Sporotrichosis laboratory findings: Difference between revisions
(Hyperlinked) |
|||
| Line 5: | Line 5: | ||
==Overview== | ==Overview== | ||
Laboratory findings consistent with the diagnosis of sporotrichosis include isolation of ''S. schenckii'' upon culture, molecular detection, a positive sporotrichin skin test, and techniques involving antibody detection. Definitive diagnosis of sporotrichosis occurs upon the isolation and identification of ''S. schenckii'' in culture. | Laboratory findings consistent with the diagnosis of sporotrichosis include isolation of ''S. schenckii'' upon culture, molecular detection, a positive sporotrichin skin test, and techniques involving [[Antibody microarray|antibody detection]]. Definitive diagnosis of sporotrichosis occurs upon the isolation and identification of ''S. schenckii'' in culture. | ||
==Laboratory findings== | ==Laboratory findings== | ||
* Sporotrichosis is a [[chronic (medicine)|chronic]] disease with slow progression and often subtle symptoms. It is difficult to diagnose, as many other diseases share similar symptoms and therefore must be ruled out. | * Sporotrichosis is a [[chronic (medicine)|chronic]] disease with slow progression and often subtle symptoms. It is difficult to diagnose, as many other diseases share similar symptoms and therefore must be ruled out. | ||
* While within human and animal tissues, ''S. schenckii'' exists in its yeast form. | * While within human and animal tissues, ''S. schenckii'' exists in its [[yeast]] form. | ||
* Varying in size and shape, these curved cells typically have 2-6 μm diameters with cigar-like buds offshooting from a narrow base. | * Varying in size and shape, these curved cells typically have 2-6 μm diameters with cigar-like buds offshooting from a narrow base. | ||
* Growing on Sabouraud dextrose agar, most ''S. schenckii'' strains become evident after 4 days. At this point, some strains lack dark pigment, while others have been infiltrated with dark pigment from the start. Upon transfer to Brain-Heart Infusion (BHI) agar, and cultured for 7 days at 37°C, the ''S. schenckii'' strains undergo dimorphism, manifesting as creamy off-white to beige colored colonies.<ref name="pmid21976602">{{cite journal| author=Barros MB, de Almeida Paes R, Schubach AO| title=Sporothrix schenckii and Sporotrichosis. | journal=Clin Microbiol Rev | year= 2011 | volume= 24 | issue= 4 | pages= 633-54 | pmid=21976602 | doi=10.1128/CMR.00007-11 | pmc=PMC3194828 | url=http://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=21976602 }} </ref> | * Growing on Sabouraud dextrose agar, most ''S. schenckii'' strains become evident after 4 days. At this point, some strains lack dark pigment, while others have been infiltrated with dark pigment from the start. Upon transfer to Brain-Heart Infusion (BHI) agar, and cultured for 7 days at 37°C, the ''S. schenckii'' strains undergo dimorphism, manifesting as creamy off-white to beige colored colonies.<ref name="pmid21976602">{{cite journal| author=Barros MB, de Almeida Paes R, Schubach AO| title=Sporothrix schenckii and Sporotrichosis. | journal=Clin Microbiol Rev | year= 2011 | volume= 24 | issue= 4 | pages= 633-54 | pmid=21976602 | doi=10.1128/CMR.00007-11 | pmc=PMC3194828 | url=http://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=21976602 }} </ref> | ||
* Patients with sporotrichosis will likely have [[antibodies]] against the fungus ''S. schenckii'', however, due to variability in sensitivity and specificity, antibody identification may not be a reliable diagnosis for this disease. The confirming diagnosis remains culturing the fungus from the skin, [[sputum]], [[synovial fluid]], and [[cerebrospinal fluid]]. | * Patients with sporotrichosis will likely have [[antibodies]] against the [[fungus]] ''S. schenckii'', however, due to variability in sensitivity and specificity, [[Antibody|antibody identification]] may not be a reliable diagnosis for this disease. The confirming diagnosis remains culturing the fungus from the skin, [[sputum]], [[synovial fluid]], and [[cerebrospinal fluid]]. | ||
