Syphilis pathophysiology: Difference between revisions
Aysha Aslam (talk | contribs) No edit summary |
Aysha Aslam (talk | contribs) |
||
| Line 61: | Line 61: | ||
| Line 87: | Line 80: | ||
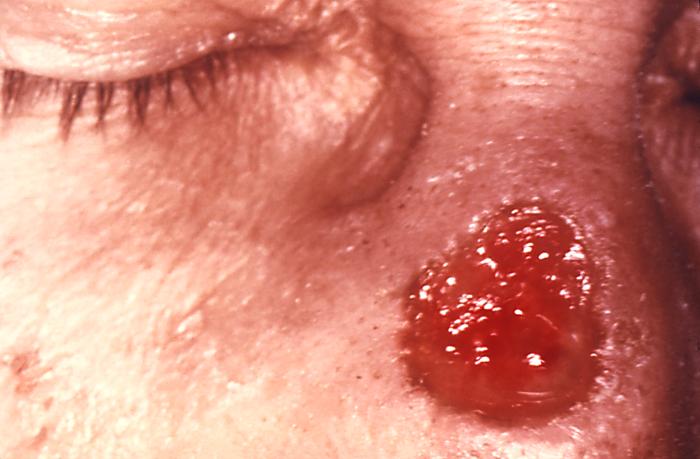
Image:Gumma of nose due to a long standing tertiary syphilitic Treponema pallidum infection 5330 lores.jpg|Gumma of the nose due to long standing tertiary syphilis | Image:Gumma of nose due to a long standing tertiary syphilitic Treponema pallidum infection 5330 lores.jpg|Gumma of the nose due to long standing tertiary syphilis | ||
</gallery> | </gallery> | ||
===Microscopic Pathology=== | ===Microscopic Pathology=== | ||
Revision as of 19:45, 26 September 2016
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]
|
Syphilis Microchapters | |
|
Diagnosis | |
|
Treatment | |
|
Case Studies | |
|
Syphilis pathophysiology On the Web | |
|
American Roentgen Ray Society Images of Syphilis pathophysiology | |
|
Risk calculators and risk factors for Syphilis pathophysiology | |
Overview
Syphilis is caused by a spirochete, treponema pallidum. It has an average incubation period of 3 - 12 weeks. However, it may vary according to the size of innoculum. Spirochete penetrates intact mucous membrane or microscopic dermal abrasions and rapidly enters systemic circulation with the central nervous system being invaded during the early phase of infection. The histopathological hallmark findings are endarteritis and plasma cell-rich infiltrates reflecting a delayed-type of hypersensitivity reaction to the spirochete.[1][2][3][4][5][6][7]
Pathogenesis
The pathogenesis of syphilis may be described in the following steps:[1][2][3][4][5][6][7][8][9][10][11]
Transmission
Treponema pallidum is usually transmitted via direct contact with the infected lesion (sexual contact) or blood transfusion (rare).
Incubation
The incubation period varies with the size of innoculum (9-90 days).
Dissemination
- Following transmission, the Trepenoma pallidum uses the intact or abraded mucous membrane to enter the body.
- It then disseminates to the lymphatics and blood stream to gain access to any organ of the body.
Seeding
- Syphilis uses fibronectin molecules to attach to the endothelial surface of the vessels in organs resulting in inflammation and obliteration of the small blood vessels causing vasculitis (end arteritis obliterans).
- Organism has slow replication rate (30-33 hrs) and evades the initial host immune response.
- It may seed to different organs of the body esp cardiovascular system and central nervous system resulting in tertiary syphilis.
Immune response
Different stages of syphilis results from the interaction between the antigen and the host immune response.[1][2]
Acute response
- The initial infection in primary syphilis is limited due to Th1 response and lack of the antibody response.
- It is speculated that there is a shift from Th1 to Th2 response during the secondary syphilis.
Chronic
- Cyototxic T cells and incomplete humoral response is mainly responsible for persistence of infection and tissue damage in the tertiary syphilis.
- Ineffective type 4 delayed hypersensitivity reaction containing macrophages and sensitized T cells is mainly responsible for the gumma formation in various organs.
Genetics
There is no known genetic association of syphilis. However, neurosyphilis may be associated with the gene polymorphism for IL 10 production with increased levels seen in the patients with neurosyphilis.[11]
Associated conditions
Syphilis is associated with the increased transmission of HIV. The underlying mechanism may be related to the accumulation of dendritic cells containing CCR5 co receptors at the site of infection, the same receptor entity binding the HIV.[9]
Gross pathology
Gross pathology
Microscopic pathology
On microscopic histopathological analysis, characteristic findings of syphilis depends on the stage of the disease:
Primary syphilis
- Mononuclear leukocytic infiltration, macrophages, and lymphocytes
- Swelling and proliferation of small blood vessels
Secondary syphilis
- Swelling and dilatation of blood vessels in the dermis
- Epidermal hyperplasia and neutrophilic infiltration
- Inflammatory cell infiltrate predominantly plasma cell
Tertiary syphilis
- Small vessel inflammation (end arteritis obliterans)
- Granulomatous lesions (gumma) containing central necrosis, inflammatory cells such as lymphocytes, macrophages, plasma cells and fibroblasts.
