Smoking cessation: Difference between revisions
m (Protected "Smoking cessation": Protecting pages from unwanted edits ([edit=sysop] (indefinite) [move=sysop] (indefinite))) |
|||
| (14 intermediate revisions by 5 users not shown) | |||
| Line 1: | Line 1: | ||
{{CMG}} | __NOTOC__ | ||
{{SI}} | |||
{{ | {{CMG}};{{AE}}{{SMP}},{{USAMA}},{{AKI}} | ||
'''To review the wikidoc chapter on [[smoking]], click [[Smoking|here]]. | |||
==Overview== | ==Overview== | ||
[[ | [[Tobacco]] use is the leading cause of preventable disease, disability, and death in the United States. Each year, nearly half a million Americans die prematurely of smoking or exposure to secondhand smoke and 16 million live with a serious illness caused by [[smoking]]. [[Smoking]] can cause repairable damage to various organs including the [[heart]], [[lungs]], [[kidneys]], [[stomach]] and [[intestines]]. [[Smoking]] is associated with the causation of various cancers in the humans. Quitting [[smoking]] cuts [[cardiovascular]] risks, reduces risk for stroke to about half that of a nonsmoker’s, reduces risks for cancers of the [[mouth]], [[throat]], [[esophagus]], and [[bladder]] by half within 5 years and ten years after quitting [[smoking]], the risk for lung cancer drops by half. [[Smoking cessation]] can be achieved by some general, non-pharmacological and pharmacological strategies. | ||
==Clinical practice guidelines== | |||
Clinical practice guidelines by the [[USPSTF]] recommend<ref>USPSTF (2015). [https://www.uspreventiveservicestaskforce.org/Page/Document/UpdateSummaryFinal/tobacco-use-in-adults-and-pregnant-women-counseling-and-interventions1?ds=1&s=smoking%20cessation Tobacco Smoking Cessation in Adults, Including Pregnant Women: Behavioral and Pharmacotherapy Interventions]</ref>: | |||
* "Adults who are not pregnant: The USPSTF recommends that clinicians ask all adults about tobacco use, advise them to stop using tobacco, and provide behavioral interventions and U.S. Food and Drug Administration – approved pharmacotherapy for cessation to adults who use tobacco. GRADE A" | |||
* "Pregnant women: The USPSTF recommends that clinicians ask all pregnant woment about tobacco use, advise them to stop using tobacco, and provide behavioral interventions for cessation to pregnant women who use tobacco. GRADE A" | |||
* "Pregnant women: The USPSTF concludes that the current evidence is insufficient ot assess the balance of benefits and harms of pharmacotherpay interventions for tobacco cessation in pregnant women. GRADE I" | |||
* "All adults, including pregnant women: The USPSTF concludes that the current evidence is insufficient to recommend electronic nicotine delivery systems for tobacco cessation in adults, incuding pregnant women. The USPSTF recommends that clinicians direct patients who smoke tobacco to other cessation interventions with established effectiveness and safety. GRADE I" | |||
Tobacco | ==Smoking and Health== | ||
The impact of smoking on the health can be summarized as follows:<ref name="urlCDC - 2010 Surgeon Generals Report - Consumer Booklet - Smoking & Tobacco Use">{{cite web |url=https://www.cdc.gov/tobacco/data_statistics/sgr/2010/consumer_booklet/index.htm |title=CDC - 2010 Surgeon General's Report - Consumer Booklet - Smoking & Tobacco Use |format= |work= |accessdate=}}</ref><ref name="urlQuickStats: Number of Deaths from 10 Leading Causes — National Vital Statistics System, United States, 2010">{{cite web |url=https://www.cdc.gov/mmwr/preview/mmwrhtml/mm6208a8.htm?s_cid=mm6208a8_w |title=QuickStats: Number of Deaths from 10 Leading Causes — National Vital Statistics System, United States, 2010 |format= |work= |accessdate=}}</ref><ref name="urlCDC - 2014 Surgeon Generals Report - Smoking & Tobacco Use">{{cite web |url=https://www.cdc.gov/tobacco/data_statistics/sgr/50th-anniversary/index.htm |title=CDC - 2014 Surgeon General's Report - Smoking & Tobacco Use |format= |work= |accessdate=}}</ref> | |||
[[image:Smoke.jpg|center]] | |||
=== | ===Effect of Smoking Cessation on various Risks=== | ||
[[ | *Quitting [[smoking]] cuts cardiovascular risks<ref name="pmid31429895">{{cite journal| author=Duncan MS, Freiberg MS, Greevy RA, Kundu S, Vasan RS, Tindle HA| title=Association of Smoking Cessation With Subsequent Risk of Cardiovascular Disease. | journal=JAMA | year= 2019 | volume= 322 | issue= 7 | pages= 642-650 | pmid=31429895 | doi=10.1001/jama.2019.10298 | pmc=6704757 | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=31429895 }} </ref>. Just 1 year after quitting smoking, your risk for a heart attack drops sharply. | ||
