Tricuspid atresia surgery: Difference between revisions
| (36 intermediate revisions by 6 users not shown) | |||
| Line 1: | Line 1: | ||
__NOTOC__ | __NOTOC__ | ||
{{Template:Tricuspid atresia}} | {{Template:Tricuspid atresia}} | ||
{{CMG}}; '''Associate Editor-In-Chief:''' [[User:KeriShafer|Keri Shafer, M.D.]] [mailto:kshafer@bidmc.harvard.edu] [[Priyamvada Singh|Priyamvada Singh, MBBS]] | {{CMG}}; '''Associate Editor-In-Chief:''' {{Sara.Zand}} [[User:KeriShafer|Keri Shafer, M.D.]] [mailto:kshafer@bidmc.harvard.edu] [[Priyamvada Singh|Priyamvada Singh, MBBS]] [mailto:psingh13579@gmail.com]; '''Assistant Editor-In-Chief:''' [[Kristin Feeney|Kristin Feeney, B.S.]] [mailto:kfeeney@elon.edu] | ||
==Overview== | ==Overview== | ||
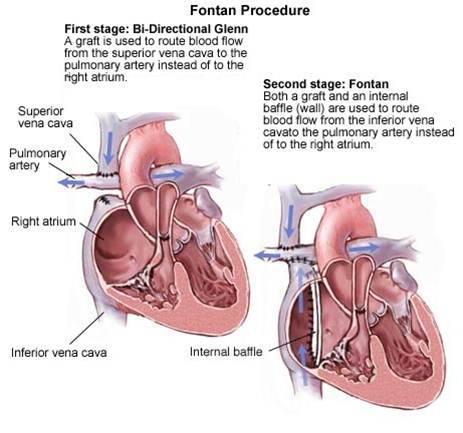
[[Surgery]] is the mainstay of therapy for [[tricuspid atresia]]. In the first 8 weeks of life if there are severe [[ Cyanosis]] and [[pulmonary obstruction]] and normal positioning [[ aorta]] and [[ pulmonary artery]], making a [[shunt]] between systemic [[subclavian artery]] to the [[ pulmonary artery ]]is necessary which is called [[Blalock -Taussig]] [[(BT shunt)]]. If the [[pulmonary artery]] comes from the [[left ventricle]] and is overflowed, [[pulmonary artery]] banding is useful for lowering the [[pulmonary blood flow]]. In older children, [[bi-direction Glenn shunt]] which is the connection between [[superior vena cava]] to the [[ pulmonary artery]] is planned for transferring the blood to the pulmonary system. [[Fontan]] procedure is a conduit between the [[ inferior vena cava]] and the [[ pulmonary artery]] whether transfers the systemic venous blood to [[pulmonary circulation at the age of 2-3 years old. | |||
==Surgery== | ==Surgery== | ||
* [[Surgery]] is the mainstay of therapy for [[tricuspid atresia]]. | |||
** In the first 8 weeks of life if there are severe [[ Cyanosis]] and [[pulmonary obstruction]] and normal positioning [[ aorta]] and [[ pulmonary artery]], making a [[shunt]] between systemic [[subclavian artery]] to the [[ pulmonary artery ]]is necessary which is called [[Blalock -Taussig]] [[(BT shunt)]].<ref name="pmid26260095">{{cite journal |vauthors=Aykanat A, Yavuz T, Özalkaya E, Topçuoğlu S, Ovalı F, Karatekin G |title=Long-Term Prostaglandin E1 Infusion for Newborns with Critical Congenital Heart Disease |journal=Pediatr Cardiol |volume=37 |issue=1 |pages=131–4 |date=January 2016 |pmid=26260095 |doi=10.1007/s00246-015-1251-0 |url=}}</ref> | |||
** If the [[pulmonary artery]] comes from the [[left ventricle]] and is overflowed, [[pulmonary artery]] banding is useful for lowering the [[pulmonary blood flow]].<ref name="pmid30811802">{{cite journal |vauthors=Boucek DM, Qureshi AM, Goldstein BH, Petit CJ, Glatz AC |title=Blalock-Taussig shunt versus patent ductus arteriosus stent as first palliation for ductal-dependent pulmonary circulation lesions: A review of the literature |journal=Congenit Heart Dis |volume=14 |issue=1 |pages=105–109 |date=January 2019 |pmid=30811802 |doi=10.1111/chd.12707 |url=}}</ref> | |||
** In older children, [[bi-direction Glenn shunt]] which is the connection between [[superior vena cava]] to the [[ pulmonary artery]] is planned for transferring the blood to the pulmonary system. | |||
**[[Fontan]] procedure is a conduit between the [[ inferior vena cava]] and the [[ pulmonary artery]] whether transfers the systemic venous blood to [[pulmonary circulation at the age of 2-3 years old.<ref name="pmid8238751">{{cite journal |vauthors=Norwood WI, Jacobs ML |title=Fontan's procedure in two stages |journal=Am. J. Surg. |volume=166 |issue=5 |pages=548–51 |date=November 1993 |pmid=8238751 |doi=10.1016/s0002-9610(05)81151-1 |url=}}</ref> | |||
**[[Endocarditis]] prophylaxis before every procedure is recommended. | |||
[[Image:TA_Fontan_procedure.jpg|left|450px]] | |||
