Spinal cord injury
For patient information, click here
| Spinal cord injury | |
| ICD-10 | G95.9, T09.3 |
|---|---|
| DiseasesDB | 12327 Template:DiseasesDB2 |
| MeSH | D013119 |
Template:Search infobox Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]
Overview
Spinal cord injury causes myelopathy or damage to white matter or myelinated fiber tracts that carry sensation and motor signals to and from the brain. It also damages gray matter in the central part of the spinal, causing segmental losses of interneurons and motorneurons. Spinal cord injury can occur from many causes, including:
- Trauma such as automobile accidents, falls, gunshots, diving accidents, war injuries, etc.
- Tumor such as meningiomas, ependymomas, astrocytomas, and metastatic cancer.
- Ischemia resulting from occlusion of spinal blood vessels, including dissecting aortic aneurisms, emboli, arteriosclerosis.
- Developmental disorders, such as spina bifida, meningomyolcoele, and other.
- Neurodegenerative diseases, such as Friedreich's ataxia, spinocerebellar ataxia, etc.
- Demyelinative diseases, such as Multiple Sclerosis.
- Transverse myelitis, resulting from spinal cord stroke, inflammation, or other causes.
- Vascular malformations, such as arteriovenous malformation (AVM), dural arteriovenous fistula (AVF), spinal hemangioma, cavernous angioma and aneurysm.
Classification
The American Spinal Cord Injury Association or ASIA defined an international classification based on neurological levels, touch and pinprick sensations tested in each dermatome, and strength of ten key muscles on each side of the body, i.e. shoulder shrug (C4), elbow flexion (C5), wrist extension (C6), elbow extension (C7), hip flexion (L2), knee extension (L3), ankle dorsiflexion (L4), long toe extension (L5), and ankle plantar flexion (S1). Each muscle is graded on a scale of 0-5 where 0 is paralyzed, 1 is slight movement, 2 is definite movement, 3 is movement against gravity, 4 is movement against manual resistance, and 5 is normal. The scores of the muscles add up to 100. The pinprick and touch sensations are grade separately for each dermatome on a scale of 0-2 where 0 is absent sensation, 1 is abnormal sensation, and 2 is normal. These add up to 112 points each for pinprick and touch.
Traumatic spinal cord injury is classified into five types by the American Spinal Injury Association (ASIA) and the International Spinal Cord Injury Classification System.
- A indicates a "complete" spinal cord injury where no motor or sensory function is preserved in the sacral segments S4-S5. A complete injury is one in which there is some neurological level below which there is no motor or sensory function. Since the S4-S5 segment is the lower segmental, absence of motor and sensory function indicates "complete" spinal cord injury.
- B indicates an "incomplete" spinal cord injury where sensory but not motor function is preserved below the neurological level and includes the sacral segments S4-S5. This is typically a transient phase and if the person recovers any motor function below the neurological level, that person essentially becomes a motor incomplete, i.e. ASIA C or D.
- C indicates an "incomplete" spinal cord injury where motor function is preserved below the neurological level and more than half of key muscles below the neurological level have a muscle grade of less than 3.
- D indicates an "incomplete" spinal cord injury where motor function is preserved below the neurological level and at least half of the key muscles below the neurological level have a muscle grade of 3 or more.
- E indicates "normal" where motor and sensory scores are normal. Note that it is possible to have spinal cord injury and neurological deficit with completely normal motor and sensory scores.
In addition, there are several clinical syndromes associated with incomplete spinal cord injuries.
- The Central Cord syndrome is associated with greater loss of upper limb function compared to lower limbs.
- The Brown-Séquard syndrome results from injury to one side with the spinal cord, causing weakness and loss of proprioception on the side of the injury and loss of pain and thermal sensation of the other side.
- The Anterior Spinal syndrome results from injury to the anterior part of the spinal cord, causing weakness and loss of pain and thermal sensations below the injury site but preservation of proprioception that is usually carried in the posterior part of the spinal cord.
- Tabes Dorsalis results from injury to the posterior part of the spinal cord, usually from infection diseases such as syphilis, causing loss of touch and proprioceptive sensation.