* Cats with sporotrichosis are unique in that the exudate from their lesions may contain numerous organisms. This makes cytological evaluation of exudate a valuable diagnostic tool in this species. Exudate is pyogranulomatous and phagocytic cells may be packed with yeast forms. These are variable in size, but many are cigar-shaped.<ref name="pmid17438048">{{cite journal| author=Alvarado-Ramírez E, Torres-Rodríguez JM| title=In vitro susceptibility of Sporothrix schenckii to six antifungal agents determined using three different methods. | journal=Antimicrob Agents Chemother | year= 2007 | volume= 51 | issue= 7 | pages= 2420-3 | pmid=17438048 | doi=10.1128/AAC.01176-06 | pmc=PMC1913275 | url=http://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=17438048 }} </ref> | * Cats with sporotrichosis are unique in that the exudate from their [[lesions]] may contain numerous organisms. This makes [[cytological]] evaluation of exudate a valuable diagnostic tool in this species. Exudate is pyogranulomatous and phagocytic cells may be packed with [[yeast]] forms. These are variable in size, but many are cigar-shaped.<ref name="pmid17438048">{{cite journal| author=Alvarado-Ramírez E, Torres-Rodríguez JM| title=In vitro susceptibility of Sporothrix schenckii to six antifungal agents determined using three different methods. | journal=Antimicrob Agents Chemother | year= 2007 | volume= 51 | issue= 7 | pages= 2420-3 | pmid=17438048 | doi=10.1128/AAC.01176-06 | pmc=PMC1913275 | url=http://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=17438048 }} </ref> | ||
===Culture and Identification=== | ===Culture and Identification=== | ||
* Definitive diagnosis of sporotrichosis occurs upon the isolation and identification of ''S. schenckii'' in culture. | * Definitive diagnosis of sporotrichosis occurs upon the isolation and identification of ''S. schenckii'' in culture. | ||
* The etiological agent may be obtained when the specimen is cultured on Sabouraud agar with chloramphenicol or on mycobiotic agar.<ref name="pmid21653757">{{cite journal| author=Oliveira DC, Lopes PG, Spader TB, Mahl CD, Tronco-Alves GR, Lara VM et al.| title=Antifungal susceptibilities of Sporothrix albicans, S. brasiliensis, and S. luriei of the S. schenckii complex identified in Brazil. | journal=J Clin Microbiol | year= 2011 | volume= 49 | issue= 8 | pages= 3047-9 | pmid=21653757 | doi=10.1128/JCM.00255-11 | pmc=PMC3147739 | url=http://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=21653757 }} </ref> | * The etiological agent may be obtained when the specimen is cultured on Sabouraud agar with [[chloramphenicol]] or on mycobiotic agar.<ref name="pmid21653757">{{cite journal| author=Oliveira DC, Lopes PG, Spader TB, Mahl CD, Tronco-Alves GR, Lara VM et al.| title=Antifungal susceptibilities of Sporothrix albicans, S. brasiliensis, and S. luriei of the S. schenckii complex identified in Brazil. | journal=J Clin Microbiol | year= 2011 | volume= 49 | issue= 8 | pages= 3047-9 | pmid=21653757 | doi=10.1128/JCM.00255-11 | pmc=PMC3147739 | url=http://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=21653757 }} </ref> | ||
* Filamentous hyaline colonies begin to grow following 5-7 days of incubation at 25ºC, and may manifest with pigmented centers.<ref name="pmid12372075">{{cite journal| author=Morris-Jones R| title=Sporotrichosis. | journal=Clin Exp Dermatol | year= 2002 | volume= 27 | issue= 6 | pages= 427-31 | pmid=12372075 | doi= | pmc= | url=http://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=12372075 }} </ref> | * Filamentous hyaline colonies begin to grow following 5-7 days of incubation at 25ºC, and may manifest with pigmented centers.<ref name="pmid12372075">{{cite journal| author=Morris-Jones R| title=Sporotrichosis. | journal=Clin Exp Dermatol | year= 2002 | volume= 27 | issue= 6 | pages= 427-31 | pmid=12372075 | doi= | pmc= | url=http://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=12372075 }} </ref> | ||
