Splenic vein thrombosis pathophysiology
|
Splenic vein thrombosis Microchapters |
|
Diagnosis |
|---|
|
Treatment |
|
Case Studies |
|
Splenic vein thrombosis pathophysiology On the Web |
|
American Roentgen Ray Society Images of Splenic vein thrombosis pathophysiology |
|
Risk calculators and risk factors for Splenic vein thrombosis pathophysiology |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1] ; Associate Editor(s)-in-Chief: Vindhya BellamKonda, M.B.B.S [2]
Overview
Splenic vein thrombosis in acute or chronic pancreatitis results from perivenous inflammation caused by the anatomic location of the splenic vein along the entire posterior aspect of the pancreatic tail, where it lies in direct contact with the peripancreatic inflammatory tissue. The exact mechanism of thrombosis is likely multi factorial, including both intrinsic endothelial damage from inflammatory or neoplastic processes and extrinsic damage secondary to venous compression from fibrosis, adjacent pseudo cysts, or edema.
Structure
The splenic vein is a blood vessel that drains blood from the spleen, the stomach fundus and part of the pancreas. It is part of the hepatic portal system. It follows a course superior to the pancreas, alongside the splenic artery. It collects branches from the stomach and pancreas, and most notably from the large intestine (also drained by the superior mesenteric vein) via the inferior mesenteric vein, which drains in the splenic vein shortly before the origin of the hepatic portal vein. The portal vein is formed when the splenic vein joins the superior mesenteric vein.
Pathophysiology
Pathogenesis
- It is thought that vein thrombosis is caused by Virchow's triad which includes:[1]
- Reduced portal blood flow
- Hypercoagulable state
- Vascular endothelial injury
<figure-inline>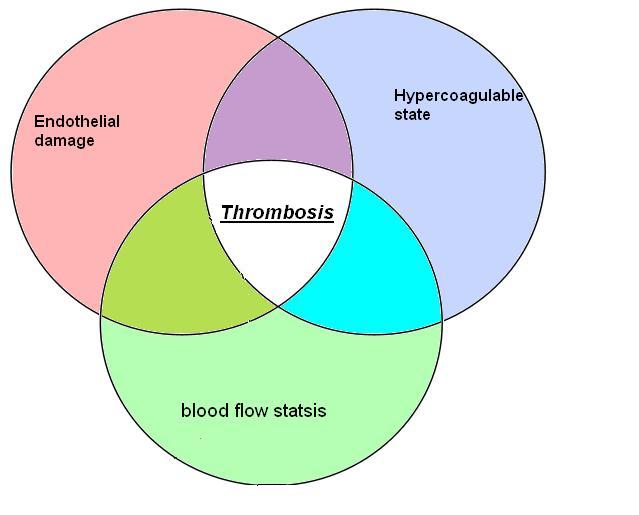
Shown below is a table depicting the elements of Virchow's triad and their modern counterparts.
| Virchow's[2] | Modern | Notes |
|---|---|---|
| Phenomena of interrupted blood-flow | "Stasis" or "venous stasis"[3] |
|
| Phenomena associated with irritation of the vessel and its vicinity | "Endothelial injury" or "vessel wall injury" |
|
| Phenomena of blood-coagulation | "Hypercoagulability" |
|
- Splenic vein thrombosis in acute or chronic pancreatitis results from acute inflammation
- The pathophysiology of thrombosis is likely multi factorial,
- Endothelial damage from inflammatory or neoplastic process is also one of the mechanism reported
- Another mechanism known to cause thrombosis is extrinsic damage secondary to venous compression from fibrosis, adjacent pseudo cysts, or edema.
- Obstruction of the splenic vein caused by enlarged retro peritoneal lymph nodes or by pancreatic or perisplenic nodes which are located near the splenic artery,above the splenic vein
located near the splenic artery, superior to the splenic vein.
- These nodes lie adjacent to the pancreas and splenic vein and compress the splenic vein when involved in an inflammatory or neoplastic process.
- When thrombosis of the splenic vein occurs, collateral vessels develop to shunt blood around the occluded splenic vein. The two most common collateral pathways use the short gastric vessels.
- In the distal esophagus, portosystemic collaterals connect the short gastric veins into the azygous system. *Splenoportal collaterals decompress the short gastric veins through both the coronary vein into the portal vein and via the gastroepiploic arcade into the superior mesenteric vein. In either case, the hypertensive short gastric veins cause increased pressure within the submucosal veins of
the gastric fundus, resulting in varices. In contrast to generalized portal hypertension, in splenic vein thrombosis flow in the coronary vein is hepatopetal rather than hepatofugal.
- At times, an enlarged gastroepiploic vein found at laparotomy may be the only indicator of occult splenic vein thrombosis. Isolated esophageal varices, although uncommon in SVT, can occur in cases in which the coronary vein joins the splenic vein proximal to the obstruction. This anatomic variant has been reported to occur in 17 % of the cases.
- Less common collateral pathways may also develop to decompress the splenic vein. The left gastroepiploic vein can collateralize to the left colic and inferior mesenteric veins. Although rare, this development has been reported to result in colonic variceal hemorrhage. Other collateral venous channels may develop via the diaphragmatic and intercostal veins to the inferior vena cava .The splenic vein may also collateralize to the renal vein via the adrenal vein.
Genetics
The exact genetics of splenic vein thrombosis is not fully understood
Associated conditions
The conditions associated with splenic vein thrombosis include:
- Pancreatitis
- Genetic disorders such as Factor V Leiden mutations
- Thrombophilias
- Abdominal trauma
Gross pathology
- There is no finding on gross pathology of Splenic vein thrombosis.
Microscopic pathology
- There is no finding on microscopic histopathological analysis.
References
- ↑ Chawla YK, Bodh V (2015). "Portal vein thrombosis". J Clin Exp Hepatol. 5 (1): 22–40. doi:10.1016/j.jceh.2014.12.008. PMC 4415192. PMID 25941431.
- ↑ Agutter, Paul S. (2008). The Aetiology of Deep Venous Thrombosis: A Critical, Historical and Epistemological Survey. Berlin: Springer. p. 84. ISBN 1-4020-6649-X.
- ↑ Lowe GD (2003). "Virchow's triad revisited: abnormal flow". Pathophysiol. Haemost. Thromb. 33 (5–6): 455–7. doi:10.1159/000083845. PMID 15692260.
- ↑ "Further reflections on Virchow's triad. - Free Online Library". Retrieved 2009-02-10.
- ↑ Chung I, Lip GY (2003). "Virchow's triad revisited: blood constituents". Pathophysiol. Haemost. Thromb. 33 (5–6): 449–54. doi:10.1159/000083844. PMID 15692259.