Uremic pericarditis: Difference between revisions
Varun Kumar (talk | contribs) |
Varun Kumar (talk | contribs) |
||
| Line 42: | Line 42: | ||
Patients may present with [[fever]], [[cachexia]] and varying levels of [[consciousness]]. | Patients may present with [[fever]], [[cachexia]] and varying levels of [[consciousness]]. | ||
'''Vitals:''' [[Hypotension]]and [[pulsus paradoxus]] are present in [[cardiac tamponade]]. The heart rate may be slow due to autonomic impairment or an [[arrhythmia]] such as atrial fibrillation, atrial flutter, heart block or a ventricular arrhythmia may be present due to an [[electrolyte]] imbalance. | '''Vitals:''' [[Hypotension]] and [[pulsus paradoxus]] are present in [[cardiac tamponade]]. The heart rate may be slow due to autonomic impairment or an [[arrhythmia]] such as atrial fibrillation, atrial flutter, heart block or a ventricular arrhythmia may be present due to an [[electrolyte]] imbalance. | ||
'''Neck:''' [[Jugular venous distension]] with a prominent Y descent and [[Kussmaul's sign]] | '''Neck:''' [[Jugular venous distension]] with a prominent Y descent and [[Kussmaul's sign]] | ||
| Line 51: | Line 51: | ||
'''Extremities:''' [[Ankle edema]] | '''Extremities:''' [[Ankle edema]] | ||
===Electrocardiogram=== | ===Electrocardiogram=== | ||
Revision as of 17:27, 30 June 2011
|
Pericarditis Microchapters |
|
Diagnosis |
|---|
|
Treatment |
|
Surgery |
|
Case Studies |
|
Uremic pericarditis On the Web |
|
American Roentgen Ray Society Images of Uremic pericarditis |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]; Associate Editor-In-Chief: Varun Kumar, M.B.B.S.
Overview
Renal failure can be associated with the development of a pericardial effusion and pericarditis, a condition known as uremic pericarditis. The underlying pathophysiology is not entirely clear, but it is hypothesized that uremic pericarditis is due to a build up of metabolic toxins such as urea, creatinine, methylguanidine which cause inflammation of pericardium. With the introduction of dialysis, the incidence of uremic pericarditis has dropped[1]. Uremic pericaritis can be further divided as:
- Uremic pericarditis in patients not undergoing dialysis.
- Uremic pericarditis in patients on maintenance dialysis.
Etiology
- Absence of dialysis in renal failure
- Inadequate dialysis in renal failure
- Volume overload during dialysis
- Infections
Pathophysiology
The pathophysiology of uremic pericarditis is not fully understood. However, there is a correlation observed with levels of blood urea nitrogen(usually >60 mg/dL) and creatinine. In renal failure, the absence or inadequate dialysis can lead to accumulation of these toxins in the body which may cause inflammation of pericardium and development of adhesions between the two pericardial layers. This could lead to loculation of effusion in pericardial cavity.
Patients undergoing dialysis may also develop pericarditis. In a series, 13% of patients undergoing hemodialysis developed pericarditis[2]
Uremic pericarditis can occur as a serous or a hemorrhagic effusion with considerable overlapping. Hemorrhagic effusions are more common secondary to uremia induced platelet dysfunction and the use of anticoagulation during hemodialysis.
Dialysis associated pericarditis may also be secondary to volume overload and bacterial or viral infections[3].
Presence of a large pericardial effusion that persists for >10 days after intensive dialysis has a high likelihood of development of cardiac tamponade
Diagnosis
History and symptoms
Patients may present with the following symptoms:
- Fever
- Chest pain that improves on leaning forward and worsens on inspiration
- Breathlessness
- Dizziness
- Malaise
- Ankle edema
Patients with uremic pericarditis may also present without any symptoms[4].
Physical examination
Patients may present with fever, cachexia and varying levels of consciousness.
Vitals: Hypotension and pulsus paradoxus are present in cardiac tamponade. The heart rate may be slow due to autonomic impairment or an arrhythmia such as atrial fibrillation, atrial flutter, heart block or a ventricular arrhythmia may be present due to an electrolyte imbalance.