* Ultimately, the isolation of ''S. schenckii'' is dependent on 5-7 day a subculture of the fungus on enriched agars, such as Brain Heart Infusion agar, at 35-37ºC. Isolation is verified following the demonstration of dimorphism.<ref name="pmid21976602">{{cite journal| author=Barros MB, de Almeida Paes R, Schubach AO| title=Sporothrix schenckii and Sporotrichosis. | journal=Clin Microbiol Rev | year= 2011 | volume= 24 | issue= 4 | pages= 633-54 | pmid=21976602 | doi=10.1128/CMR.00007-11 | pmc=PMC3194828 | url=http://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=21976602 }} </ref> | * Ultimately, the isolation of ''S. schenckii'' is dependent on 5-7 day a subculture of the fungus on enriched agars, such as Brain Heart Infusion agar, at 35-37ºC. Isolation is verified following the demonstration of dimorphism.<ref name="pmid21976602">{{cite journal| author=Barros MB, de Almeida Paes R, Schubach AO| title=Sporothrix schenckii and Sporotrichosis. | journal=Clin Microbiol Rev | year= 2011 | volume= 24 | issue= 4 | pages= 633-54 | pmid=21976602 | doi=10.1128/CMR.00007-11 | pmc=PMC3194828 | url=http://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=21976602 }} </ref> | ||
* In some cases, isolation requires multiple subcultures. | * In some cases, isolation requires multiple subcultures. | ||
* While positive a culture is the strongest indication for diagnosis, this method may be more realistic in cutaneous forms of the disease than in certain systematic manifestations, due to greater lengths required for the collection of fungus in systematic forms.<ref name="pmid21976602" /> | * While positive a culture is the strongest indication for diagnosis, this method may be more realistic in cutaneous forms of the disease than in certain systematic manifestations, due to greater lengths required for the collection of [[fungus]] in systematic forms.<ref name="pmid21976602" /> | ||
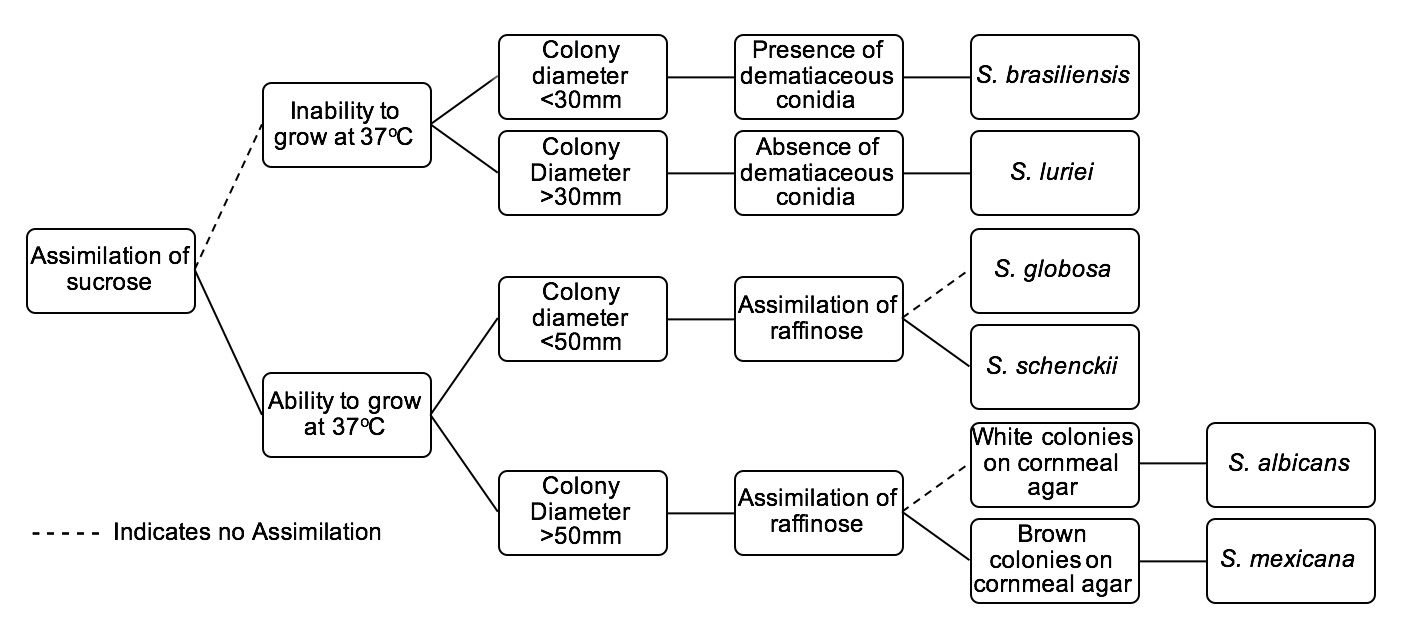
The gold standard for diagnosis of Sporotrichosis is with fungal culture. The tree below serves as an identification key for six ''Sporothrix'' species of clinical interest: | The gold standard for diagnosis of Sporotrichosis is with [[fungal]] culture. The tree below serves as an identification key for six ''Sporothrix'' species of clinical interest: | ||
[[Image:Sporotree.jpg|thumb|none|800x800px|Identification tree for ''Sporothrix'' species of clinical interest. These clinically significant ''Sporothrix'' species include: ''S. brasiliensis'', ''S. luriei'', ''S. globosa'', ''S. schenckii'', ''S. albicans'', and ''S. mexicana''. When cultivating at 37°C, specimens are to be cultured on Potato Dextrose Agar.<ref name="pmid21976602">{{cite journal| author=Barros MB, de Almeida Paes R, Schubach AO| title=Sporothrix schenckii and Sporotrichosis. | journal=Clin Microbiol Rev | year= 2011 | volume= 24 | issue= 4 | pages= 633-54 | pmid=21976602 | doi=10.1128/CMR.00007-11 | pmc=PMC3194828 | url=http://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=21976602 }} </ref> ]] | [[Image:Sporotree.jpg|thumb|none|800x800px|Identification tree for ''Sporothrix'' species of clinical interest. These clinically significant ''Sporothrix'' species include: ''S. brasiliensis'', ''S. luriei'', ''S. globosa'', ''S. schenckii'', ''S. albicans'', and ''S. mexicana''. When cultivating at 37°C, specimens are to be cultured on Potato Dextrose Agar.<ref name="pmid21976602">{{cite journal| author=Barros MB, de Almeida Paes R, Schubach AO| title=Sporothrix schenckii and Sporotrichosis. | journal=Clin Microbiol Rev | year= 2011 | volume= 24 | issue= 4 | pages= 633-54 | pmid=21976602 | doi=10.1128/CMR.00007-11 | pmc=PMC3194828 | url=http://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=21976602 }} </ref> ]] | ||