-
Typical presentation of secondary syphilis rash on the palms of the hands and usually also seen on soles of feet
-
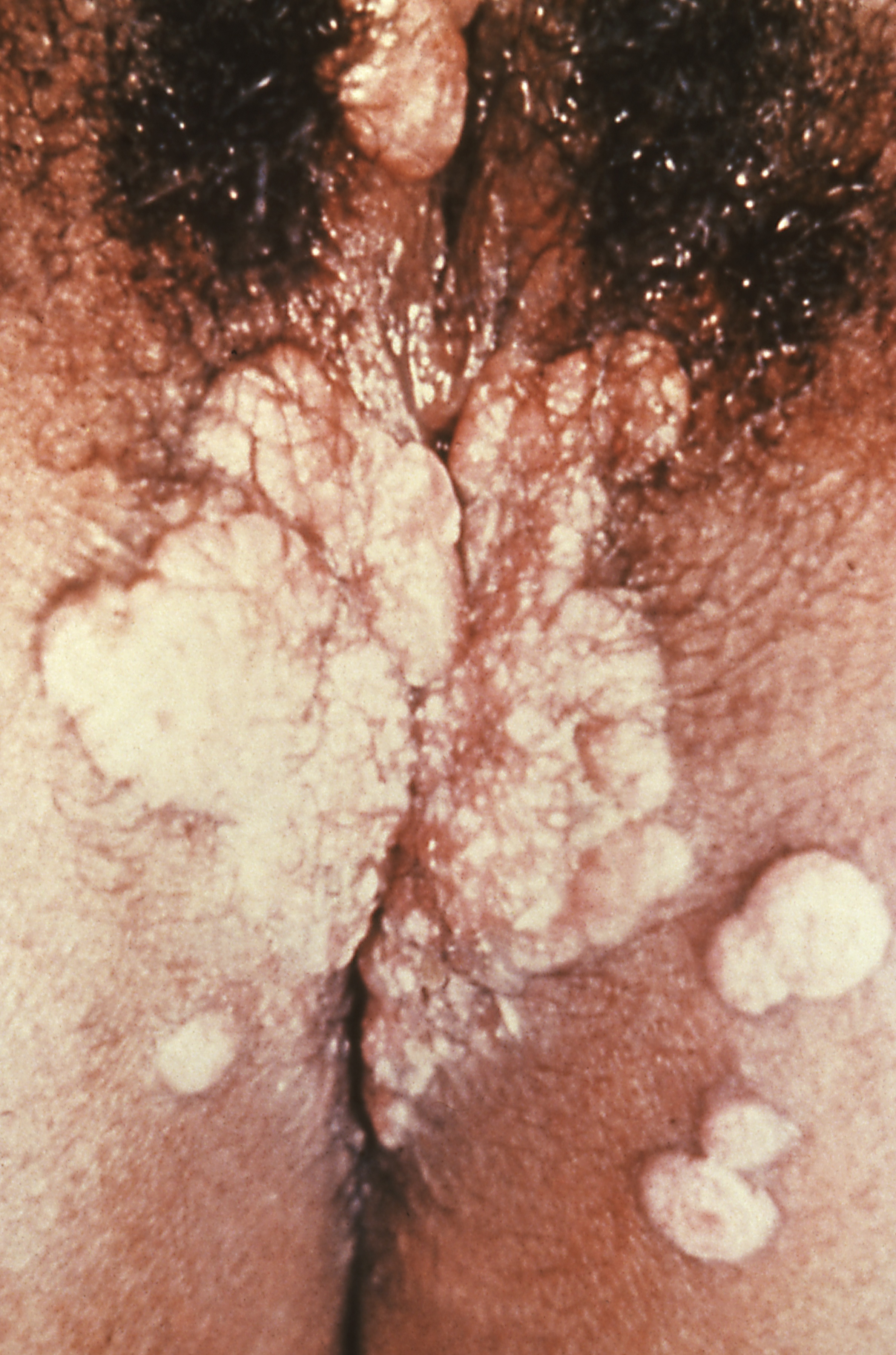
Condyoma lata (syphilis secondary)
-
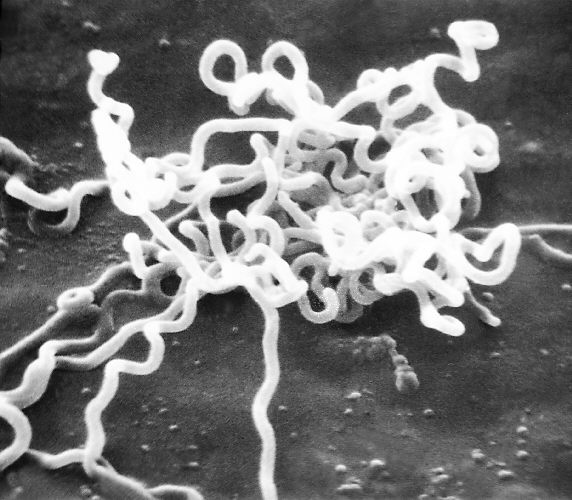
Electron micrograph of Treponema pallidum
-
Syphilis lesions on a patient's back
-
Syphilis lesions on a patient's chest
-
Chancres on the penile shaft due to a primary syphilitic infection
-
Secondary syphilis manifested perineal condylomata lata lesions, which presented as gray, raised papules that sometimes appear on the vulva or near the anus, or in any other warm intertriginous region.
