Tension pneumothorax resident survival guide
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]
Overview
Tension pneumothorax is a medical emergency caused by accumulation of air in the pleural cavity. Air enter the intrapleural space through the lung parenchyma, or through a traumatic communication from the chest wall.
Causes
Life Threatening Causes
Life-threatening causes include conditions which may result in death or permanent disability within 24 hours if left untreated. Tension pneumothorax is a life-threatening condition and must be treated as such irrespective of the underlying causes.
Common Causes
- Mechanical ventilation
- Trauma
- Central venous catheter
- Cardiopulmonary resuscitation
- Emphysema
- Chronic obstructive pulmonary disease
- Asthma
Management
Shown below is an algorithm depicting the management of tension pneumothorax.[1]
Characterize the symptoms:[1] ❑ Breathlessness | |||||||||||||||||||||||||||||||||||||
Examine the patient: Vital signs ❑ Respiratory rate:
❑ Heart rate: ❑ Blood pressure Focused chest examination[1] Inspection ❑ Reduced lung expansion on the affected side Palpation ❑ Trachea shifted to the opposite side Percussion Auscultation ❑ Diminished breath sounds on the affected side | |||||||||||||||||||||||||||||||||||||
Manage the patient with a multidisciplinary team: ❑ Consult a thoracic surgeon ❑ Consult a cardiologist | |||||||||||||||||||||||||||||||||||||
Consider other diseases with similar presentations: ❑ Acute myocardial infarction ❑ Pericardial tamponade ❑ Emphysema | |||||||||||||||||||||||||||||||||||||
| Categorize the Patient | |||||||||||||||||||||||||||||||||||||
| Hemodynamically Stable | Hemodynamically Unstable | ||||||||||||||||||||||||||||||||||||
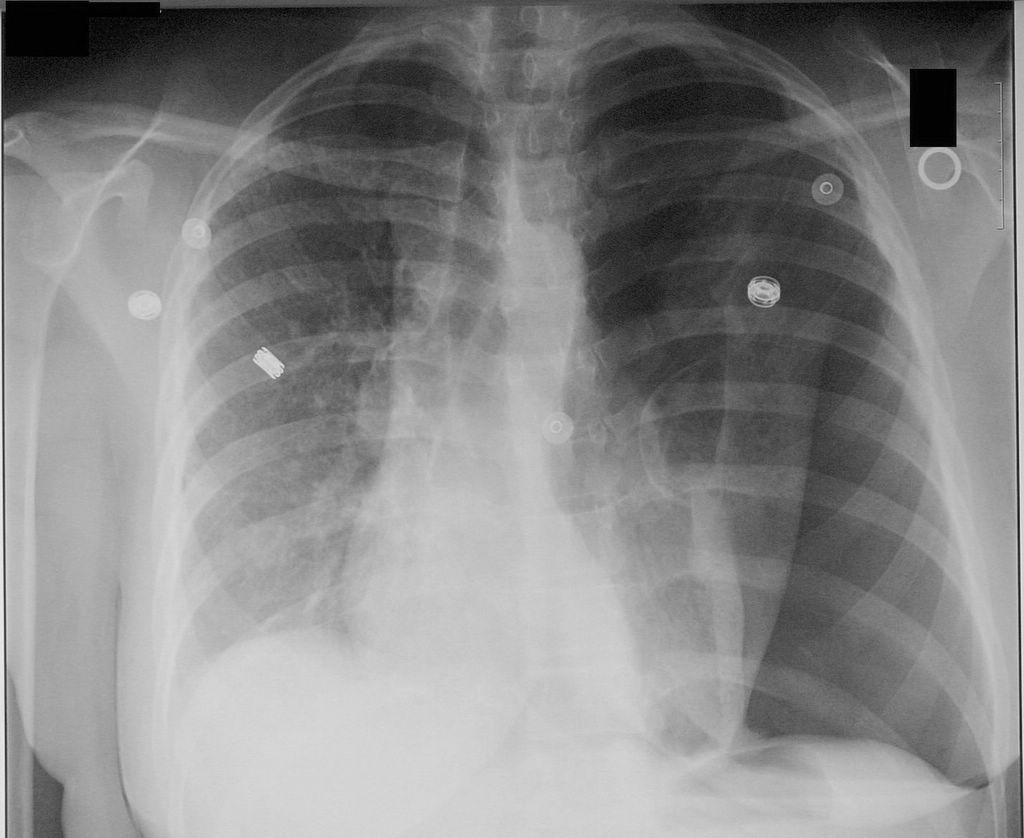
Confirm diagnosis Imaging studies
❑ Chest CT scanning
| Emergency needle decompression ❑ Aseptic preparation
❑ Use 14-16 G intravenous cannula
Antibiotic therapy | ||||||||||||||||||||||||||||||||||||
| Aspirate using 14-16 G cannula | Admit the patient | ||||||||||||||||||||||||||||||||||||
Insert chest drain ❑ Site: the triangle of safety bordered by
❑ Requirments
❑ Equipment required
| |||||||||||||||||||||||||||||||||||||
❑ Pleural space size < 2cm | ❑ Pleural space size > 2cm | ||||||||||||||||||||||||||||||||||||
| Follow Up | Chest drain | ||||||||||||||||||||||||||||||||||||
Do`s
- Tension pneumothorax diagnosis should be made based on the history and physical examination findings.
- Serial chest radiographs every 6 hrs on the first day after injury to rule out pneumothorax is ideal.[2]
- Leave the cannula in place until bubbling is confirmed in the chest drain underwater seal system
- Suspect tension pneumothorax with blunt and penetrating trauma to the chest
- Differentiate tension pneumothorax from pericardial tamponade, and myocardial infarction.
- Suspect tension pneumothorax in patients on mechanical ventilations, who have a rapid onset of hemodynamic instability or cardiac arrest, and require increasing peak inspiratory pressures.
- Check chest tubes, as they can become plugged or malpositioned and stop functioning.
- Give adequate analgesia to patients before chest tube insertion, as the procedure is extremely painful.
- Refer the patient to respiratory specialist within 24h of admission.
Dont`s
- Don`t start using chest radiograph or CT scan unless in doubt regarding the diagnosis and when the patient's clinical condition is sufficiently stable.
- Don`t use large bore chest drains.[1]
- Don`t repeat needle aspiration unless there were technical difficulties.
References
- ↑ 1.0 1.1 1.2 1.3 1.4 MacDuff A, Arnold A, Harvey J, BTS Pleural Disease Guideline Group (2010). "Management of spontaneous pneumothorax: British Thoracic Society Pleural Disease Guideline 2010". Thorax. 65 Suppl 2: ii18–31. doi:10.1136/thx.2010.136986. PMID 20696690.
- ↑ 2.0 2.1 Sharma A, Jindal P (2008). "Principles of diagnosis and management of traumatic pneumothorax". J Emerg Trauma Shock. 1 (1): 34–41. doi:10.4103/0974-2700.41789. PMC 2700561. PMID 19561940.