| Line 31: | Line 31: | ||
* Though there is a scarcity of molecular methods of diagnosis for Sporotrichosis in standard care, researchers have identified a variety of detection systems. | * Though there is a scarcity of molecular methods of diagnosis for Sporotrichosis in standard care, researchers have identified a variety of detection systems. | ||
* Molecular findings specific to specimens of Sporotrichosis: | * Molecular findings specific to specimens of Sporotrichosis: | ||
** Detected particular nucleic acid probes that target large subunit rRNA genes from ''S. schenckii'' | ** Detected particular [[nucleic acid]] probes that target large subunit [[rRNA]] genes from ''S. schenckii'' | ||
** Additionally, the researchers extracted DNA from clinical specimens by boiling them in an alkaline guanidine-phenol-Tris reagent, amplifying a segment of the 28S rRNA gene with universal primers, and utilizing amplicon identification via probe hybridization.<ref name="pmid8576345">{{cite journal| author=Sandhu GS, Kline BC, Stockman L, Roberts GD| title=Molecular probes for diagnosis of fungal infections. | journal=J Clin Microbiol | year= 1995 | volume= 33 | issue= 11 | pages= 2913-9 | pmid=8576345 | doi= | pmc=PMC228606 | url=http://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=8576345 }} </ref> | ** Additionally, the researchers extracted [[DNA]] from clinical specimens by boiling them in an [[alkaline]] guanidine-phenol-Tris reagent, amplifying a segment of the 28S [[Ribosomal RNA|rRNA]] gene with universal [[Primer (molecular biology)|primers]], and utilizing [[amplicon]] identification via probe hybridization.<ref name="pmid8576345">{{cite journal| author=Sandhu GS, Kline BC, Stockman L, Roberts GD| title=Molecular probes for diagnosis of fungal infections. | journal=J Clin Microbiol | year= 1995 | volume= 33 | issue= 11 | pages= 2913-9 | pmid=8576345 | doi= | pmc=PMC228606 | url=http://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=8576345 }} </ref> | ||
===Sporotrichin Skin Test=== | ===Sporotrichin Skin Test=== | ||
| Line 39: | Line 39: | ||
* In roughly 90% of confirmed sporotrichosis cases, the test comes back positive.<ref name="pmid3709907">{{cite journal| author=Itoh M, Okamoto S, Kariya H| title=Survey of 200 cases of sporotrichosis. | journal=Dermatologica | year= 1986 | volume= 172 | issue= 4 | pages= 209-13 | pmid=3709907 | doi= | pmc= | url=http://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=3709907 }} </ref> | * In roughly 90% of confirmed sporotrichosis cases, the test comes back positive.<ref name="pmid3709907">{{cite journal| author=Itoh M, Okamoto S, Kariya H| title=Survey of 200 cases of sporotrichosis. | journal=Dermatologica | year= 1986 | volume= 172 | issue= 4 | pages= 209-13 | pmid=3709907 | doi= | pmc= | url=http://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=3709907 }} </ref> | ||
* A positive test result may also result following a previous ''S. schenckii'' infection. | * A positive test result may also result following a previous ''S. schenckii'' infection. | ||
* There is a lack of standardization in regards to antigen production, which may result in a variation in findings.<ref name="pmid21976602" /> | * There is a lack of standardization in regards to [[antigen]] production, which may result in a variation in findings.<ref name="pmid21976602" /> | ||
===Antibody Detection and Identification=== | ===Antibody Detection and Identification=== | ||