-
Gumma of the nose due to long standing tertiary syphilis
Microscopic Pathology
Brain: Gumma of Syphilis
{{#ev:youtube|Cd60sjchsN8}}
Brain: Paresis (syphilis)
{{#ev:youtube|1Ibu71qHznA}}
References
- ↑ 1.0 1.1 1.2 Carlson JA, Dabiri G, Cribier B, Sell S (2011). "The immunopathobiology of syphilis: the manifestations and course of syphilis are determined by the level of delayed-type hypersensitivity". Am J Dermatopathol. 33 (5): 433–60. doi:10.1097/DAD.0b013e3181e8b587. PMC 3690623. PMID 21694502.
- ↑ 2.0 2.1 2.2 Fitzgerald TJ (1992). "The Th1/Th2-like switch in syphilitic infection: is it detrimental?". Infect Immun. 60 (9): 3475–9. PMC 257347. PMID 1386838.
- ↑ 3.0 3.1 Singh AE, Romanowski B (1999). "Syphilis: review with emphasis on clinical, epidemiologic, and some biologic features". Clin Microbiol Rev. 12 (2): 187–209. PMC 88914. PMID 10194456.
- ↑ 4.0 4.1 Engelkens HJ, ten Kate FJ, Vuzevski VD, van der Sluis JJ, Stolz E (1991). "Primary and secondary syphilis: a histopathological study". Int J STD AIDS. 2 (4): 280–4. PMID 1911961.
- ↑ 5.0 5.1 Thomas DD, Navab M, Haake DA, Fogelman AM, Miller JN, Lovett MA (1988). "Treponema pallidum invades intercellular junctions of endothelial cell monolayers". Proc Natl Acad Sci U S A. 85 (10): 3608–12. PMC 280263. PMID 3285346.
- ↑ 6.0 6.1 Quatresooz P, Piérard GE (2009). "Skin homing of Treponema pallidum in early syphilis: an immunohistochemical study". Appl Immunohistochem Mol Morphol. 17 (1): 47–50. doi:10.1097/PAI.0b013e3181788186. PMID 18800002.
- ↑ 7.0 7.1 Tanabe JL, Huntley AC (1986). "Granulomatous tertiary syphilis". J Am Acad Dermatol. 15 (2 Pt 2): 341–4. PMID 3734178.
- ↑ Baker-Zander S, Sell S (1980). "A histopathologic and immunologic study of the course of syphilis in the experimentally infected rabbit. Demonstration of long-lasting cellular immunity". Am J Pathol. 101 (2): 387–414. PMC 1903600. PMID 7001910.
- ↑ 9.0 9.1 Sheffield JS, Wendel GD, McIntire DD, Norgard MV (2007). "Effect of genital ulcer disease on HIV-1 coreceptor expression in the female genital tract". J Infect Dis. 196 (10): 1509–16. doi:10.1086/522518. PMID 18008231.
- ↑ Abell E, Marks R, Jones EW (1975). "Secondary syphilis: a clinico-pathological review". Br J Dermatol. 93 (1): 53–61. PMID 1191529.
- ↑ 11.0 11.1 Pastuszczak M, Jakiela B, Jaworek AK, Wypasek E, Zeman J, Wojas-Pelc A (2015). "Association of Interleukin-10 promoter polymorphisms with neurosyphilis". Hum Immunol. 76 (7): 469–72. doi:10.1016/j.humimm.2015.06.010. PMID 26100683.