Systemic lupus erythematosus MRI: Difference between revisions
| Line 21: | Line 21: | ||
** T2: nonspecific, increased periportal [[edema]] | ** T2: nonspecific, increased periportal [[edema]] | ||
| | | | ||
[[File:9763697dab2e8388d7a54b513a3e42 jumbo.jpg|thumb|300px|<SMALL><SMALL>''[https://radiopaedia.org/ | [[File:9763697dab2e8388d7a54b513a3e42 jumbo.jpg|thumb|300px|<SMALL><SMALL>''[https://radiopaedia.org/ Adapted from Radiopaedia]''</SMALL></SMALL>]] | ||
[[File:9531e159d25c6beef968d6c1caf46c jumbo.jpg|thumb|300px|<SMALL><SMALL>''[https://radiopaedia.org/ | [[File:9531e159d25c6beef968d6c1caf46c jumbo.jpg|thumb|300px|<SMALL><SMALL>''[https://radiopaedia.org/ Adapted from Radiopaedia]''</SMALL></SMALL>]] | ||
|- | |- | ||
![[Cholecystitis]] | ![[Cholecystitis]] | ||
| Line 30: | Line 30: | ||
* [[Gallbladder|Gall bladder]] wall thickening | * [[Gallbladder|Gall bladder]] wall thickening | ||
| | | | ||
[[File:Acute-cholecystitis-3.jpg|thumb|300px|<SMALL><SMALL>''[https://radiopaedia.org/ | [[File:Acute-cholecystitis-3.jpg|thumb|300px|<SMALL><SMALL>''[https://radiopaedia.org/ Adapted from Radiopaedia]''</SMALL></SMALL>]] | ||
|- | |- | ||
![[Acute pancreatitis|Pancreatitis]] | ![[Acute pancreatitis|Pancreatitis]] | ||
| Line 41: | Line 41: | ||
**** Circumscribed fluid collection | **** Circumscribed fluid collection | ||
| | | | ||
[[File:C13ada80fec4008d775777547a65ef big gallery.jpg|thumb|300px|<SMALL><SMALL>''[https://radiopaedia.org/ | [[File:C13ada80fec4008d775777547a65ef big gallery.jpg|thumb|300px|<SMALL><SMALL>''[https://radiopaedia.org/ Adapted from Radiopaedia]''</SMALL></SMALL>]] | ||
|- | |- | ||
![[Mesenteric vascular occlusion|Mesenteric vasculitis]] | ![[Mesenteric vascular occlusion|Mesenteric vasculitis]] | ||
| Line 61: | Line 61: | ||
* The normal [[pericardial]] thickness is considered 2 mm while a thickness of over 4 mm suggests a [[pericarditis]] | * The normal [[pericardial]] thickness is considered 2 mm while a thickness of over 4 mm suggests a [[pericarditis]] | ||
| | | | ||
[[File:59f9b477529f76aad3615898fb5d6f big gallery.jpg|thumb|300px|<SMALL><SMALL>''[https://radiopaedia.org/ | [[File:59f9b477529f76aad3615898fb5d6f big gallery.jpg|thumb|300px|<SMALL><SMALL>''[https://radiopaedia.org/ Adapted from Radiopaedia]''</SMALL></SMALL>]] | ||