* Findings from antibody detection techniques merely establish speculative diagnosis for sporotrichosis. The use of additional methods of clinical and epidemiological associations is necessary for definite diagnosis. | * Findings from [[antibody]] detection techniques merely establish speculative diagnosis for sporotrichosis. The use of additional methods of clinical and epidemiological associations is necessary for definite diagnosis. | ||
* Antibody detection in sera from infected hosts has been outlined as a diagnostic tool for cases of sporotrichosis. | * Antibody detection in sera from infected hosts has been outlined as a diagnostic tool for cases of sporotrichosis. | ||
* Precipitation and agglutination methods were among the first techniques. | * [[Precipitation (chemistry)|Precipitation]] and [[agglutination]] methods were among the first techniques. | ||
* Double immunodiffusion does not typically display cross reactions with the sera specimens taken from hosts with other infectious diseases that have similar clinical findings, namely [[chromoblastomycosis]] and [[leishmaniasis]]. | * Double [[immunodiffusion]] does not typically display cross reactions with the sera specimens taken from hosts with other [[Infectious disease|infectious diseases]] that have similar clinical findings, namely [[chromoblastomycosis]] and [[leishmaniasis]]. | ||
* Researchers have found that an anodic arc, or S arc, upon [[immunoelectrophoresis]] is characteristic of cases of sporotrichosis.<ref name="pmid6429540">{{cite journal| author=de Albornoz MB, Villanueva E, de Torres ED| title=Application of immunoprecipitation techniques to the diagnosis of cutaneous and extracutaneous forms of sporotrichosis. | journal=Mycopathologia | year= 1984 | volume= 85 | issue= 3 | pages= 177-83 | pmid=6429540 | doi= | pmc= | url=http://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=6429540 }} </ref> | * Researchers have found that an anodic arc, or S arc, upon [[immunoelectrophoresis]] is characteristic of cases of sporotrichosis.<ref name="pmid6429540">{{cite journal| author=de Albornoz MB, Villanueva E, de Torres ED| title=Application of immunoprecipitation techniques to the diagnosis of cutaneous and extracutaneous forms of sporotrichosis. | journal=Mycopathologia | year= 1984 | volume= 85 | issue= 3 | pages= 177-83 | pmid=6429540 | doi= | pmc= | url=http://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=6429540 }} </ref> | ||
* Tube and latex agglutination have been used since the 1970's as a means of serodiagnosis, though this technique is less effective in cases of cutaneous sporotrichosis. | * Tube and latex [[agglutination]] have been used since the 1970's as a means of serodiagnosis, though this technique is less effective in cases of cutaneous sporotrichosis. | ||
* Immunoenzymatic assays have been used as a means of serodiagnosis. | * Immunoenzymatic [[assays]] have been used as a means of serodiagnosis. | ||
* An enzyme-linked immunosorbent assay (ELISA) was developed for specific antibody detection in serum specimens of patients with sporotrichosis.<ref name="pmid17215334">{{cite journal| author=Almeida-Paes R, Pimenta MA, Pizzini CV, Monteiro PC, Peralta JM, Nosanchuk JD et al.| title=Use of mycelial-phase Sporothrix schenckii exoantigens in an enzyme-linked immunosorbent assay for diagnosis of sporotrichosis by antibody detection. | journal=Clin Vaccine Immunol | year= 2007 | volume= 14 | issue= 3 | pages= 244-9 | pmid=17215334 | doi=10.1128/CVI.00430-06 | pmc=PMC1828849 | url=http://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=17215334 }} </ref> | * An [[Enzyme linked immunosorbent assay (ELISA)|enzyme-linked immunosorbent assay (ELISA)]] was developed for specific antibody detection in serum specimens of patients with sporotrichosis.<ref name="pmid17215334">{{cite journal| author=Almeida-Paes R, Pimenta MA, Pizzini CV, Monteiro PC, Peralta JM, Nosanchuk JD et al.| title=Use of mycelial-phase Sporothrix schenckii exoantigens in an enzyme-linked immunosorbent assay for diagnosis of sporotrichosis by antibody detection. | journal=Clin Vaccine Immunol | year= 2007 | volume= 14 | issue= 3 | pages= 244-9 | pmid=17215334 | doi=10.1128/CVI.00430-06 | pmc=PMC1828849 | url=http://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=17215334 }} </ref> | ||