- Conus Medullaris syndrome results from injury to the tip of the spinal cord, located at L1 vertebra.
- Cauda Equina syndrome is, strictly speaking, not really spinal cord injury but injury to the spinal roots below the L1 vertebra.
One can have spine injury without spinal cord injury. Many people suffer transient loss of function ("stingers") in sports accidents or pain in "whiplash" of the neck without neurological loss and relatively few of these suffer spinal cord injury sufficient to warrant hospitalization. In the United States, the incidence of spinal cord injury has been estimated to be about 35 cases per million per year, or approximately 10,500 per year (35 * 300). In China, the incidence of spinal cord injury was recently estimated to be as high as 65 cases per million per year in urban areas. If so, assuming a population of 1.3 billion, this would suggest an incidence of 84,500 per year (65 * 1300).
The prevalence of spinal cord injury is not well known in many large countries. In some countries, such as Sweden and Iceland, registries are available. About 450,000 people in the United States live with spinal cord injury (one in 670), and there are about 11,000 new spinal cord injuries every year (one in 30,000). The majority of them (78%) involve males between the ages of 16-30 and result from motor vehicle accidents (42%), violence (24%), or falls (27%).
The Effects of Spinal Cord Injury
| |
| Segmental Spinal Cord Level and Function | |
|---|---|
| Level | Function |
| Cl-C6 | Neck flexors |
| Cl-Tl | Neck extensors |
| C3, C4, C5 | Supply diaphragm (mostly C4) |
| C5, C6 | Shoulder movement, raise arm (deltoid); flexion of elbow (biceps); C6 externally rotates the arm (supinates) |
| C6, C7 | Extends elbow and wrist (triceps and wrist extensors); pronates wrist |
| C7, T1 | Flexes wrist |
| C7, T1 | Supply small muscles of the hand |
| T1 -T6 | Intercostals and trunk above the waist |
| T7-L1 | Abdominal muscles |
| L1, L2, L3, L4 | Thigh flexion |
| L2, L3, L4 | Thigh adduction |
| L4, L5, S1 | Thigh abduction |
| L5, S1, S2 | Extension of leg at the hip (gluteus maximus) |
| L2, L3, L4 | Extension of leg at the knee (quadriceps femoris) |
| L4, L5, S1, S2 | Flexion of leg at the knee (hamstrings) |
| L4, L5, S1 | Dorsiflexion of foot (tibialis anterior) |
| L4, L5, S1 | Extension of toes |
| L5, S1, S2 | Plantar flexion of foot |
| L5, S1, S2 | Flexion of toes |
The exact effects of a spinal cord injury vary according to the type and level injury, and can be organized into two types:
- In a complete injury, there is no function below the "neurological" level, defined as the lowest level that has intact neurological function. If a person has some level below which there is no motor and sensory function, the injury is said to be "complete". Recent evidence suggest that less than 5% of people with "complete" spinal cord injury recover locomotion.
- A person with an incomplete injury retains some sensation or movement below the level of the injury. The lowest spinal cord level is S4-5, representing the anal sphincter and peri-anal sensation. So, if a person is able to contract the anal sphincter voluntarily or is able to feel peri-anal pinprick or touch, the injury is said to be "incomplete". Recent evidence suggest that over 95% of people with "incomplete" spinal cord injury recover some locomotory ability.
In addition to a loss of sensation and motor function below the point of injury, individuals with spinal cord injuries will often experience other complications of spinal cord injury:
- Bowel and bladder function is regulated by the sacral region of the spine, so it is very common to experience dysfunction of the bowel and bladder, including infections of the bladder, and anal incontinence.
- Sexual function is also associated with the sacral region, and is often affected.
- Injuries of the C-1, C-2 will often result in a loss of breathing, necessitating mechanical ventilators or phrenic nerve pacing.
- Inability or reduced ability to regulate heart rate, blood pressure), sweating and hence body temperature.
- Spasticity (increased reflexes and stiffness of the limbs).
- Neuropathic pain.
- Autonomic dysreflexia or abnormal increases in blood pressure, sweating, and other autonomic responses to pain or sensory disturbances.
- Atrophy of muscle.
- Osteoporosis (loss of calcium) and bone degeneration.