|- | |- | ||
![[Pericardial effusion]] | ![[Pericardial effusion]] | ||
| Line 74: | Line 74: | ||
** Early postcontrast enhancement due to regional vasodilatation and increased blood volume, secondary to the [[inflammation]] | ** Early postcontrast enhancement due to regional vasodilatation and increased blood volume, secondary to the [[inflammation]] | ||
| | | | ||
[[File:Lymphocytic-myocarditis.jpg|thumb|300px|<SMALL><SMALL>''[https://radiopaedia.org/ | [[File:Lymphocytic-myocarditis.jpg|thumb|300px|<SMALL><SMALL>''[https://radiopaedia.org/ Adapted from Radiopaedia]''</SMALL></SMALL>]] | ||
|- | |- | ||
| rowspan="4" style="background: #DCDCDC; " |<small><small>[[Neurological ]]</small></small> | | rowspan="4" style="background: #DCDCDC; " |<small><small>[[Neurological ]]</small></small> | ||
!General | !General | ||
| | | | ||
* [[White matter]] [[lesions]] | * [[White matter]] [[lesions]] | ||
* [[Periventricular nucleus|Periventricular]] hyperintensities | * [[Periventricular nucleus|Periventricular]] hyperintensities | ||
* Detects clinically silent [[Lesion|lesions]] | * Detects clinically silent [[Lesion|lesions]] | ||
| | | | ||
[[File:Ec9e2a6a4c1d377bdee5f0ccbbf180 big gallery.jpg|thumb|300px|<SMALL><SMALL>''[https://radiopaedia.org/ | [[File:Ec9e2a6a4c1d377bdee5f0ccbbf180 big gallery.jpg|thumb|300px|<SMALL><SMALL>''[https://radiopaedia.org/ Adapted from Radiopaedia]''</SMALL></SMALL>]] | ||
|- | |- | ||
![[Stroke]] | ![[Stroke]] | ||
| Line 93: | Line 92: | ||
* High T2 signal after 6 hours of [[stroke]] | * High T2 signal after 6 hours of [[stroke]] | ||
| | | | ||
[[File:Subacute-middle-cerebral-artery-infarct.jpg|thumb|300px|<SMALL><SMALL>''[https://radiopaedia.org/ | [[File:Subacute-middle-cerebral-artery-infarct.jpg|thumb|300px|<SMALL><SMALL>''[https://radiopaedia.org/ Adapted from Radiopaedia]''</SMALL></SMALL>]] | ||
|- | |- | ||
![[Neuropathies]] | ![[Neuropathies]] | ||
| Line 104: | Line 103: | ||
*** Contrast enhancement of the [[nerve]], best seen with fat-suppressed T1 coronal images | *** Contrast enhancement of the [[nerve]], best seen with fat-suppressed T1 coronal images | ||
| | | | ||