Neck: Jugular venous distension with a prominent Y descent and Kussmaul's sign
Chest: Ewart's sign may be present. This includes a pericardial knock, pericardial rub(heard best while leaning forwards) and distant heart sounds
Abdomen: Hepatomegaly, ascites
Extremities: Ankle edema
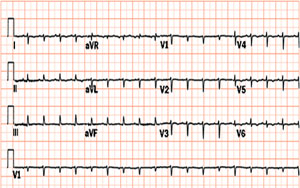
Electrocardiogram
Typical ECG changes of acute pericarditis such as ST and T wave elevations may not be seen in uremic pericarditis. This could be due to non-involvement of myocardium[3].
However, electrical alternans may be seen in presence of cardiac tamponade and other ECG changes related to electrolytes abnormalities due to poor renal function may be noted.
Chest X ray
Enlargement of cardiac shadow related to myocardial dysfunction, volume overload, or pericardial effusion may be observed on chest x-ray.

Echocardiography
Echocardiogram may show presence of fluid surrounding the heart in pericardial effusion. Loculated effusions secondary to adhesions in pericardial cavity may also be visualized as shown in the video below. Swinging motion of the heart may be seen in patients with cardiac tamponade.
Echocardiography of heart with loculated pericardial effusion compressing the left ventricle <youtube v=unnmmlCyyZM/>
Cardiac catheterization
In presence Cardiac tamponade, there is equalization of pressures in all four chambers of heart. The right atrial pressure equals the right ventricular end diastolic pressure equals the pulmonary artery diastolic pressure.
Treatment
- Patient with uremic pericarditis should be treated with intensive hemodialysis which would most often results in resolution of pericardial effusion and chest pain[5][6]within 1-2 weeks. Pericardiocentesis can be done to drain effusion if it is causing hemodynamic compromise such as in cardiac tamponade. Use of heparin free hemodialysis is adviced to prevent development of hemopericardium.
- Hypokalemia and hypophosphatemia should be prevented by supplementing the dialysis solution when appropriate[7].
- NSAIDs may be used in treatment of chest pain secondary to pericarditis. In case of recurrent pericardial effusion, pericardiotomy where a pericardial window for drainage of effusion may be made. In large refractory effusion, intra pericardial instillation of non-absorbable corticosteroids may be considered[8][2].
- Pericardiectomy should be done in refractory and severely symptomatic patients.
- Appropriate antivirals or antibiotics should be used in treatment of infective pericarditis which may occur in immunocompromised states resulting after renal transplantation[9].
References
- ↑ Bailey GL, Hampers CL, Hager EB, Merrill JP (1968). "Uremic pericarditis. Clinical features and management". Circulation. 38 (3): 582–91. PMID 5673609.
- ↑ 2.0 2.1 Rutsky EA, Rostand SG (1987). "Treatment of uremic pericarditis and pericardial effusion". Am J Kidney Dis. 10 (1): 2–8. PMID 3605080.
- ↑ 3.0 3.1 Gunukula SR, Spodick DH (2001). "Pericardial disease in renal patients". Semin Nephrol. 21 (1): 52–6. PMID 11172559.
- ↑ Banerjee A, Davenport A (2006). "Changing patterns of pericardial disease in patients with end-stage renal disease". Hemodial Int. 10 (3): 249–55. doi:10.1111/j.1542-4758.2006.00104.x. PMID 16805885.
- ↑ Maisch B, Seferović PM, Ristić AD, Erbel R, Rienmüller R, Adler Y; et al. (2004). "Guidelines on the diagnosis and management of pericardial diseases executive summary; The Task force on the diagnosis and management of pericardial diseases of the European society of cardiology". Eur Heart J. 25 (7): 587–610. doi:10.1016/j.ehj.2004.02.002. PMID 15120056.
- ↑ Maisch B, Ristić AD (2003). "Practical aspects of the management of pericardial disease". Heart. 89 (9): 1096–103. PMC 1767862. PMID 12923044.
- ↑ Emelife-Obi C, Chow MT, Qamar-Rohail H, Leehey DJ, Gandhi VC, Ing TS (1998). "Use of a phosphorus-enriched hemodialysate to prevent hypophosphatemia in a patient with renal failure-related pericarditis". Clin Nephrol. 50 (2): 131–3. PMID 9725787.
- ↑ Wood JE, Mahnensmith RL (2001). "Pericarditis associated with renal failure: evolution and management". Semin Dial. 14 (1): 61–6. PMID 11208042.
- ↑ Sever MS, Steinmuller DR, Hayes JM, Streem SB, Novick AC (1991). "Pericarditis following renal transplantation". Transplantation. 51 (6): 1229–32. PMID 1646505.