Subgaleal hemorrhage
|
Subgaleal Hemorrhage Microchapters |
|
Diagnosis |
|---|
|
Treatment |
|
Case Studies |
|
Subgaleal hemorrhage On the Web |
|
American Roentgen Ray Society Images of Subgaleal hemorrhage |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]
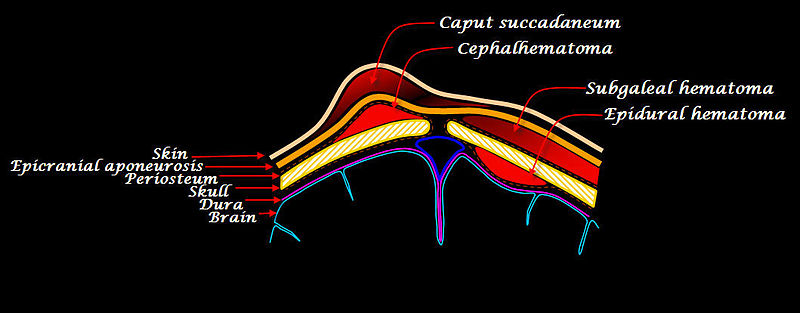
Synonyms and keywords: Subgaleal hematoma
Overview
Subgaleal hemorrhage is bleeding in the potential space between the skull periosteum and the scalp galea aponeurosis.
Causes
Majority (90%) result from vacuum applied to the head at delivery (Ventouse assisted delivery). Subgaleal hematoma has a high frequency of occurrence of associated head trauma (40%), such as intracranial hemorrhage or skull fracture. The occurrence of these features does not correlate significantly with the severity of subgaleal hemorrhage.
Symptoms
The diagnosis is generally a clinical one, with a fluctuant boggy mass developing over the scalp (especially over the occiput) with superficial skin bruising. The swelling develops gradually 12-72 hours after delivery, although it may be noted immediately after delivery in severe cases. The hematoma spreads across the whole calvaria as its growth is insidious and may not be recognized for hours. Patients with subgaleal hematoma may present with hemorrhagic shock. The swelling may obscure the fontanel and cross suture lines (distinguishing it from cephalohematoma). Watch for significant hyperbilirubinemia. The long-term prognosis is generally good. Laboratory studies consist of a hematocrit evaluation.
Management
Management consists of vigilant observation over days to detect progression. Fluid bolus may be required if blood loss is significant and patient becomes tachycardic. Transfusion and phototherapy may be necessary. Investigation for coagulopathy may be indicated.