[[File:D1797f6a1a111e62b0f9ba00fc93bb big gallery.jpg|thumb|300px|<SMALL><SMALL>''[https://radiopaedia.org/ | [[File:D1797f6a1a111e62b0f9ba00fc93bb big gallery.jpg|thumb|300px|<SMALL><SMALL>''[https://radiopaedia.org/ Adapted from Radiopaedia]''</SMALL></SMALL>]] | ||
[[File:Myelitis.jpg|thumb|300px|<SMALL><SMALL>''[https://radiopaedia.org/ | [[File:Myelitis.jpg|thumb|300px|<SMALL><SMALL>''[https://radiopaedia.org/ Adapted from Radiopaedia]''</SMALL></SMALL>]] | ||
|- | |- | ||
![[Encephalitis|Autoimmune encephalitis]] | ![[Encephalitis|Autoimmune encephalitis]] | ||
| Line 116: | Line 115: | ||
* Patchy areas of enhancement | * Patchy areas of enhancement | ||
| | | | ||
[[File:11b6d7d362d132027d14f5a6a12236 big gallery.jpg|thumb|300px|<SMALL><SMALL>''[https://radiopaedia.org/ | [[File:11b6d7d362d132027d14f5a6a12236 big gallery.jpg|thumb|300px|<SMALL><SMALL>''[https://radiopaedia.org/ Adapted from Radiopaedia]''</SMALL></SMALL>]] | ||
|- | |- | ||
| rowspan="4" style="background: #DCDCDC; " |<small><small>[[Musculoskeletal]]</small></small> | | rowspan="4" style="background: #DCDCDC; " |<small><small>[[Musculoskeletal]]</small></small> | ||
| Line 125: | Line 124: | ||
** Tapering of digital [[vessels]] | ** Tapering of digital [[vessels]] | ||
| | | | ||
[[File:Secondary-raynauds-phenomenon.jpg|thumb|300px|<SMALL><SMALL>''[https://radiopaedia.org/ | [[File:Secondary-raynauds-phenomenon.jpg|thumb|300px|<SMALL><SMALL>''[https://radiopaedia.org/ Adapted from Radiopaedia]''</SMALL></SMALL>]] | ||
|- | |- | ||
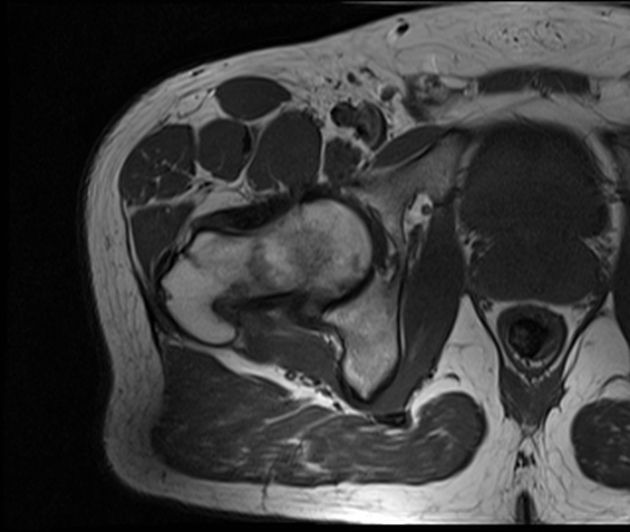
![[Myositis]] | ![[Myositis]] | ||
| Line 131: | Line 130: | ||
* [[Edema|Intramuscular edema]] (increased high T2 signal) | * [[Edema|Intramuscular edema]] (increased high T2 signal) | ||
| | | | ||
[[File:11f542413e3f946e7401ba6184820f big gallery.jpg|thumb|300px|<SMALL><SMALL>''[https://radiopaedia.org/ | [[File:11f542413e3f946e7401ba6184820f big gallery.jpg|thumb|300px|<SMALL><SMALL>''[https://radiopaedia.org/ Adapted from Radiopaedia]''</SMALL></SMALL>]] | ||
|- | |- | ||
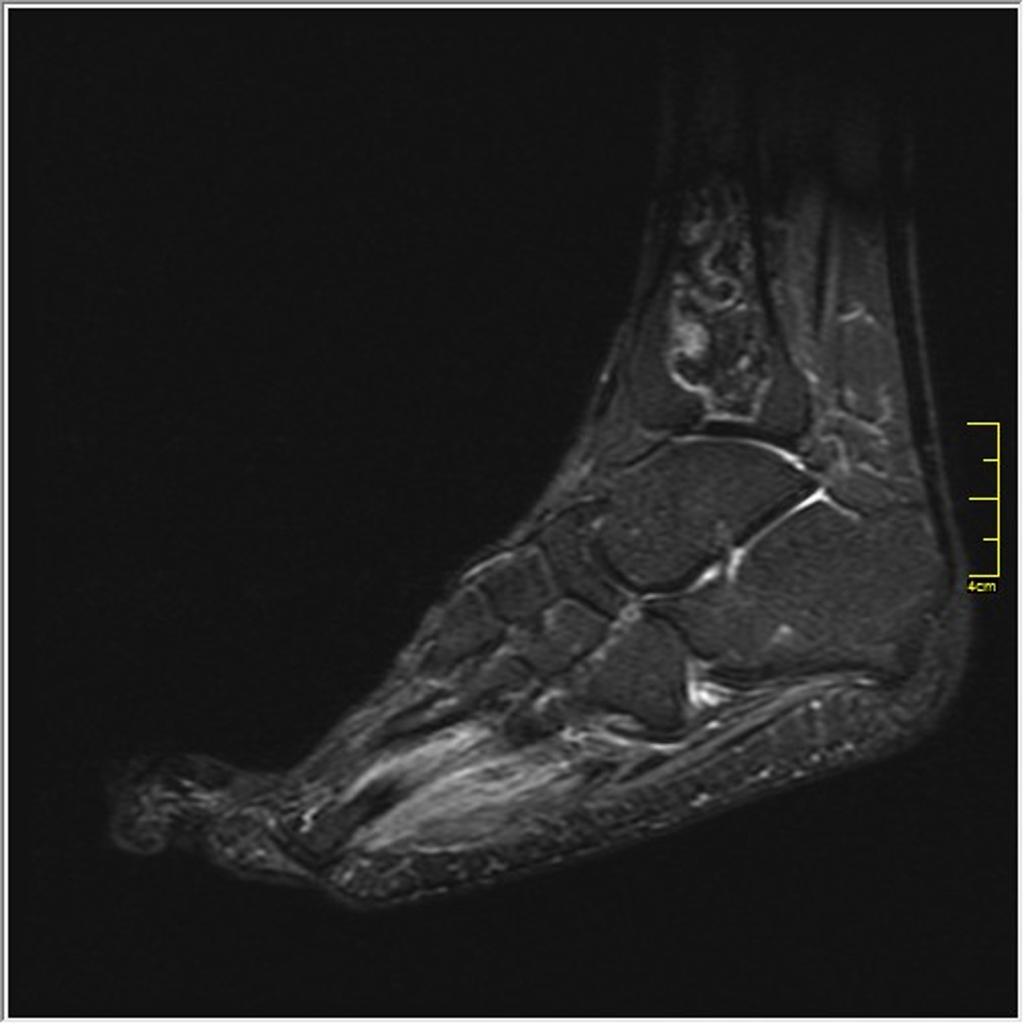
![[Arthritis]]/[[tenosynovitis]] | ![[Arthritis]]/[[tenosynovitis]] | ||
| Line 139: | Line 138: | ||
* [[Synovial]] overgrowth | * [[Synovial]] overgrowth | ||
| | | | ||