*Within 2 to 5 years after quitting smoking, your risk for stroke may reduce to about that of a nonsmoker’s. | |||
*If you quit [[smoking]], your risks for cancers of the [[mouth]], [[throat]], [[esophagus]], and bladder drop by half within 5 years. | |||
*Ten years after you quit [[smoking]], your risk for lung cancer drops by half. | |||
==Smoking cessation== | |||
===General Principles=== | |||
The 5As are an evidence-based framework for structuring smoking cessation in health care settings. The 5As include: '''''Ask, Assess, Advise, Assist and Arrange follow-up'''''. | |||
* | <br> | ||
<br> | |||
{| align=center | |||
* | |- | ||
* | | | ||
{| style="border: 0px; font-size: 90%; margin: 3px;" align=center | |||
!align="center" style="background:#4479BA; color: #FFFFFF;" |The 5As | |||
!align="center" style="background:#4479BA; color: #FFFFFF;" |Technique | |||
|- | |||
|align="center" style="background:#DCDCDC;"|'''A'''sk | |||
|style="padding: 5px 5px; background: #F5F5F5;" align="left" |Identify and document tobacco use status for every patient at every visit | |||
|- | |||
|align="center" style="background:#DCDCDC;"|'''A'''dvise | |||
|style="padding: 5px 5px; background: #F5F5F5;" align="left" |In a clear, strong, and personalized manner, urge every [[tobacco]] user to quit. | |||
Advices should be: | |||
* Clear: | |||
** I think it is important for you to quit smoking now and I can help you. Cutting down while you are ill is not enough. | |||
* Strong: | |||
** As your clinician, I need you to know that quitting smoking is the most important thing you can do to protect your health now and in the future. The clinic staff and I will help you. | |||
* Personalized: | |||
** Tie tobacco use to current health, and its social and economic costs, motivation level to quit, and the impact of [[tobacco]] use on children and others in the household. | |||
|- | |||
|align="center" style="background:#DCDCDC;"|'''A'''ssess | |||
|style="padding: 5px 5px; background: #F5F5F5;" align="left" |Assess willingness to make a quit attempt. | |||
* Is the [[tobacco]] user willing to make a quit attempt within the next 30 days? | |||
|- | |||
|align="center" style="background:#DCDCDC;"|'''A'''ssist | |||
|style="padding: 5px 5px; background: #F5F5F5;" align="left" | | |||
* For the patient willing to make a quit attempt, offer medication and provide or refer for counseling or additional treatment to help the patient quit. | |||
* For patients unwilling to quit at the time, provide interventions designed to increase future quit attempts. | |||
|- | |||
* | |align="center" style="background:#DCDCDC;"|'''A'''rrange follow-up | ||
|style="padding: 5px 5px; background: #F5F5F5;" align="left" | | |||
* For the patient willing to make a quit attempt, arrange for followup contacts, beginning within the first week after the quit date. | |||
* | |||
* For patients unwilling to make a quit attempt at the time, address tobacco dependence and willingness to quit at next clinic visit. | |||
|} | |||
|} | |||
===Pharmacological=== | |||
First-line pharmacotherapy includes the multiple forms of nicotine replacement therapy (patch, nasal spray, losenge, gum, inhaler), sustained- release [[Bupropion extended release|bupropion]] hydrochloride, and [[varenicline]]. Second line therapy includes [[clonidine]] and [[nortriptyline]] and have been found to be efficacious.<ref name="urlwww.vapremier.com">{{cite web |url=https://www.vapremier.com/assets/SmokingCessationGuideline.pdf |title=www.vapremier.com |format= |work= |accessdate=}}</ref><br> | |||
'''The following is a description of the various treatment modalities available:'''<ref name="pmid18617085">{{cite journal| author=Clinical Practice Guideline Treating Tobacco Use and Dependence 2008 Update Panel, Liaisons, and Staff| title=A clinical practice guideline for treating tobacco use and dependence: 2008 update. A U.S. Public Health Service report. | journal=Am J Prev Med | year= 2008 | volume= 35 | issue= 2 | pages= 158-76 | pmid=18617085 | doi=10.1016/j.amepre.2008.04.009 | pmc=4465757 | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=18617085 }} </ref> | |||
*'''[[Bupropion extended release|Sustained release bupropion]] hydrochloride:''' | |||