- Gallbladder and renal stones.
The Location of the Injury
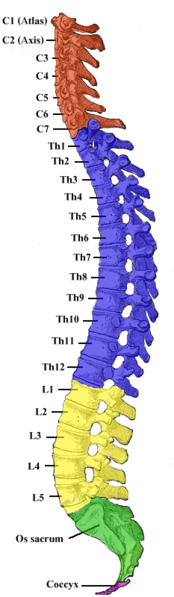
Knowing the exact level of the injury on the spinal cord is important when predicting what parts of the body might be affected by paralysis and loss of function.
Below is a list of typical effects of spinal cord injury by location (refer to the spinal cord map to the right). Please keep in mind that while the prognosis of complete injuries are predictable, incomplete injuries are very variable and may differ from the descriptions below.
Cervical injuries
Cervical (neck) injuries usually result in full or partial tetraplegia. Depending on the exact location of the injury, one with a spinal cord injury at the cervical level may retain some amount of function as detailed below, but are otherwise completely paralyzed.
- C3 vertebrae and above : Typically lose diaphragm function and require a ventilator to breathe.
- C4 : May have some use of biceps and shoulders, but weaker
- C5 : May retain the use of shoulders and biceps, but not of the wrists or hands.
- C6 : Generally retain some wrist control, but no hand function.
- C7 and T1 : Can usually straighten their arms but still may have dexterity problems with the hand and fingers. C7 is generally the level for functional independence.
Thoracic injuries
Injuries at the thoracic level and below result in paraplegia. The hands, arms, head, and breathing are usually not affected.
- T1 to T8 : Most often have control of the hands, but lack control of the abdominal muscles so control of the trunk is difficult or impossible. Effects are less severe the lower the injury.
- T9 to T12 : Allows good trunk and abdominal muscle control, and sitting balance is very good.
Lumbar and Sacral injuries
The effect of injuries to the lumbar or sacral region of the spinal canal are decreased control of the legs and hips, urinary system, and anus.
Central Cord and Other Syndromes
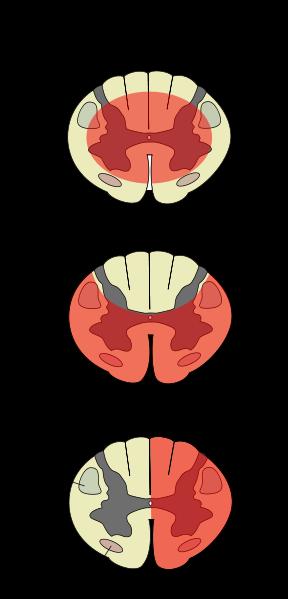
Central cord syndrome (picture 1) is a form of incomplete spinal cord injury characterized by impairment in the arms and hands and, to a lesser extent, in the legs. This is also referred to as inverse paraplegia, because the hands and arms are paralyzed while the legs and lower extremities work correctly.
Most often the damage is to the cervical or upper thoracic regions of the spinal cord, and characterized by weakness in the arms with relative sparing of the legs with variable sensory loss.
This condition is associated with ischemia, hemorrhage, or necrosis involving the central portions of the spinal cord (the large nerve fibers that carry information directly from the cerebral cortex). Corticospinal fibers destined for the legs are spared due to their more external location in the spinal cord.
This clinical pattern may emerge during recovery from spinal shock due to prolonged swelling around or near the vertebrae, causing pressures on the cord. The symptoms may be transient or permanent.
Anterior cord syndrome (picture 2) is also an incomplete spinal cord injury. Below the injury, motor function, pain sensation, and temperature sensation is lost; touch, proprioception (sense of position in space), and vibration sense remain intact. Posterior cord syndrome (not pictured) can also occur, but is very rare.
Brown-Séquard syndrome (picture 3) usually occurs when the spinal cord is hemisectioned or injured on the lateral side. On the ipsilateral side of the injury (same side), there is a loss of motor function, proprioception, vibration, and light touch. Contralaterally (opposite side of injury), there is a loss of pain, temperature, and deep touch sensations.