[[File:A87cc2247174b9aad66f9bfe89bb1c big gallery.jpg|thumb|300px|<SMALL><SMALL>''[https://radiopaedia.org/ | [[File:A87cc2247174b9aad66f9bfe89bb1c big gallery.jpg|thumb|300px|<SMALL><SMALL>''[https://radiopaedia.org/ Adapted from Radiopaedia]''</SMALL></SMALL>]] | ||
|- | |- | ||
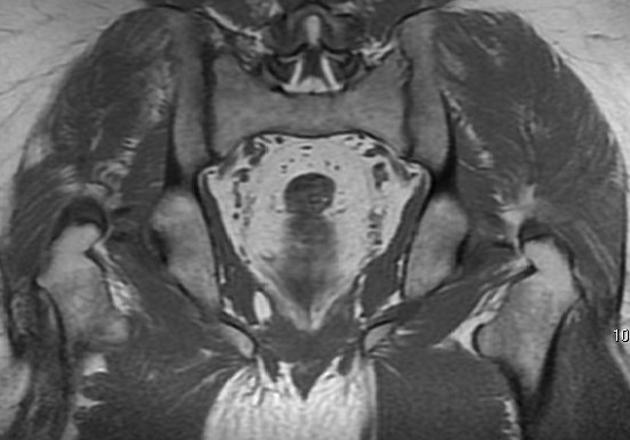
![[Osteonecrosis]] ([[Avascular necrosis]]) | ![[Osteonecrosis]] ([[Avascular necrosis]]) | ||
| Line 153: | Line 152: | ||
** In characteristic stress locations insufficiency fractures may appear as areas of high signal intensity due to [[bone marrow]] edema | ** In characteristic stress locations insufficiency fractures may appear as areas of high signal intensity due to [[bone marrow]] edema | ||
| | | | ||
[[File:Medullary-bone-infarct-lupus-on-corticosteroids.JPG|thumb|300px|<SMALL><SMALL>''[https://radiopaedia.org/ | [[File:Medullary-bone-infarct-lupus-on-corticosteroids.JPG|thumb|300px|<SMALL><SMALL>''[https://radiopaedia.org/ Adapted from Radiopaedia]''</SMALL></SMALL>]] | ||
[[File:Osteoprosis mri.jpg|thumb|300px|<SMALL><SMALL>''[https://radiopaedia.org/ | [[File:Osteoprosis mri.jpg|thumb|300px|<SMALL><SMALL>''[https://radiopaedia.org/ Adapted from Radiopaedia]''</SMALL></SMALL>]] | ||
|} | |} | ||
Revision as of 15:44, 4 August 2017
|
Systemic lupus erythematosus Microchapters |
|
Differentiating Systemic lupus erythematosus from other Diseases |
|---|
|
Diagnosis |
|
Treatment |
|
Case Studies |
|
Systemic lupus erythematosus MRI On the Web |
|
American Roentgen Ray Society Images of Systemic lupus erythematosus MRI |
|
Directions to Hospitals Treating Systemic lupus erythematosus |
|
Risk calculators and risk factors for Systemic lupus erythematosus MRI |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]
Overview
On abdominal MRI, systemic lupus erythematosus (SLE) may be characterized by hepatomegaly, pancreatic parenchymal enlargement, and hypervascularity of mesentery. On cardiac MRI, SLE may be characterized by mitral leaflet thickening, pericardial thickness, and pericardial effusions. On brain MRI, SLE may be characterized by white matter lesions, changes in blood circulation of the brain, and patchy areas of enhancement. On musculoskeletal MRI, SLE may be characterized by intramuscular edema, proliferative tenosynovitis, and bone marrow edema.
