Citrullinemia
|
WikiDoc Resources for Citrullinemia |
|
Articles |
|---|
|
Most recent articles on Citrullinemia Most cited articles on Citrullinemia |
|
Media |
|
Powerpoint slides on Citrullinemia |
|
Evidence Based Medicine |
|
Clinical Trials |
|
Ongoing Trials on Citrullinemia at Clinical Trials.gov Trial results on Citrullinemia Clinical Trials on Citrullinemia at Google
|
|
Guidelines / Policies / Govt |
|
US National Guidelines Clearinghouse on Citrullinemia NICE Guidance on Citrullinemia
|
|
Books |
|
News |
|
Commentary |
|
Definitions |
|
Patient Resources / Community |
|
Patient resources on Citrullinemia Discussion groups on Citrullinemia Patient Handouts on Citrullinemia Directions to Hospitals Treating Citrullinemia Risk calculators and risk factors for Citrullinemia
|
|
Healthcare Provider Resources |
|
Causes & Risk Factors for Citrullinemia |
|
Continuing Medical Education (CME) |
|
International |
|
|
|
Business |
|
Experimental / Informatics |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]; Associate Editor(s)-in-Chief:
| Citrullinemia | ||
 | ||
|---|---|---|
| Citrulline | ||
| ICD-10 | E72.2 | |
| ICD-9 | 270.6 | |
| OMIM | 215700 605814 603471 | |
| DiseasesDB | 29676 Template:DiseasesDB2 | |
| eMedicine | ped/406 | |
| MeSH | C10.228.140.163.100.175 | |
Overview
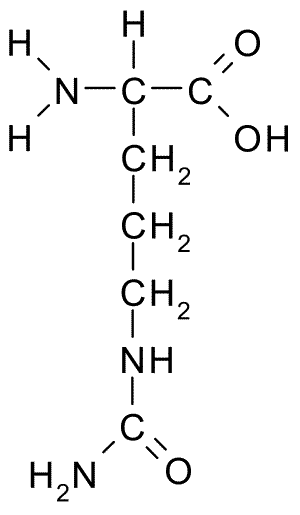
Citrullinemia is an inherited disorder that causes ammonia and other toxic substances to accumulate in the blood. Two forms of citrullinemia have been described; they have different signs and symptoms and are caused by mutations in different genes. Citrullinemia belongs to a class of genetic diseases called urea cycle disorders. The urea cycle is a sequence of chemical reactions that takes place in the liver. These reactions process excess nitrogen, generated when protein is used by the body, to make a compound called urea that is excreted by the kidneys.
Both types of citrullinemia are inherited in an autosomal recessive pattern.
Historical Perspective
Classification
Types
Type I
Type I citrullinemia (Online Mendelian Inheritance in Man (OMIM) 215700, also known as classic citrullinemia) usually becomes evident in the first few days of life. Affected infants typically appear normal at birth, but as ammonia builds up in the body they develop a lack of energy (lethargy), poor feeding, vomiting, seizures, and loss of consciousness. These medical problems can be life-threatening in many cases. Less commonly, a milder form of type I citrullinemia can occur in childhood or adulthood. Some people with gene mutations that cause type I citrullinemia never experience signs and symptoms of the disorder.
Type I citrullinemia is the most common form of the disorder, affecting about 1 in 57,000 births worldwide. Mutations in the ASS gene cause type I citrullinemia. The enzyme made by this gene, argininosuccinate synthetase (EC 6.3.4.5), is responsible for one step of the urea cycle. Mutations in the ASS gene reduce the activity of the enzyme, which disrupts the urea cycle and prevents the body from processing nitrogen effectively. Excess nitrogen, in the form of ammonia, and other byproducts of the urea cycle accumulate in the bloodstream, leading to the characteristic features of type I citrullinemia.
Type II
The signs and symptoms of type II citrullinemia (Online Mendelian Inheritance in Man (OMIM) 605814 and Online Mendelian Inheritance in Man (OMIM) 603471) usually appear during adulthood and mainly affect the nervous system. Characteristic features include confusion, abnormal behaviors (such as aggression, irritability, and hyperactivity), seizures, and coma. These signs and symptoms can be life-threatening, and are known to be triggered by certain medications, infections, and alcohol intake in people with type II citrullinemia.
Type II citrullinemia may also develop in people who had a liver disorder called neonatal intrahepatic cholestasis during infancy. This condition blocks the flow of bile and prevents the body from processing certain nutrients properly. In many cases, the signs and symptoms resolve within a year. Years or even decades later, however, some of these people develop the characteristic features of adult type II citrullinemia.
Type II citrullinemia is primarily found in the Japanese population, where it occurs in an estimated 1 in 100,000 to 230,000 individuals. Type II has also been reported in people from East Asian and Middle Eastern populations. Mutations in the SLC25A13 gene are responsible for type II citrullinemia. This gene makes a protein called citrin, which normally shuttles certain molecules in and out of mitochondria. These molecules are essential for the urea cycle and are also involved in making proteins and nucleotides. Mutations in the SLC25A13 mutation typically prevent the production of any functional citrin, which inhibits the urea cycle and disrupts the production of proteins and nucleotides. The resulting buildup of ammonia and other toxic substances leads to the signs and symptoms of type II citrullinemia. Researchers have determined that many infants with neonatal intrahepatic cholestasis have the same mutations in the SLC25A13 gene as adults with type II citrullinemia.
Pathophysiology
Causes
Differentiating Citrullinemia from Other Diseases
Epidemiology and Demographics
Risk Factors
Screening
Natural History, Complications, and Prognosis
Diagnosis
Diagnostic Criteria
History and Symptoms
Physical Examination
Laboratory Findings
Imaging Findings
Other Diagnostic Studies
Treatment
Medical Therapy
Surgery
Prevention
See also
External links
- The U.S. National Library of Medicine (This article incorporates public domain text from this source)