Splenomegaly: Difference between revisions
No edit summary |
No edit summary |
||
| Line 14: | Line 14: | ||
MeshID = D013163 | | MeshID = D013163 | | ||
}} | }} | ||
{{ | {{Splenomegaly}} | ||
{{CMG}}; {{AOEIC}} Gichoya Judy Wawira [mailto:judywawira@gmail.com], Moi University School of Medicine | {{CMG}}; {{AOEIC}} Gichoya Judy Wawira [mailto:judywawira@gmail.com], Moi University School of Medicine | ||
Revision as of 19:58, 29 August 2012
| Splenomegaly | |
 | |
|---|---|
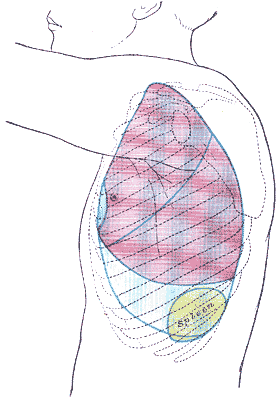
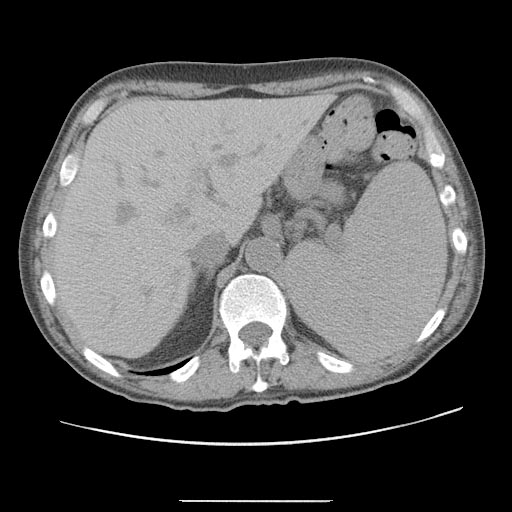
| Massively enlarged spleen, the result of extramedullary hematopoiesis, is outlined above. This patient's left upper quadrant appears more full than the corresponding area on the right. Image courtesy of Charlie Goldberg, M.D., UCSD School of Medicine and VA Medical Center, San Diego, California | |
| ICD-10 | Q89.0, R16.1 |
| ICD-9 | 759.0, 789.2 |
| DiseasesDB | 12375 |
| MedlinePlus | 003276 |
| MeSH | D013163 |
Template:Splenomegaly Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]; Associate Editor(s)-In-Chief: Gichoya Judy Wawira [2], Moi University School of Medicine
Overview
Splenomegaly is an enlargement of the spleen, which usually lies in the left upper quadrant (LUQ) of the human abdomen. It is one of the four cardinal signs of hypersplenism, the other three being cytopenia(s), normal or hyperplastic bone marrow, and a response to splenectomy. Splenomegaly is usually associated with increased workload (such as in hemolytic anemias), which suggests that it is a response to hyperfunction. It is therefore not surprising that splenomegaly is associated with any disease process that involves abnormal red blood cells being destroyed in the spleen. Other common causes include congestion due to portal hypertension and infiltration by leukemias and lymphomas.