Key MRI findings in systemic lupus erythematosus
Most of SLEs complications can be visualized with other, more feasible imaging techniques, so MRI is not the imaging modality of choice for the diagnosis of most complications of SLE. However, if it is done, the following changes can be found in different organ systems of the body:[1][2][3][4][5][6][7][8][9][10][11]
| Organ involvement | Disease | MRI | Preview |
|---|---|---|---|
| Gastrointestinal | Hepatitis |
|
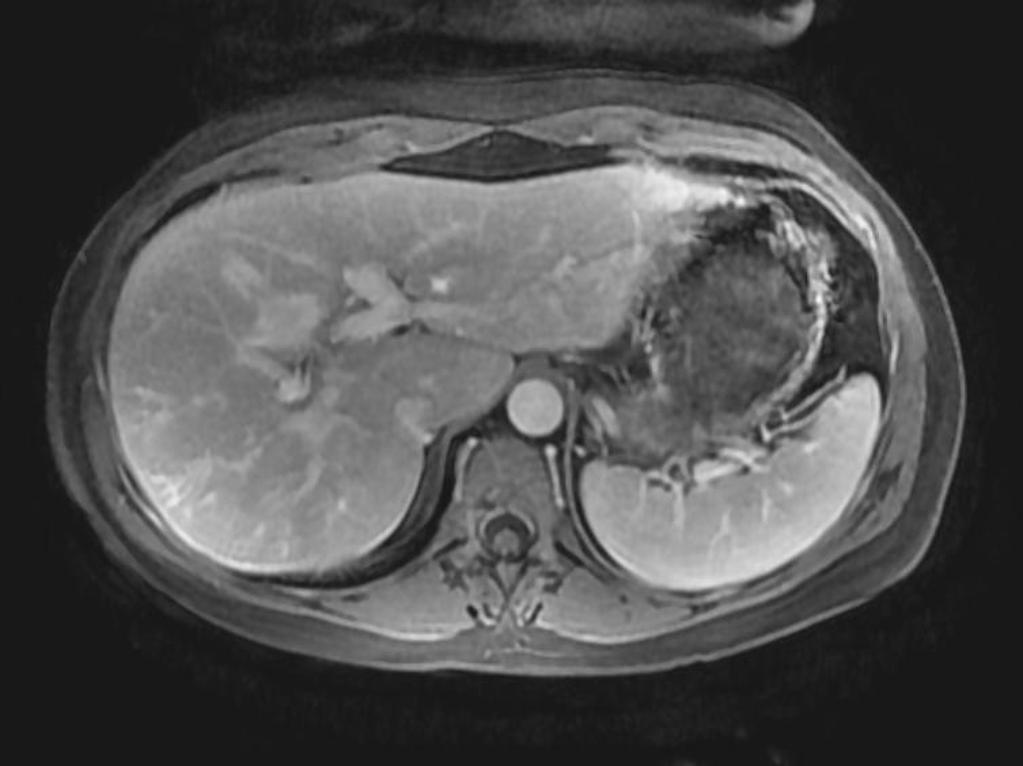 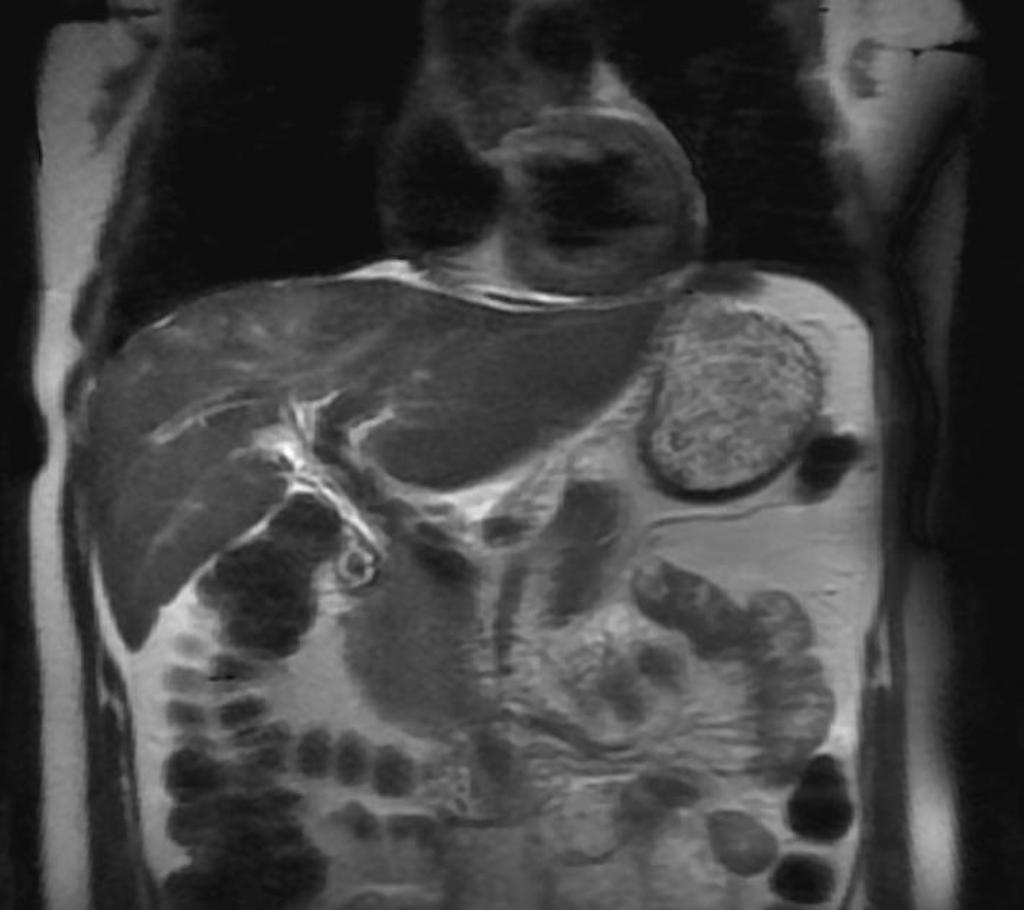 |
| Cholecystitis |
|
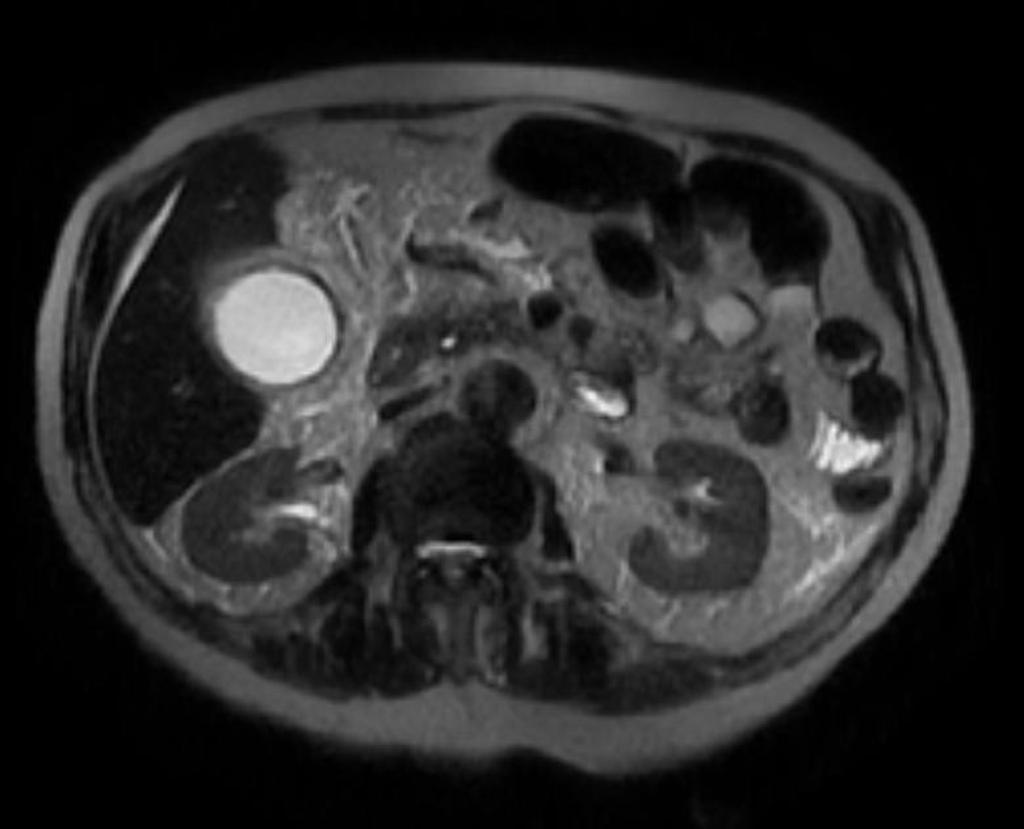 | |
| Pancreatitis |
|
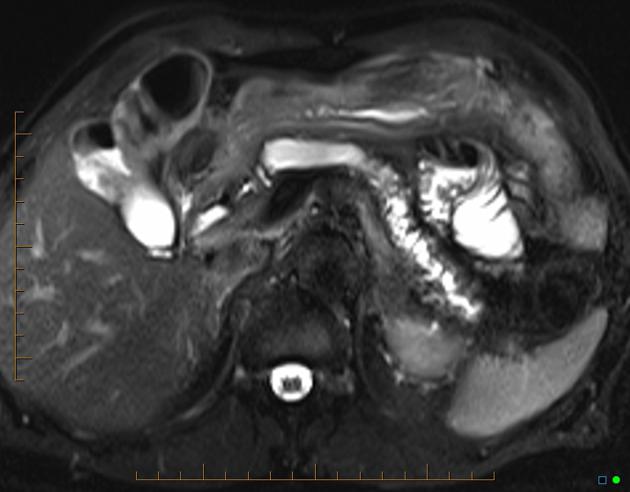 | |
| Mesenteric vasculitis |
|
||
| Cardiac | Mitral stenosis |
|
|
| Acute pericarditis |
|
 | |
| Pericardial effusion |
|
||
| Myocarditis |
|
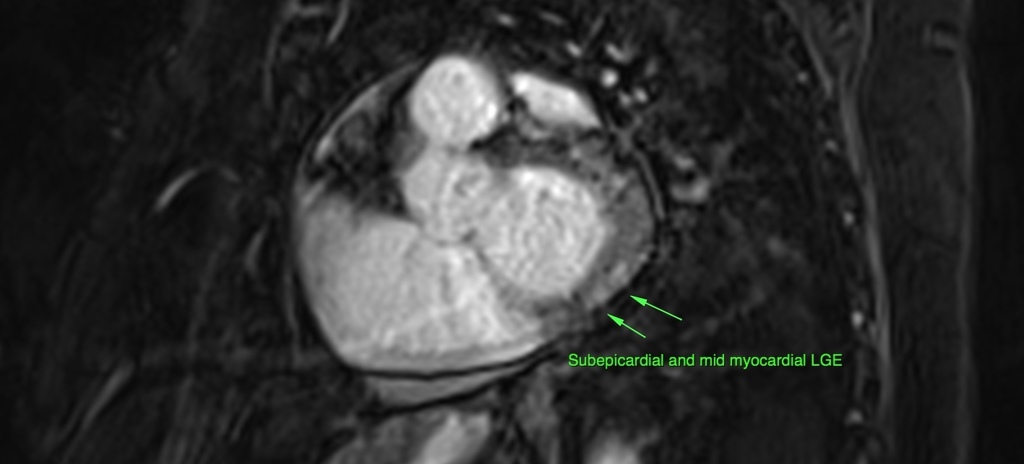 | |