Treatment
Treatment for acute traumatic spinal cord injuries have consisted of giving high dose methylprednisolone if the injury occurred within 8 hours. The recommendation is primarily based on the National Acute Spinal Cord Injury Studies (NASCIS) II and III. Some of the claims of the studies have been challenged as being from faulty interpretation of the data.
Breakthrough medical research shows stem cell transplants could have the potential to help or cure paralysis caused by spinal injury. Stem cells are primal cells found in all multi-cellular organisms. They can be made to differentiate into a range of specialized cells including nerve cells, which can be transplanted into the body.
Special Tests to Determine Spine Pathology Sign Pathology Long Tract Signs Babinski: first toe dorsiflexion with fanning out of other toes when sharp instrument is rubbed on lateral border of foot from calcaneus to head of first metatarsal Upper motor neuron lesion; corticospinal tract. Hoffman: flick distal phalanx away from palm; look for pincer effect between thumb and index finger; look for asymmetry. Cord compression; CNS dysfunction; brisk muscle stretch reflex Tramner reflex: Elevate middle finger above other fingers and flick distal phalanx toward palm; look for pincer effect between thumb and index finger; look for asymmetry. Cord compression; CNS dysfunction; brisk muscle stretch reflex Inverted radial reflex: finger flexion upon testing brachioradialis reflex Cervical myelopathy Finger escape: abduction of fifth finger because of weak hand intrinsics Cervical myelopathy Lhermitte: neck flexion causing lightning-like sensation radiating down back Cervical stenosis; disk herniation; multiple sclerosis with posterior column dysfunction (original description) Cross adductor: stimulate patellar reflex and note contralateral thigh adductor contraction UMN lesion Chaddock: laterally abduct the little toe briskly and let it slap back against the other toes or flick the third or fourth toe down rapidly; note dorsiflexion of the great toe. UMN lesion Jaw jerk reflex: gently tap on patient's jaw with patient's mouth slightly open; a positive reflex is when the jaw closes In a patient with UMN signs, a positive jaw jerk test suggests that the etiology is not in the cervical spine but that the pathology is located above the level of the pons Nerve Root Compression Spurling: extend and bend the neck laterally and apply axial load to the top of the head; patient will report radicular pain. Cervical nerve root compression Straight-leg raise (SLR): with patient supine or sitting perform, SLR and patient will report pain in the distribution of the nerve root irritated; for sciatic involvement, the pain must extend distal to the knee Nerve root compression Contralateral SLR (Frajerstajn): raising asymptomatic side causes pain down symptomatic side Indicates either a central disk herniation or an axillary herniation on the symptomatic side Lasegue: perform SLR and then dorsiflex the ankle; should exacerbate SLR radiculopathy; less than 70 degrees of hip flexion is a positive Lasegue sign Nerve root compression Bowstring: with patient supine, raise leg, flex knee, then apply pressure to popliteal fossa to elicit radicular pain Nerve root compression Cram test: similar to Lasègue sign; extend hip then straighten leg to elicit pain Nerve root compression Milgram: patient raises both legs off examining table and holds for 30 seconds; note radiculopathy Nerve root compression Naffziger: compress neck veins for 10 seconds with patient supine; coughing produces radiculopathy Nerve root compression Hoover: examiner places hands under patient's heel while the supine patient tries to perform SLR with the contralateral leg If the patient is malingering or not trying, then there will be a lack of downward pressure on the hand under the heel (opposite foot not performing the SLR) Femoral stretch: with patient prone or lying on side, the hip is held in extension and the knee is flexed Femoral neuritis or L3 or L4 radiculopathy Other Signs Wartenberg: unopposed abduction of the little finger Ulnar nerve paresis Beevor: have patient perform a quarter abdominal sit-up with arms crossed behind head; note any up, down, or sideways movement of the umbilicus Lower abdominal muscles (controlled by spinal cord below T9) are weaker than upper abdominal muscles Cremasteric reflex (males): stroke the inner thigh (genitofemoral nerve) and note ascent of the ipsilateral testicle Bulbocavernosus reflex: compress glans penis or pull on a Foley catheter; note contraction of the anal sphincter When present, signals end of spinal cord shock after cord injury Anal wink: apply sharp stimulus and note contraction of the external anal sphincter When present, signals end of spinal cord shock after cord injury Patrick (FABER) test: the hip is placed in a flexed, abducted, and externally rotated position, and ipsilateral foot is placed on opposite knee; pressure is put on ipsilateral knee and opposite ASIS Sacroiliac pain Localizing dermatomes C6: thumb C7: middle finger C8: small finger T4: nipple T10: umbilicus L1: inguinal ligament
