Venous thromboembolism
Editors-in-Chief: C. Michael Gibson, M.S., M.D. Associate Editor-In-Chief: Ujjwal Rastogi, MBBS [1]
Synonyms and keywords: VTE
Overview
Venous thromboembolism (VTE) is a hypernym which includes Deep venous thrombosis (DVT) and pulmonary embolism (PE). It is a major public health problem and one of the most common cause of preventable cause of death in hospital patients. It is the third most common cardiovascular disorder after coronary artery disease and stroke. It is frequently underestimated and misdiagnosed and failure to provide adequate prophylaxis and therapy can be fatal for the patient.
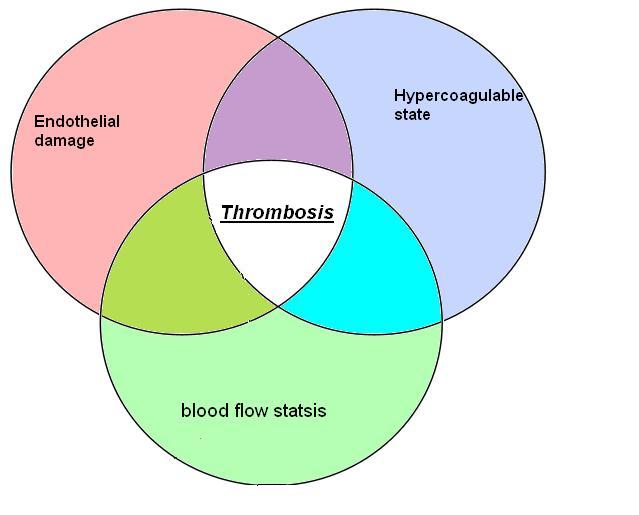
Pathophysiology
Figure : Virchow's triad encompasses three broad categories of factors that are thought to contribute to venous thrombosis.
Classification Scheme
VTE includes DVT and PE, which are further divided into:
- Deep Venous Thrombosis: Its classified as
- Superficial
- Upper extremity
- Isolated Calf
- Proximal
- Pulmonary embolism:its classified as
- Silent
- Symptomatic
- Fatal
Epidemiology
Annualy, more than 900,000 cases are reported to have clinicaly evident Venous thromboembolism. More than 300,000 deaths are attributed to pulmonary embolism in United states[1]. More than 25,000 people die in England from venous thromboembolism developed in hospital. This is more than the total number of deaths attributable to Breast cancer, AIDS, and road traffic accidents, when combined together. Close to a third of total patients encounter some sort of a long term effects.[2]
Risk Factors
Recently a research group[3]. has postulated a risk-prediction algorithm for VTE. This algorith helps:
- Estimates individual risk for VTE
- To start prophylaxis in patients at risk for VTE.
This algorithm does not work in these conditions:
- History of venous thrombosis
- Family history of venous thrombosis.
- Pregnant patients
- Patients on Anticoagulations
- Symptoms suggestive of thrombosis.
The various variables that are taken into account are as follows
| Age |
| Body mass index |
| Smoking status (non-smoker; ex-smoker; light, moderate, or heavy smoker) |
| Townsend deprivation score |
| Varicose veins |
| Congestive cardiac failure |
| Rheumatoid arthritis |
| Chronic renal disease |
| Inflammatory bowel disease |
| Cancer:(lung, gastrointestinal, pancreas, renal, breast, prostate, other) |
| Recent hospital admission |
| Recent hip fracture or hip surgery (or both) |
| Current use of antipsychotic drugs:(none, atypical, typical) |
| Current use of tamoxifen |
| Current use of hormone replacement therapy: (none, equine or non-equine hormone replacement therapy) |
| Use of antiplatelets |
| Cardiovascular disease(stroke, transient ischaemic attack, or coronary artery disease) |
| Atrial fibrillation |
| Asthma |
| Chronic obstructive pulmonary disease |
| Family history of venous thromboembolism |
To calculate the risk prediction click here
Differential Diagnosis
There are other conditions that can mimic VTE
- Venous
- Superficial thrombophlebitis
- Post-thrombotic syndrome
- Chronic venous insufficiency
- Venous obstruction
- Other
- Cellulitis
- Baker's cyst
- Torn gastrocnemius muscle
- Fracture
- Haematoma
- Acute arterial ischaemia
- Lymphoedema
- Hypoproteinaemia (for example, cirrhosis, nephrotic syndrome)
Complication
Acute
- Sudden death.
Chronic
- Long term morbidity and reduced survival.
- Post-thrombotic Syndrome.
- Pulmonary Hypertension.
These long term complications increase treatment cost and decrease patients quality of life. Inflation-adjusted hospital treatment cost in the year 2002 was an average $ 16,000 per patient[4].
Diagnosis
History & Symptoms
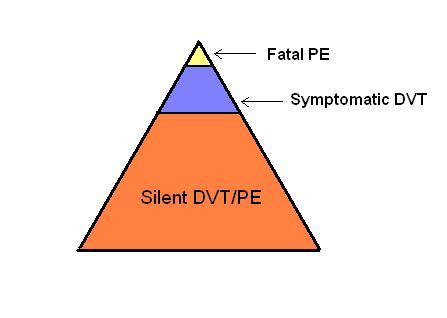
Only 10-20% of VTE is clinically recognized, as depicted by the figure below
Figure :The challenge in diagnosis of VTE
As VTE involves both DVT and PE, the patient can present with complaints of either of the disease.