| Neurological | General |
|
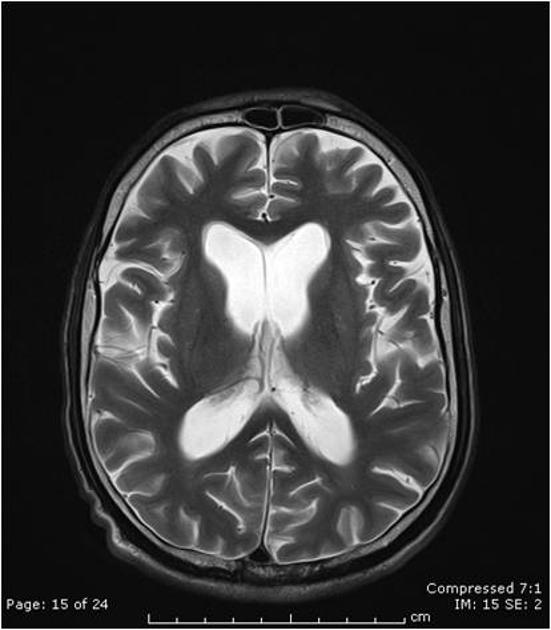 |
| Stroke |
 | ||
| Neuropathies |
|
  | |
| Autoimmune encephalitis |
|
 | |
| Musculoskeletal | Raynaud phenomen |
|
 |
| Myositis |
|
 | |
| Arthritis/tenosynovitis |
|
 | |
| Osteonecrosis (Avascular necrosis) |
|
  |
References
- ↑ Appenzeller S (2013). "Magnetic resonance imaging in systemic lupus erythematosus: where do we stand?". Cogn Behav Neurol. 26 (2): 53–4. doi:10.1097/WNN.0b013e31829d5b60. PMID 23812167.
- ↑ Thurman JM, Serkova NJ (2015). "Non-invasive imaging to monitor lupus nephritis and neuropsychiatric systemic lupus erythematosus". F1000Res. 4: 153. doi:10.12688/f1000research.6587.2. PMC 4536614. PMID 26309728.
- ↑ Lin K, Lloyd-Jones DM, Li D, Liu Y, Yang J, Markl M, Carr JC (2015). "Imaging of cardiovascular complications in patients with systemic lupus erythematosus". Lupus. 24 (11): 1126–34. doi:10.1177/0961203315588577. PMC 4567427. PMID 26038342.