Waddell Signs for Nonorganic Pathology Signs Outcome Observations: Pain out of proportion to stimulus (example, light touch) Pain in a nonanatomic distribution Poor outcome after operative or nonoperative treatment if 3 or more positive signs Exaggerated pain response Four tests (none should be positive): 1. Skin roll test: roll skin between index and thumb and note radicular symptoms 2. Head compression: apply 5 pounds of load and note 3. Twist test: patient standing with feet planted, examiner rotates torso left and right and notes pain 4. Flip test: Perform sitting and supine SLR and note any difference in pain
Introduction:
Fractures and dislocations of the spine are serious injuries that most commonly occur in young people. The most common causes of severe spinal trauma are motor vehicle accidents, falls, diving accidents, and gunshot wounds. Spinal injury should be suspected in any patient with a head injury or severe facial or scalp lacerations. In any patient with recent trauma, complaints of neck pain or spinal pain should be considered indicative of a spinal injury until proved otherwise.
Risk factors for spinal injury:
1.inability to assess neck pain because of a secondary distracting injury,
2.abnormal neurological findings,
3. a history of transient neurological symptoms,
4physical signs of spinal trauma (e.g., ecchymosis and abrasions),
5.unreliable examination, significant head or face trauma, or
6.an inconsolable child .
Manifestations of Spinal Shock:After a spinal cord injury,
spinal shock occurs. It is manifested by
1) flaccid paralysis,
2)hypotonia,
3)areflexia, and
4)an absent bulbo-cavernosus reflex (BCR).
At this time, the neurologic level cannot be determined. The BCR typically returns during the first 24 to 48 hours after the injury and can be tested by squeezing the glands penis, pubis, or pulling on a Foley and eliciting contraction of the anal sphincter.
Goals of Spine Trauma Care
1. Protect against further injury during evaluation and management
2. Quickly identify spine injury or document absence of spine injury
3. Optimize conditions for maximal neurological recovery
4. Maintain or restore spinal alignment
5. Minimize loss of spinal mobility
6. Obtain a healed and stable spinal column
7. Facilitate rehabilitation
Complete Spinal Cord Injury (SCI):
Indicates no function below a given levels after spinal shock is over, where an incomplete injury has some distal neurologic function present especially sacral sparing.
Acute Management for SCI: Initial management : 1)spine immobilization 2) full traumawork-up, and 3) methylprednisolone within the first 8 hours after injury.
Steroid Protocol for SCI:The steroid protocol for giving methylprednisolone after SCI is given. Most benefit occurs in the first 8 hours, and additional effect occurs within the first 24 hours it is as follows: • 0 to 3 hours: 30 mg/kg loading dose, then 5.4 mg/kg for 23 hours • 3 to 8 hours: 30 mg/kg loading dose, then 5.4 mg/kg for 48 hours • 8 hours: no methylprednisolone
Definitions of Terms Describing Spinal Cord Injury
Impairment Loss of motor and sensory function
Disability Loss in daily life functioning
Tetraplegia Loss of motor and or sensory function in the cervical segments
Paraplegia Loss of motor and or sensory function in the thoracic, lumbar, or sacral segments
Dermatome Area of skin innervated by sensory axons within each segmental nerve
Myotome Collection of muscle fibers by the motor axons within each segmental nerve
Neurologic level The most caudal segment with normal sensory and motor function on both sides
Sensory level The most caudal segment with normal sensory function on both sides
Motor level The most caudal segment with normal motor function on both sides
Skeletal level Radiographic level of greatest vertebral damage
Sensory score Numeric summary value of sensory impairment
Motor score Numeric summary value of motor impairment
Incomplete injury Partial preservation of sensory and/or motor function below the neurologic level and sensory and/or motor preservation of the lowest sacral segment
Complete injury Absence of sensory and motor function in the lowest sacral segment
Dermatomes and myotomes caudal to the neurologic level that remain
partially innervated
Diagnostic imaging:
1.Plain radiography : anteroposterior and lateral views.
