Amenorrhea surgery
|
Amenorrhea Microchapters |
|
Patient Information |
|---|
|
Diagnosis |
|
Treatment |
|
Case Studies |
|
Amenorrhea surgery On the Web |
|
American Roentgen Ray Society Images of Amenorrhea surgery |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]; Associate Editor(s)-in-Chief: Eiman Ghaffarpasand, M.D. [2]
Overview
The mainstay of treatment for amenorrhea is medical therapy. Surgery is usually reserved for patients with either hypothalamus or pituitary tumors, Turner syndrome, and genital anatomical defects (imperforate hymen or transverse vaginal septum). The surgical treatment for hypothalamus or pituitary tumors includes tumor resection via endoscopic transsphenoidal surgery. Ovaries have to be excised in Turner syndrome to prevent malignant transformation. Small incision is the preferred surgical procedure for imperforate hymen and septal excision is the main treatment for transverse vaginal septum.
Surgery
Pituitary and hypothalamus tumors
 |
| _fioC34LZeg|500}} |
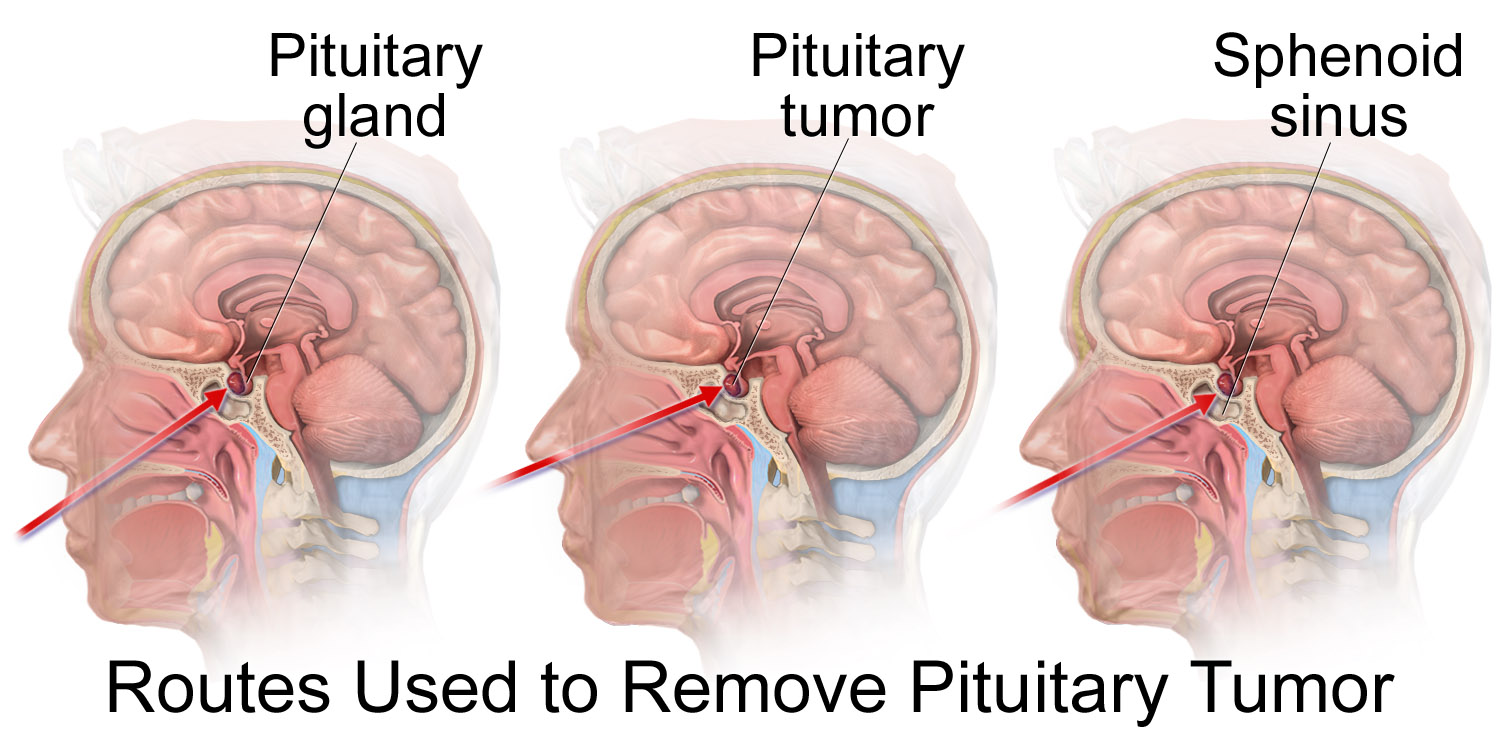
Endoscopic transsphenoidal surgery[1]
- In this method, the pituitary tumor is excised through nostrils by means of a tiny fiber-optic endoscopic tube.