- With PE, depending upon the severity of the disease, the patient experience
- Shortness of breath
- Loss of Consciousness(in case of massive PE.)
- A smaller PE near the pleura can present with
- While with DVT, patient can complain of
- swelling of lower extremity which can be warm and tender.
Physical examination
Appearance of the Patient
- Tachypnea is the most common sign of PE.
- Other sign that may be present are
- Tachycardia
- Loud S2
- Cyanosis
- Signs of DVT.
Lab Tests
- Arterial blood gas
- Plasma D-dimer
- Plasma D-dimer>500 ng/ml, PE present (Found to be 97% sensitive and 45% specific)
- Plasma D-dimer<500 excludes PE (Have a high negative predictive value)
- Workup for hypercoagulation: which include
- Activated protein C resistance
- factor V Leiden mutation
- Protein C
- protein S, free and total.
- Antithrombin
- Lupus anticoagulant
- Anticardiolipin antibodies
- Plasma homocysteine values
Electrocardiogram
ECG is important as it helps in ruling out myocardial infarction which also present with chest pain.
Chest x ray
It is more helpful in making an alternative diagnoses (Eg. pneumonia which can present with dyspnea and chest pain), than for diagnosing VTE. Xray findings are most often normal in patients with PE, It may reveal:
- Enlarged right descending pulmonary artery
- Decreased pulmonary vascularity (Westermark sign)
- Elevation of the hemidiaphragm (Hampton hump)
In case of an infarction:
- A wedge-shaped infiltrate or
- Pleural effusion might be present.
Ultrasonography
- A Doppler USG detects thrombus within a vein.
- Normal vein:free of internal echoes, compresseble.
- Acute DVT:internal echoes are present, non compressible vein.
With the color flow Doppler, motion and the direction of flow are assessed in a far better way.
CT
It involves the pulmonary vessels imaging by use of intravenous contrast material and is diagnosed by filling defects, which are either central or adherent to the wall.
- Advantages
- Minimally invasive
- Allows concurrent visualization of the parenchyma, pleura, and mediastinum.
- Limitations
- Need for contrast
- Dose of radiation is comparatively higher than that of other diagnostic procedures
Prophylaxis
A study involving data from 16 acute care hospitals confirmed the occurrence of VTE in patient who did not received thrombo-prophylaxis in-spite of being at risk and having no contraindication for thromboprophylaxis [5].
VTE occurs in approximately 50% patients undergoing major orthopedic surgery who do not receive appropriate thromboprophylaxis [2].
In post-surgical patients, following strategies have been helpful in reducing the risk of VTE[6]:
- Change in life style.
- Healthy diet[7].
- Exercise.
- Decreasing body weight.
- Avoiding smoking.
- Prevention of dehydration.
- Maintaining normal blood pressure.
Following recommendations are made for patients falling into other categories[6] :
- Patients at low risk for DVT:
- Graduated elastic compressions.
- Bedridden patients:
- Pneumatic compression.
- Patients in Critical Care Unit:
- Heparins (Heparin, lmwh, unfractionated Heparin)
- Warfarin.
- Direct thrombin inhibitors.
Treatment
See also
- Venous thromboembolism: Under-recognized and under-treated
- Deep vein thrombosis
- Pulmonary embolism
- Thrombosis
- Nephrotic syndrome and risk of venous and arterial thromboembolism
References
- ↑ Heit JA (2008). "The epidemiology of venous thromboembolism in the community". Arterioscler Thromb Vasc Biol. 28 (3): 370–2. doi:10.1161/ATVBAHA.108.162545. PMC 2873781. PMID 18296591.
- ↑ Prandoni P, Lensing AW, Cogo A, Cuppini S, Villalta S, Carta M; et al. (1996). "The long-term clinical course of acute deep venous thrombosis". Ann Intern Med. 125 (1): 1–7. PMID 8644983.
- ↑ Hippisley-Cox J, Coupland C (2011). "Development and validation of risk prediction algorithm (QThrombosis) to estimate future risk of venous thromboembolism: prospective cohort study". BMJ. 343: d4656. doi:10.1136/bmj.d4656. PMC 3156826. PMID 21846713. line feed character in
|title=at position 12 (help) - ↑ O'Brien JA, Caro JJ (2002). "Direct medical cost of managing deep vein thrombosis according to the occurrence of complications". Pharmacoeconomics. 20 (9): 603–15. PMID 12141888. Retrieved 2011-12-10.
- ↑ Amin A, Spyropoulos AC, Dobesh P, Shorr A, Hussein M, Mozaffari E, Benner JS (2010). "Are hospitals delivering appropriate VTE prevention? The venous thromboembolism study to assess the rate of thromboprophylaxis (VTE start)". J. Thromb. Thrombolysis. 29 (3): 326–39. doi:10.1007/s11239-009-0361-z. PMC 2837191. PMID 19548071. Retrieved 2011-12-10. Unknown parameter
|month=ignored (help) - ↑ 6.0 6.1 Goldhaber SZ (2004). "Prevention of recurrent idiopathic venous thromboembolism". Circulation. 110 (24 Suppl 1): IV20–4. doi:10.1161/01.CIR.0000150641.65000.f2. PMID 15598644. Retrieved 2011-12-10. Unknown parameter
|month=ignored (help) - ↑ Galson SK (2009). "Prevent deep vein thrombosis and pulmonary embolism with a healthful diet". J Am Diet Assoc. 109 (4): 592. doi:10.1016/j.jada.2009.02.020. PMID 19328250. Retrieved 2011-12-10. Unknown parameter
|month=ignored (help)