Tension pneumothorax resident survival guide
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]; Associate Editor(s)-in-Chief: Hamid Qazi, MD, BSc [2], Mohamed Moubarak, M.D. [3], Twinkle Singh, M.B.B.S. [4], Rim Halaby, M.D. [5]
| Tension Pneumothorax Resident Survival Guide Microchapters |
|---|
| Overview |
| Causes |
| FIRE |
| Diagnosis |
| Treatment |
| Do's |
| Don'ts |
Overview
Tension pneumothorax is a life threatening condition that results from the accumulation of air in the pleural cavity. Air enters the intrapleural space through an injured parietal pleura, visceral pleura or tracheobronchial tree that forms a one way valve. The one way valve allows the air to enter in the pleural cavity (during inspiration) but prevents its escape (during expiration). Subsequently, the intrapleural pressure rises and results in respiratory and cardiovascular failure. Tension pneumothorax can occur as a result of trauma, ventilation or resuscitation.[1] The cardinal symptoms and signs of tension pneumothorax are severe dyspnea, chest pain, hypotension, hypoxia, tachycardia and jugular vein distention. Tension pneumothorax should be managed immediately with emergency needle decompression followed by insertion of a chest tube.
Causes
Life Threatening Causes
Tension pneumothorax is a life-threatening condition and must be treated as such irrespective of the underlying cause.
Common Causes
- Asthma
- Central venous catheter
- Cardiopulmonary resuscitation
- Chronic obstructive pulmonary disease
- Emphysema
- Mechanical ventilation
- Trauma[1]
Click here for the complete list of causes.
FIRE: Focused Initial Rapid Evaluation
A Focused Initial Rapid Evaluation (FIRE) as shown below should be performed to identify patients in need of immediate intervention.
Boxes in red signify that an urgent management is needed.
Identify cardinal findings that increase the pretest probability of tension pneumothorax: ❑ Chest pain ❑ Dyspnea ❑ Hypoxia ❑ Hypotension ❑ Tachycardia ❑ Jugular venous distension ❑ Absent breath sounds on the affected side | |||||||||||||||||||||||||||||
Does the patient have high probability of tension pneumothorax? | |||||||||||||||||||||||||||||
Yes | No | ||||||||||||||||||||||||||||
❑ Immediately insert a 14-16 Gauge needle in the 2nd intercostal space at the midclavicular line of the affected hemithorax | |||||||||||||||||||||||||||||
❑ Insert chest drain immediately after needle decompression | |||||||||||||||||||||||||||||
Complete Diagnostic Approach
A complete diagnostic approach should be carried out after a focused initial rapid evaluation is conducted and following initiation of any urgent intervention.[1]
Characterize the symptoms: ❑ Dyspnea | |||||||||||||||||||||||||||
Identify the precipitating factors: ❑ Recent invasive procedures ❑ Mechanical ventilation | |||||||||||||||||||||||||||