** In 2007, researchers discussed an enzyme-linked immunosorbent assay, also known as [[Enzyme linked immunosorbent assay (ELISA)|ELISA]]. [[ELISA]] functions by detecting particular antibodies in the serum samples from infected patients. Though [[ELISA]] demonstrated 100% sensitivity to all 35 positive serum samples, sera samples from patients with cutaneous [[leishmaniasis]] resulted in cross-results. | ** In 2007, researchers discussed [[Enzyme linked immunosorbent assay (ELISA)|an enzyme-linked immunosorbent assay]], also known as [[Enzyme linked immunosorbent assay (ELISA)|ELISA]]. [[ELISA]] functions by detecting particular [[antibodies]] in the [[serum]] samples from infected patients. Though [[ELISA]] demonstrated 100% sensitivity to all 35 positive [[serum]] samples, sera samples from patients with cutaneous [[leishmaniasis]] resulted in cross-results. | ||
** In instances involving cross-results and false positives, [[ELISA]] may be use in addition to other diagnostic techniques. | ** In instances involving cross-results and false positives, [[ELISA]] may be use in addition to other diagnostic techniques. | ||
* Exoantigens formed by a mycelial-phase ''S. schenckii'' strain were isolated amidst an epidemic in Rio de Janeiro, Brazil. This epidemic was the first that was rooted in zoonotic transmission. | * Exoantigens formed by a mycelial-phase ''S. schenckii'' strain were isolated amidst an [[epidemic]] in Rio de Janeiro, Brazil. This [[epidemic]] was the first that was rooted in [[zoonotic]] transmission. | ||
** Researchers developed an enzyme immunoassay with these exoantigens. | ** Researchers developed an enzyme [[immunoassay]] with these exoantigens. | ||
** Researchers described and experimented with this antigen, finding no cross-results with sera taken from patients with other mycoses.<ref name="pmid12462523">{{cite journal| author=Mendoza M, Díaz AM, Hung MB, Zambrano EA, Díaz E, De Albornoz MC| title=Production of culture filtrates of Sporothrix schenckii in diverse culture media. | journal=Med Mycol | year= 2002 | volume= 40 | issue= 5 | pages= 447-54 | pmid=12462523 | doi= | pmc= | url=http://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=12462523 }} </ref> | ** Researchers described and experimented with this [[antigen]], finding no cross-results with sera taken from patients with other [[mycoses]].<ref name="pmid12462523">{{cite journal| author=Mendoza M, Díaz AM, Hung MB, Zambrano EA, Díaz E, De Albornoz MC| title=Production of culture filtrates of Sporothrix schenckii in diverse culture media. | journal=Med Mycol | year= 2002 | volume= 40 | issue= 5 | pages= 447-54 | pmid=12462523 | doi= | pmc= | url=http://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=12462523 }} </ref> | ||
==References== | ==References== | ||
Revision as of 16:18, 28 January 2016
|
Sporotrichosis Microchapters |
|
Diagnosis |
|---|
|
Treatment |
|
Case Studies |
|
Sporotrichosis laboratory findings On the Web |
|
American Roentgen Ray Society Images of Sporotrichosis laboratory findings |
|
Risk calculators and risk factors for Sporotrichosis laboratory findings |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]; Associate Editor(s)-in-Chief: Alison Leibowitz [2]
Overview
Laboratory findings consistent with the diagnosis of sporotrichosis include isolation of S. schenckii upon culture, molecular detection, a positive sporotrichin skin test, and techniques involving antibody detection. Definitive diagnosis of sporotrichosis occurs upon the isolation and identification of S. schenckii in culture.