2.Computed Tomography.
3.Magnetic Resonance Imaging. Most common sites for spine injuries are: 1. cranio-cervical, 2. cervico-thoracic, and 3. thoraco-lumbar. Initial evaluation of trama patient: Following 3 images provide crucial information that facilitates resuscitation. 1. lateral cervical spine x-ray 2. Obtaining an AP chest x-ray, an 3. AP pelvis x-ray They are often the most difficult to see on standard x-rays. Among these injuries, the most serious and most frequently missed is the cranio-cervical dissociation. A systematic approach to reading cervical x-rays can help reduce the chances of missing an important injury. What to look for in lateral xray? 1.Alignment of the cervical vertebrae is assessed by examining longitudinal lines along vertebral bodies, lamina, and spinous processes. 2.Examining alignment of the lamina in the upper cervical vertebrae is particularly helpful in excluding injuries of the cranio-cervical junction in both children and adults. 3.The prevertebral soft tissues can be useful as an indicator of swelling from acute hemorrhage. 4.Increased thickness and altered contour of the pharyngeal tissue anterior to C2 (i.e., convexity instead of concavity caudal to the C1 anterior arch) suggest acute cranio-cervical injury.
Computed Tomography:
CT and MRI may be useful together in determining the presence and extent of spinal column injury . MRI is superior in demonstrating spinal cord pathology and intervertebral disc herniation. CT is superior to MRI in demonstrating bony injury.
Magnetic Resonance Imaging: MRI is useful for imaging soft tissues and bone. MRI shows edema and hemorrhage associated with acute spinal cord injury. Increased cord signal and parenchymal cord hemorrhage indicate poor prognosis for neurologic recovery . MRI is useful for assessing the cranio-cervical junction. MRI provides noninvasive assessment of the vertebral artery blood flow in cervical trauma, which can be frequently disrupted in cervical spine injuries.
Descriptions of Incomplete Cord Injury Patterns
Syndrome
Lesion Clinical Presentation
Bell's cruciate paralysis Long tract injury at the level of decussation in brainstem Variable cranial nerve involvement, greater upper extremity weakness than lower, greater proximal weakness than distal
Anterior cord Anterior gray matter, descending corticospinal motor tract, and spinothalamic tract injury with preservation of dorsal columns Variable motor and pain and temperature sensory loss with preservation of proprioception and deep pressure sensation
Central cord Incomplete cervical white matter injury Sacral sparing and greater weakness in the upper limbs than the lower limbs
Brown-Sequard Injury to one lateral half of cord and preservation of contralateral half Ipsilateral motor and proprioception loss and contralateral pain and temperature sensory loss
Conus medullaris Injury to the sacral cord (conus) and lumbar nerve roots within the spinal canal Areflexic bladder, bowel, and lower limbs
May have preserved bulbocavernosus and micturition reflexes
Cauda equina Injury to the lumbosacral nerve roots within the spinal canal Areflexic bladder, bowel, and lower limbs
Root injury Avulsion or compression injury to single or multiple nerve roots (brachial plexus avulsion) Dermatomal sensory loss, myotomal motor loss, and absent deep tendon reflexes
Neurogenic and Hypovolemic Shock
Neurogenic Shock* Hypovolemic Shock
As the result of loss of sympathetic outflow As the result of hemorrhage
Hypotension Hypotension
Bradycardia Tachycardia
Warm extremities Cold extremities
Normal urine output Low urine output
ASIA Impairment Scale A Complete No motor or sensory function in the lowest sacral segment (S4-S5) B Incomplete Sensory function below neurologic level and in S4-S5, no motor function below neurologic level C Incomplete Motor function is preserved below neurologic level and more than half of the key muscle groups below neurologic level have a muscle grade <3 D Incomplete Motor function is preserved below neurologic level and at least half of the key muscle groups below neurologic level have a muscle grade = 3 E Normal Sensory and motor function is normal
(ASIA, American Spinal Injury Association.)