Examine the patient: Appearance of the patient Vital signs ❑ Tachycardia Skin ❑ Cyanosis Neck ❑ Jugular venous distension (absent in severe hypotension) Respiratory examination Inspection Additional findings in ventilated patients ❑ Decreased oxygen saturation | |||||||||||||||||||||||||||
Consider alternative diagnosis:
| |||||||||||||||||||||||||||
| ❑ High probability of tension pneumothorax | ❑ Low probability of tension pneumothorax and patient is hemodynamically stable | ||||||||||||||||||||||||||
| ❑ Proceed with immediate needle decompression | |||||||||||||||||||||||||||
Order imaging studies: ❑ Order chest X-ray looking for:
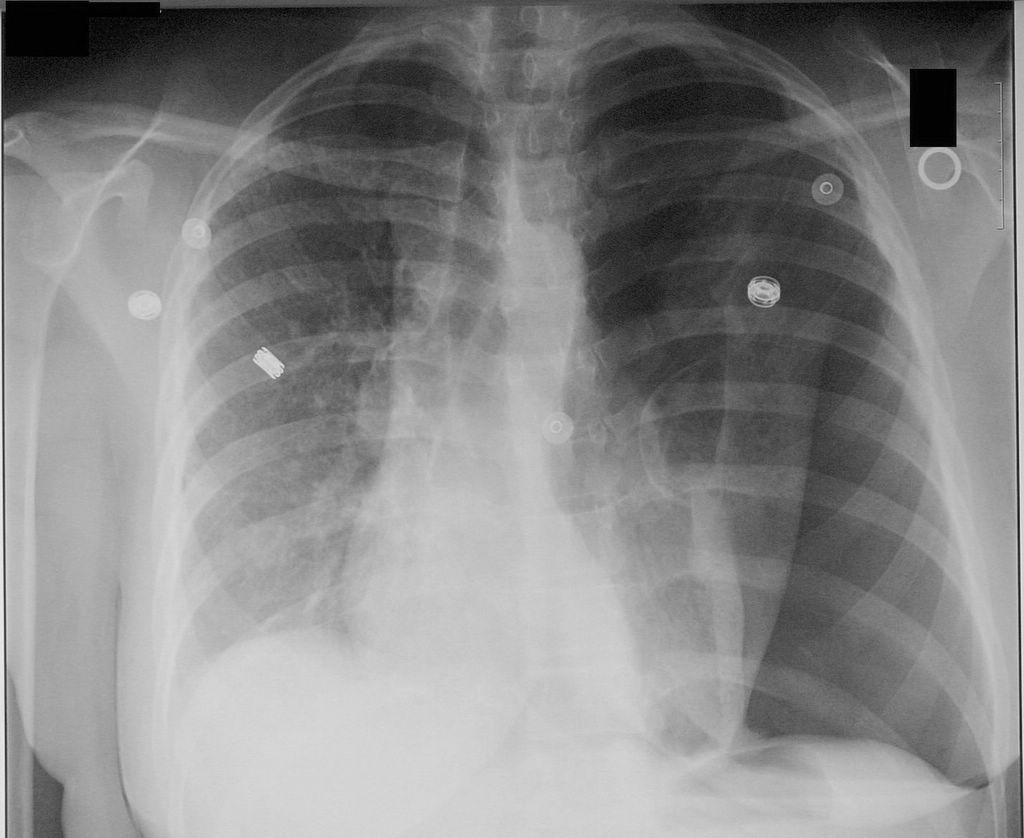
Shown below is an image of a chest X-ray depicting tension pneumothorax in the left lung. | |||||||||||||||||||||||||||
Treatment
Perform emergency needle decompression:[1] ❑ Wear a gown, face mask and eye shield
❑ Insert a 14-16 gauge needle with a catheter at a 90° angle | |||||||||||||||||||||||||||||||||||||
Insert a chest tube (tube thoracostomy) immediately after needle decompression: ❑ Make sure that the following equipments are available:
❑ Administer adequate analgesics | |||||||||||||||||||||||||||||||||||||
Follow up: ❑ Refer the patient to a respiratory physician if pneumothorax does not respond within 48 hours | |||||||||||||||||||||||||||||||||||||
Do's
- Suspect tension pneumothorax in the case of blunt and penetrating trauma to the chest.
- Immediately cover penetrating chest wounds with an occlusive or pressure bandage in trauma patients with suspected tension pneumothorax.
- Suspect tension pneumothorax among patients on mechanical ventilation who develop a rapid onset of hemodynamic instability or cardiac arrest and require an increase in the peak inspiratory pressure.
- Order serial chest radiographs every 6 hours on the first day following chest trauma to rule out pneumothorax.[2]
- Refer the patient to a respiratory specialist within 24 hours of admission.
- Order a chest X-ray before chest tube removal to confirm the re-expansion of the affected lung.
Don'ts
- Don't remove the catheter from the 2nd intercostal space unless a chest tube is appropriately placed.
- Don't use large bore chest tubes.[1]
- Don't leave the chest tube more than 7 days, as it will increase the risk of infection.
References
- ↑ 1.0 1.1 1.2 1.3 1.4 1.5 1.6 MacDuff A, Arnold A, Harvey J, BTS Pleural Disease Guideline Group (2010). "Management of spontaneous pneumothorax: British Thoracic Society Pleural Disease Guideline 2010". Thorax. 65 Suppl 2: ii18–31. doi:10.1136/thx.2010.136986. PMID 20696690.
- ↑ 2.0 2.1 Sharma A, Jindal P (2008). "Principles of diagnosis and management of traumatic pneumothorax". J Emerg Trauma Shock. 1 (1): 34–41. doi:10.4103/0974-2700.41789. PMC 2700561. PMID 19561940.
<headertabs />