- First, bilateral nasal septal mucosa is incised in a C-shaped manner. The septal bone is approached through this incision.
- Then, sphenoidal rostrum and anterior wall of sphenoid sinus are gradually removed, a bone window is opened through the skull space.
- After that, the dura mater is passed and the lesion becomes visible.
- Finally, the tumor is removed using curette and basket with suction.
- Advantages:
- Disadvantages:
- Not for large tumors
- Recurrent sinusitis in the future
- Low cure rate in case of suprasellar adhesion to adjunct tissues
Craniotomy[2]
- Although the preferred procedure to excise the pituitary tumors is a trans-sphenoidal approach, but in some cases (1-4%) the size of the tumor or any suprasellar adhesion may require trans-cranial method.
- Situations requiring transcranial method include:
- Isolation by a narrow waist at the diaphragma sellae
- Containment within the cavernous sinus lateral to the carotid artery
- Projection anteriorly onto the planum sphenoidal
- Projection laterally into the middle fossa
- Skull base surgical procedure is also the option for pituitary tumor treatment but may encounter the problems that transsphenoidal method is faced with.
- Advantages:
- Resection of large tumors
- Ability to excise the tumors with suprasellar specific conditions
- Disadvantages:
- Long duration of post-operation recovery
- Damage to other parts of the brain
| 4YD9629Mgag|500}} |
Turner syndrome[3]
- Since the dysgenetic ovaries in Turner syndrome have a higher risk of malignancy, they have to be resected whenever the disease is diagnosed.
- In the presence of Y chromosome, the chance of becoming malignant is higher in Turner syndrome, and oophorectomy (even salpingo-oophorectomy) has to be performed urgently.
Anatomical defect
Imperforate hymen
- The surgical procedure is to make a small incision on hymen, excised the extra hymen membrane (small central hymenotomy).[4]
Transverse vaginal septum
- The surgical procedure includes excision of septum via vaginal canal. Prognosis is generally good with most patients reporting normal menstruation cycles after surgery.[5]
References
- ↑ Fan YP, Lv MH, Feng SY, Fan X, Hong HY, Wen WP; et al. (2014). "Full Endoscopic Transsphenoidal Surgery for Pituitary Adenoma-emphasized on Surgical Skill of Otolaryngologist". Indian J Otolaryngol Head Neck Surg. 66 (Suppl 1): 334–40. doi:10.1007/s12070-011-0317-4. PMC 3918297. PMID 24533411.
- ↑ Youssef AS, Agazzi S, van Loveren HR (2005). "Transcranial surgery for pituitary adenomas". Neurosurgery. 57 (1 Suppl): 168–75, discussion 168–75. PMID 15987585.
- ↑ Kanakatti Shankar R, Inge TH, Gutmark-Little I, Backeljauw PF (2014). "Oophorectomy versus salpingo-oophorectomy in Turner syndrome patients with Y-chromosome material: clinical experience and current practice patterns assessment". J. Pediatr. Surg. 49 (11): 1585–8. doi:10.1016/j.jpedsurg.2014.06.012. PMID 25475798.
- ↑ Temizkan O, Kucur SK, Ağar S, Gözükara I, Akyol A, Davas I (2012). "Virginity sparing surgery for imperforate hymen: report of two cases and review of literature". J Turk Ger Gynecol Assoc. 13 (4): 278–80. doi:10.5152/jtgga.2012.46. PMC 3881718. PMID 24592057.
- ↑ Al-Abdulhadi F, Diejomaoh MF, El Biaa A, Jirous J, Al-Qenae M (2010). "Excision of high vaginal septum". Arch. Gynecol. Obstet. 281 (5): 955–7. doi:10.1007/s00404-009-1293-8. PMID 19943056.