Laboratory findings
- Sporotrichosis is a chronic disease with slow progression and often subtle symptoms. It is difficult to diagnose, as many other diseases share similar symptoms and therefore must be ruled out.
- While within human and animal tissues, S. schenckii exists in its yeast form.
- Varying in size and shape, these curved cells typically have 2-6 μm diameters with cigar-like buds offshooting from a narrow base.
- Growing on Sabouraud dextrose agar, most S. schenckii strains become evident after 4 days. At this point, some strains lack dark pigment, while others have been infiltrated with dark pigment from the start. Upon transfer to Brain-Heart Infusion (BHI) agar, and cultured for 7 days at 37°C, the S. schenckii strains undergo dimorphism, manifesting as creamy off-white to beige colored colonies.[1]
- Patients with sporotrichosis will likely have antibodies against the fungus S. schenckii, however, due to variability in sensitivity and specificity, antibody identification may not be a reliable diagnosis for this disease. The confirming diagnosis remains culturing the fungus from the skin, sputum, synovial fluid, and cerebrospinal fluid.
- Cats with sporotrichosis are unique in that the exudate from their lesions may contain numerous organisms. This makes cytological evaluation of exudate a valuable diagnostic tool in this species. Exudate is pyogranulomatous and phagocytic cells may be packed with yeast forms. These are variable in size, but many are cigar-shaped.[2]
Culture and Identification
- Definitive diagnosis of sporotrichosis occurs upon the isolation and identification of S. schenckii in culture.
- The etiological agent may be obtained when the specimen is cultured on Sabouraud agar with chloramphenicol or on mycobiotic agar.[3]
- Filamentous hyaline colonies begin to grow following 5-7 days of incubation at 25ºC, and may manifest with pigmented centers.[4]
- Ultimately, the isolation of S. schenckii is dependent on 5-7 day a subculture of the fungus on enriched agars, such as Brain Heart Infusion agar, at 35-37ºC. Isolation is verified following the demonstration of dimorphism.[1]
- In some cases, isolation requires multiple subcultures.
- While positive a culture is the strongest indication for diagnosis, this method may be more realistic in cutaneous forms of the disease than in certain systematic manifestations, due to greater lengths required for the collection of fungus in systematic forms.[1]
The gold standard for diagnosis of Sporotrichosis is with fungal culture. The tree below serves as an identification key for six Sporothrix species of clinical interest:
Molecular Detection and Identification
- Though there is a scarcity of molecular methods of diagnosis for Sporotrichosis in standard care, researchers have identified a variety of detection systems.
- Molecular findings specific to specimens of Sporotrichosis:
- Detected particular nucleic acid probes that target large subunit rRNA genes from S. schenckii
- Additionally, the researchers extracted DNA from clinical specimens by boiling them in an alkaline guanidine-phenol-Tris reagent, amplifying a segment of the 28S rRNA gene with universal primers, and utilizing amplicon identification via probe hybridization.[5]
Sporotrichin Skin Test
- While the cutaneous sporotrichin skin test can serve as a helpful diagnostic tool, it is mainly utilized in epidemiological studies.
- The test detects the cellular immune response, delayed hypersensitivity.
- In roughly 90% of confirmed sporotrichosis cases, the test comes back positive.[6]
- A positive test result may also result following a previous S. schenckii infection.
- There is a lack of standardization in regards to antigen production, which may result in a variation in findings.[1]
Antibody Detection and Identification
- Findings from antibody detection techniques merely establish speculative diagnosis for sporotrichosis. The use of additional methods of clinical and epidemiological associations is necessary for definite diagnosis.