Complete differential diagnosis splenomegaly in alphabetical order
In alphabetical order. [1] [2]
- AIDS
- Angioimmunoblastic lymphoanedopathy
- Angiosarcoma
- Autoimmune hemolytic anemia
- Bacterial septicemia
- Bone marrow damage
- Bone marrow infiltration
- Brucellosis
- Castleman's syndrome
- Cavernous transformation of the portal vein
- Cellular infiltration
- Chronic myoletic leukemia
- Collagen vascular diseases
- Congestive heart failure
- Constrictive pericarditis
- Coronavirus
- Corynebacterium diphtheriae
- Cytomegalovirus
- Early sickle cell anemia
- Endocarditis
- Ehrlichiosis
- Eosinophillic granuloma
- Epstein-Barr Virus Infection
- Felty's syndrome
- Fever unknown origin
- Fibromas
- Fungal infections
- Gaucher's disease
- Hemangiomas
- Hamartomas
- Hemoglobinopathy
- Hemolytic anemia
- Hepatic echinococcosis
- Hepatic schistomasis
- Hepatic vein obstruction
- Hepatitis
- Hereditary spherocytosis
- Histiocytosis
- Histoplasmosis
- HIV
- Hodgkin's lymphoma
- Hurler's syndrome
- Hyperlipidemias
- Idiopathic splenomegaly
- Immune hemolytic anemias
- Infective Endocarditis
- Infectious mononucleosis
- Interleukin-2
- Iron deficiency anemia
- Leishmaniasis
- Letterer-Siwe disease
- Leukemia
- Lymphangiomas
- Lymphoid leukemia
- Lympho-reticulosarcoma
- Malaria
- Malignancy
- Melanoma
- Myelofibrosis
- Myeloid leukemia
- Myeloid metaplasia
- Monocytic leukemia
- Mononucleosis
- Myobacterium avium complex
- Myoproliferative syndrome(s)
- Niemann-Pick disease
- Non-Hodgkin's lymphoma
- Nutritional anemias
- Osteomyelosclerosis
- Paroxysmal nocturnal hemoglobinuria
- Polycythemia vera
- Portal hypertension
- Q fever
- Radiation
- Rheumatoid arthritis
- RMSF
- Sarcoidosis
- Schistosomiasis
- Serum sickness
- Sickle cell disease
- Splenic abscess
- Splenic artery anuerysm
- Splenic cysts
- Splenic hamartoma
- Splenic hemangioma
- Splenic vein obstruction/thrombosis
- Stillness disease
- Subacute bacterial endocarditis
- Syphillis
- Systemic lupus erythematosus
- Tangier disease
- Thalassemia major
- Thyrotoxicosis
- Toxoplasmosis
- Trauma
- Trypanosomiasis
- Tuberculosis
- Tumors
- Typhoid fever
- Vein obstruction
- Viral hepatitis
- Weil's disease
- Less common causes [3]
Differential diagnosis of causes by organ system or pathogenesis
Splenomegaly grouped on the basis of the pathogenic mechanism
The causes of massive splenomegaly (>1000gms) are much fewer and include:
Thalassemia
Kala-Azar (Leishmaniasis)
Portal hypertension of Bilharziasis
Chronic myelogenous leukemia
lymphomas
hairy cell leukemia
myelofibrosis
polycythemia vera
Gauchers disease
chronic lymphocytic leukemia
sarcoidosis
autoimmune hemolytic anemia
Malaria
Clinical presentation
Symptoms may include abdominal pain, early satiety due to splenic encroachment, or the symptoms of anemia due to accompanying cytopenia.
Signs of splenomegaly may include a palpable left upper quadrant abdominal mass or splenic rub. It can be detected on physical examination by using Castell's sign or Traube's space, but an ultrasound can be used to confirm diagnosis.[4]
Treatment
If the splenomegaly underlies hypersplenism, a splenectomy is indicated and will correct the problem. After splenectomy, however, patients have an increased risk for infectious diseases.
After splenectomy, patients should be vaccinated against Haemophilus influenzae and Streptococcus pneumoniae. They should receive annual influenza vaccinations. Long-term prophylactic antibiotics should be given.
Related chapters
Resources
- PatientPlus Splenomegaly and hypersplenism
- Template:MerckManual (Hypersplenism)
References
- ↑ Sailer, Christian, Wasner, Susanne. Differential Diagnosis Pocket. Hermosa Beach, CA: Borm Bruckmeir Publishing LLC, 2002:77 ISBN 1591032016
- ↑ Kahan, Scott, Smith, Ellen G. In A Page: Signs and Symptoms. Malden, Massachusetts: Blackwell Publishing, 2004:68 ISBN 140510368X
- ↑ Kahan, Scott, Smith, Ellen G. In a page: Signs and Symptoms. Malden, Massachusetts: Blackwell Publishing, 2004:157
- ↑ Grover SA, Barkun AN, Sackett DL (1993). "The rational clinical examination. Does this patient have splenomegaly?". JAMA. 270 (18): 2218–21. PMID 8411607. Ovid full text
Template:Phakomatoses and other congenital malformations not elsewhere classified
Template:Skin and subcutaneous tissue symptoms and signs Template:Nervous and musculoskeletal system symptoms and signs Template:Urinary system symptoms and signs Template:Cognition, perception, emotional state and behaviour symptoms and signs Template:Speech and voice symptoms and signs Template:General symptoms and signs