<br clear="left"/> | |||
==References== | ==References== | ||
| Line 85: | Line 37: | ||
[[Category:Pediatrics]] | [[Category:Pediatrics]] | ||
[[Category:Disease]] | [[Category:Disease]] | ||
[[Category:Needs overview]] | |||
[[Category:Cardiovascular diseases]] | |||
[[Category:Up-To-Date cardiology]] | |||
[[Category:Up-To-Date]] | |||
{{WH}} | {{WH}} | ||
{{WS}} | {{WS}} | ||
Latest revision as of 19:42, 8 November 2020
|
Tricuspid atresia Microchapters |
|
Diagnosis |
|---|
|
Treatment |
|
Special Scenarios |
|
Case Studies |
|
Tricuspid atresia surgery On the Web |
|
American Roentgen Ray Society Images of Tricuspid atresia surgery |
|
Risk calculators and risk factors for Tricuspid atresia surgery |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]; Associate Editor-In-Chief: Sara Zand, M.D.[2] Keri Shafer, M.D. [3] Priyamvada Singh, MBBS [4]; Assistant Editor-In-Chief: Kristin Feeney, B.S. [5]
Overview
Surgery is the mainstay of therapy for tricuspid atresia. In the first 8 weeks of life if there are severe Cyanosis and pulmonary obstruction and normal positioning aorta and pulmonary artery, making a shunt between systemic subclavian artery to the pulmonary artery is necessary which is called Blalock -Taussig (BT shunt). If the pulmonary artery comes from the left ventricle and is overflowed, pulmonary artery banding is useful for lowering the pulmonary blood flow. In older children, bi-direction Glenn shunt which is the connection between superior vena cava to the pulmonary artery is planned for transferring the blood to the pulmonary system. Fontan procedure is a conduit between the inferior vena cava and the pulmonary artery whether transfers the systemic venous blood to [[pulmonary circulation at the age of 2-3 years old.
Surgery
- Surgery is the mainstay of therapy for tricuspid atresia.
- In the first 8 weeks of life if there are severe Cyanosis and pulmonary obstruction and normal positioning aorta and pulmonary artery, making a shunt between systemic subclavian artery to the pulmonary artery is necessary which is called Blalock -Taussig (BT shunt).[1]
- If the pulmonary artery comes from the left ventricle and is overflowed, pulmonary artery banding is useful for lowering the pulmonary blood flow.[2]
- In older children, bi-direction Glenn shunt which is the connection between superior vena cava to the pulmonary artery is planned for transferring the blood to the pulmonary system.
- Fontan procedure is a conduit between the inferior vena cava and the pulmonary artery whether transfers the systemic venous blood to [[pulmonary circulation at the age of 2-3 years old.[3]
- Endocarditis prophylaxis before every procedure is recommended.
References
- ↑ Aykanat A, Yavuz T, Özalkaya E, Topçuoğlu S, Ovalı F, Karatekin G (January 2016). "Long-Term Prostaglandin E1 Infusion for Newborns with Critical Congenital Heart Disease". Pediatr Cardiol. 37 (1): 131–4. doi:10.1007/s00246-015-1251-0. PMID 26260095.
- ↑ Boucek DM, Qureshi AM, Goldstein BH, Petit CJ, Glatz AC (January 2019). "Blalock-Taussig shunt versus patent ductus arteriosus stent as first palliation for ductal-dependent pulmonary circulation lesions: A review of the literature". Congenit Heart Dis. 14 (1): 105–109. doi:10.1111/chd.12707. PMID 30811802.
- ↑ Norwood WI, Jacobs ML (November 1993). "Fontan's procedure in two stages". Am. J. Surg. 166 (5): 548–51. doi:10.1016/s0002-9610(05)81151-1. PMID 8238751.