanlisib on Drug Transporter Substrates
- Copanlisib is not an inhibitor of P-gp, BCRP, multi-drug resistance-associated protein (MRP2), bile salt export pump (BSEP), OATP1B1, OATP1B3, OAT1, OAT3, OCT1, OCT2, and MATE1 at therapeutic 60 mg dose plasma concentrations.
- Copanlisib is an inhibitor of MATE2-K (IC50: 0.09 μM). Based on the PK of Copanlisib,inhibition may occur after Copanlisib infusion at approved recommended dosage. The clinical significance of this potential inhibition on plasma concentrations of concomitantly administered drugs that are MATE2-K substrates is unknown.
Nonclinical Toxicology
Carcinogenesis, Mutagenesis, Impairment of Fertility
- Carcinogenicity studies have not been conducted with Copanlisib.
- Copanlisib did not cause genetic damage in in vitro or in vivo assays.
- Fertility studies with Copanlisib were not conducted; however, adverse findings in male and female reproductive systems were observed in the repeat dose toxicity studies. Findings in the male rats and/or dogs included effects on the testes (germinal epithelial degeneration, decreased weight, and/or tubular atrophy), epididymides (spermatic debris, decreased weight, and/or oligospermia/aspermia), and prostate (reduced secretion and/or decreased weight). Findings in female rats included effects on ovaries (hemorrhage, hemorrhagic cysts, and decreased weight), uterus (atrophy, decreased weight), vagina (mononuclear infiltration), and a dose-related reduction in the numbers of female rats in estrus.
Clinical Studies
Relapsed Follicular Lymphoma
- The efficacy of Copanlisib was evaluated in a single-arm, multicenter, phase 2 clinical trial (NCT 01660451) CHRONOS-1 in a total of 142 subjects, which included 104 subjects with follicular B-cell non-Hodgkin lymphoma who had relapsed disease following at least two prior treatments. Patients must have received rituximab and an alkylating agent. Baseline patient characteristics are summarized in Table 4. The most common prior systemic therapies were chemotherapy in combination with anti-CD20 immunotherapy (89%), chemotherapy alone (41%), and anti-CD20 immunotherapy alone (37%). In CHRONOS-1, 34% of patients received two prior lines of therapy and 36% received three prior lines of therapy.

- Refractory: No response or progression of disease within six months of last treatment.
- One hundred forty-two patients received 60 mg Copanlisib; 130 patients received fixed dose 60 mg Copanlisib and 12 patients received 0.8 mg/kg equivalent Copanlisib administered as a 1-hour intravenous infusion on Days 1, 8, and 15 of a 28-day treatment cycle on an intermittent schedule (three weeks on and one week off). Treatment continued until disease progression or unacceptable toxicity. Tumor response was assessed according to the International Working Group response criteria for malignant lymphoma. Efficacy based on overall response rate (ORR) was assessed by an Independent Review Committee. Efficacy results from CHRONOS-1 are summarized in Table 5.

How Supplied
- Copanlisib is contained in a colorless glass vial closed with bromobutyl stopper with a flanged closure. Each vial of Copanlisib contains Copanlisib as a lyophilized solid.

Storage
Product as packaged for sale
- Copanlisib vials must be refrigerated at 2°C to 8°C (36°F to 46°F).
Product after reconstitution
- Administer reconstituted and diluted solution immediately. If not, refrigerate at 2°C to 8°C (36°F to 46°F) and use within 24 hours. After refrigeration, allow the product to adapt to room temperature before use. Avoid exposure of the diluted solution to direct sunlight.
- Mix only with 0.9% NaCl solution. Do not mix or inject Copanlisib with other drugs or other diluents.
Images
Drug Images
{{#ask: Page Name::Copanlisib |?Pill Name |?Drug Name |?Pill Ingred |?Pill Imprint |?Pill Dosage |?Pill Color |?Pill Shape |?Pill Size (mm) |?Pill Scoring |?NDC |?Drug Author |format=template |template=DrugPageImages |mainlabel=- |sort=Pill Name }}
Package and Label Display Panel

{{#ask: Label Page::Copanlisib |?Label Name |format=template |template=DrugLabelImages |mainlabel=- |sort=Label Page }}
Patient Counseling Information
- Infections – Advise patients that Copanlisib can cause serious infections that may be fatal. Advise patients to immediately report symptoms of infection
- Hyperglycemia – Advise patients that an infusion-related increase in blood glucose may occur, and to notify their healthcare provider of any symptoms such as pronounced hunger, excessive thirst, headaches, or frequently urinating. Blood glucose levels should be well controlled prior to infusion
- Hypertension – Advise patients that an infusion-related increase in blood pressure may occur, and to notify their healthcare provider of any symptoms such as dizziness, passing out, headache, and/or a pounding heart. Blood pressure should be normal or well controlled prior to infusion
- Non-infectious pneumonitis – Advise patients of the possibility of pneumonitis, and to report any new or worsening respiratory symptoms including cough or difficulty breathing
- Neutropenia – Advise patients of the need for periodic monitoring of blood counts and to notify their healthcare provider immediately if they develop a fever or any signs of infection
- Severe cutaneous reactions – Advise patients that a severe cutaneous reaction may occur, and to notify their healthcare provider if they develop skin reactions (rash, redness, swelling, itching or peeling of the skin)
- Pregnancy – Advise females of reproductive potential to use effective contraceptive methods and to avoid becoming pregnant during treatment with Copanlisib and for at least one month after the last dose. Advise patients to notify their healthcare provider immediately in the event of a pregnancy or if pregnancy is suspected during Copanlisib treatment. Advise males with female partners of reproductive potential to use effective contraception during treatment with Copanlisib and for at least one month after the last dose
- Lactation – Advise women not to breastfeed during treatment with Copanlisib and for at least 1 month after the last dose

Precautions with Alcohol
Alcohol-Copanlisib interaction has not been established. Talk to your doctor regarding the effects of taking alcohol with this medication.
Brand Names
- Aliqopa
Look-Alike Drug Names
There is limited information regarding Copanlisib Look-Alike Drug Names in the drug label.
Drug Shortage
Price
References
The contents of this FDA label are provided by the National Library of Medicine.