- ↑ Sarbu N, Bargalló N, Cervera R (2015). "Advanced and Conventional Magnetic Resonance Imaging in Neuropsychiatric Lupus". F1000Res. 4: 162. doi:10.12688/f1000research.6522.2. PMC 4505788. PMID 26236469.
- ↑ Qin H, Guo Q, Shen N, Huang X, Wu H, Zhang M, Bao C, Chen S (2014). "Chest imaging manifestations in lupus nephritis". Clin. Rheumatol. 33 (6): 817–23. doi:10.1007/s10067-014-2586-2. PMID 24696368.
- ↑ Goh YP, Naidoo P, Ngian GS (2013). "Imaging of systemic lupus erythematosus. Part II: gastrointestinal, renal, and musculoskeletal manifestations". Clin Radiol. 68 (2): 192–202. doi:10.1016/j.crad.2012.06.109. PMID 22901453.
- ↑ Gal Y, Twig G, Mozes O, Greenberg G, Hoffmann C, Shoenfeld Y (2013). "Central nervous system involvement in systemic lupus erythematosus: an imaging challenge". Isr. Med. Assoc. J. 15 (7): 382–6. PMID 23943987.
- ↑ Shirato M, Hisa N, Fujikura Y, Ohkuma K, Kutsuki S, Hiramatsu K (1992). "[Imaging diagnosis of lupus enteritis--especially about sonographic findings]". Nihon Igaku Hoshasen Gakkai Zasshi (in Japanese). 52 (10): 1394–9. PMID 1448334.
- ↑ Adachi JD, Lau A (2014). "Systemic lupus erythematosus, osteoporosis, and fractures". J. Rheumatol. 41 (10): 1913–5. doi:10.3899/jrheum.140919. PMID 25275093.
- ↑ Curiel R, Akin EA, Beaulieu G, DePalma L, Hashefi M (2011). "PET/CT imaging in systemic lupus erythematosus". Ann. N. Y. Acad. Sci. 1228: 71–80. doi:10.1111/j.1749-6632.2011.06076.x. PMID 21718325.
- ↑ Goh YP, Naidoo P, Ngian GS (2013). "Imaging of systemic lupus erythematosus. Part I: CNS, cardiovascular, and thoracic manifestations". Clin Radiol. 68 (2): 181–91. doi:10.1016/j.crad.2012.06.110. PMID 22901452.