- Antibody detection in sera from infected hosts has been outlined as a diagnostic tool for cases of sporotrichosis.
- Precipitation and agglutination methods were among the first techniques.
- Double immunodiffusion does not typically display cross reactions with the sera specimens taken from hosts with other infectious diseases that have similar clinical findings, namely chromoblastomycosis and leishmaniasis.
- Researchers have found that an anodic arc, or S arc, upon immunoelectrophoresis is characteristic of cases of sporotrichosis.[7]
- Tube and latex agglutination have been used since the 1970's as a means of serodiagnosis, though this technique is less effective in cases of cutaneous sporotrichosis.
- Immunoenzymatic assays have been used as a means of serodiagnosis.
- An enzyme-linked immunosorbent assay (ELISA) was developed for specific antibody detection in serum specimens of patients with sporotrichosis.[8]
- In 2007, researchers discussed an enzyme-linked immunosorbent assay, also known as ELISA. ELISA functions by detecting particular antibodies in the serum samples from infected patients. Though ELISA demonstrated 100% sensitivity to all 35 positive serum samples, sera samples from patients with cutaneous leishmaniasis resulted in cross-results.
- In instances involving cross-results and false positives, ELISA may be use in addition to other diagnostic techniques.
- Exoantigens formed by a mycelial-phase S. schenckii strain were isolated amidst an epidemic in Rio de Janeiro, Brazil. This epidemic was the first that was rooted in zoonotic transmission.
- Researchers developed an enzyme immunoassay with these exoantigens.
- Researchers described and experimented with this antigen, finding no cross-results with sera taken from patients with other mycoses.[9]
References
- ↑ 1.0 1.1 1.2 1.3 1.4 Barros MB, de Almeida Paes R, Schubach AO (2011). "Sporothrix schenckii and Sporotrichosis". Clin Microbiol Rev. 24 (4): 633–54. doi:10.1128/CMR.00007-11. PMC 3194828. PMID 21976602.
- ↑ Alvarado-Ramírez E, Torres-Rodríguez JM (2007). "In vitro susceptibility of Sporothrix schenckii to six antifungal agents determined using three different methods". Antimicrob Agents Chemother. 51 (7): 2420–3. doi:10.1128/AAC.01176-06. PMC 1913275. PMID 17438048.
- ↑ Oliveira DC, Lopes PG, Spader TB, Mahl CD, Tronco-Alves GR, Lara VM; et al. (2011). "Antifungal susceptibilities of Sporothrix albicans, S. brasiliensis, and S. luriei of the S. schenckii complex identified in Brazil". J Clin Microbiol. 49 (8): 3047–9. doi:10.1128/JCM.00255-11. PMC 3147739. PMID 21653757.
- ↑ Morris-Jones R (2002). "Sporotrichosis". Clin Exp Dermatol. 27 (6): 427–31. PMID 12372075.
- ↑ Sandhu GS, Kline BC, Stockman L, Roberts GD (1995). "Molecular probes for diagnosis of fungal infections". J Clin Microbiol. 33 (11): 2913–9. PMC 228606. PMID 8576345.
- ↑ Itoh M, Okamoto S, Kariya H (1986). "Survey of 200 cases of sporotrichosis". Dermatologica. 172 (4): 209–13. PMID 3709907.
- ↑ de Albornoz MB, Villanueva E, de Torres ED (1984). "Application of immunoprecipitation techniques to the diagnosis of cutaneous and extracutaneous forms of sporotrichosis". Mycopathologia. 85 (3): 177–83. PMID 6429540.
- ↑ Almeida-Paes R, Pimenta MA, Pizzini CV, Monteiro PC, Peralta JM, Nosanchuk JD; et al. (2007). "Use of mycelial-phase Sporothrix schenckii exoantigens in an enzyme-linked immunosorbent assay for diagnosis of sporotrichosis by antibody detection". Clin Vaccine Immunol. 14 (3): 244–9. doi:10.1128/CVI.00430-06. PMC 1828849. PMID 17215334.
- ↑ Mendoza M, Díaz AM, Hung MB, Zambrano EA, Díaz E, De Albornoz MC (2002). "Production of culture filtrates of Sporothrix schenckii in diverse culture media". Med Mycol. 40 (5): 447–54. PMID 12462523.