**Dose: 150 mg every morning for 3 days, then 150 mg twice daily. | |||
**Duration: The duration of treatment is 7–12 weeks followed by a maintenance therapy up to 6 months. | |||
**Adverse effects: [[Insomnia]] and [[dry mouth]]. | |||
**Treatment must be initiated 1-2 weeks prior to the quit date. | |||
** Number needed to treat: 22<ref name="pmid27158893">{{cite journal| author=Cahill K, Lindson-Hawley N, Thomas KH, Fanshawe TR, Lancaster T| title=Nicotine receptor partial agonists for smoking cessation. | journal=Cochrane Database Syst Rev | year= 2016 | volume= | issue= 5 | pages= CD006103 | pmid=27158893 | doi=10.1002/14651858.CD006103.pub7 | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=27158893 }} </ref> | |||
*'''[[Nicotine]] gum:''' | |||
**Dose: 1–24 cigarettes/day: 2mg gum (up to 24 pieces/day). ≥ 25 cigarettes/day: 4 mg gum (up to 24 pieces/day). | |||
**Duration: Up to 12 weeks | |||
**Adverse effects: Mouth soreness and [[dyspepsia]] | |||
*'''[[Nicotine (inhalant)|Nicotine inhaler]]:''' | |||
**Dose: 6–16 cartridges/day | |||
**Duration: Up to 6 months | |||
**Adverse effects: Local irritation of [[mouth]] and throat | |||
*'''[[Nicotine]] lozenges:''' | |||
**Dose: Time to 1st cigarette > 30 min: 2 mg lozenge. Time to 1st cigarette ≤ 30 min: 4 mg lozenge. 4–20 lozenges/day can be used based on the need. | |||
**Duration: Up to 12 weeks | |||
**Adverse effects: [[Nausea and vomiting|Nausea]] and [[heartburn]] | |||
*'''[[Nicotine]] nasal spray:''' | |||
**Dose: 8–40 doses/day | |||
**Duration: 3–6 months | |||
**Adverse effects: Nasal irritation | |||
*'''[[Varenicline]]:''' | |||
**Dose: 0.5 mg/day for 3 days followed by 0.5 mg twice/day for 4 days. Then, 1 mg twice/day | |||
**Duration: 3–6 months | |||
**Adverse effects: [[Nausea and vomiting|Nausea]], [[Sleeping difficulty|trouble sleeping]], vivid/strange dreams and [[depressed mood]] | |||
** Number needed to treat: 11<ref name="pmid27158893">{{cite journal| author=Cahill K, Lindson-Hawley N, Thomas KH, Fanshawe TR, Lancaster T| title=Nicotine receptor partial agonists for smoking cessation. | journal=Cochrane Database Syst Rev | year= 2016 | volume= | issue= 5 | pages= CD006103 | pmid=27158893 | doi=10.1002/14651858.CD006103.pub7 | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=27158893 }} </ref> | |||
===Cost-effectiveness=== | |||
The cost per year of life save from smoking cessation<ref name="pmid9388153">{{cite journal| author=Cromwell J, Bartosch WJ, Fiore MC, Hasselblad V, Baker T| title=Cost-effectiveness of the clinical practice recommendations in the AHCPR guideline for smoking cessation. Agency for Health Care Policy and Research. | journal=JAMA | year= 1997 | volume= 278 | issue= 21 | pages= 1759-66 | pmid=9388153 | doi= | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=9388153 }} </ref><ref name="pmid16706571">{{cite journal| author=Kaper J, Wagena EJ, van Schayck CP, Severens JL| title=Encouraging smokers to quit: the cost effectiveness of reimbursing the costs of smoking cessation treatment. | journal=Pharmacoeconomics | year= 2006 | volume= 24 | issue= 5 | pages= 453-64 | pmid=16706571 | doi=10.2165/00019053-200624050-00004 | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=16706571 }} </ref> is less than the costs per year of life saved from [[lung cancer screening |screening for lung cancer]] with low-dose [[computed tomography]]<ref name="pmid31683314">{{cite journal| author=Criss SD, Cao P, Bastani M, Ten Haaf K, Chen Y, Sheehan DF et al.| title=Cost-Effectiveness Analysis of Lung Cancer Screening in the United States: A Comparative Modeling Study. | journal=Ann Intern Med | year= 2019 | volume= | issue= | pages= | pmid=31683314 | doi=10.7326/M19-0322 | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=31683314 }} </ref><ref name="pmid25372087">{{cite journal| author=Black WC, Gareen IF, Soneji SS, Sicks JD, Keeler EB, Aberle DR et al.| title=Cost-effectiveness of CT screening in the National Lung Screening Trial. | journal=N Engl J Med | year= 2014 | volume= 371 | issue= 19 | pages= 1793-802 | pmid=25372087 | doi=10.1056/NEJMoa1312547 | pmc=4335305 | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=25372087 }} [https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=&cmd=prlinks&id=25715973 Review in: Evid Based Med. 2015 Apr;20(2):78] </ref>. | |||
==See also== | ==See also== | ||
| Line 93: | Line 112: | ||
*[[Tobacco cessation clinic]] | *[[Tobacco cessation clinic]] | ||
*[[Tobacco and health]] | *[[Tobacco and health]] | ||
==References== | ==References== | ||
{{reflist|2}} | |||
[[Category:Tobacco cessation| ]] | [[Category:Tobacco cessation| ]] | ||
| Line 133: | Line 122: | ||
[[Category:Tobacco]] | [[Category:Tobacco]] | ||
{{jb1}} | {{jb1}} | ||
{{WikiDoc Help Menu}} | {{WikiDoc Help Menu}} | ||
{{WikiDoc Sources}} | {{WikiDoc Sources}} | ||
Latest revision as of 21:27, 25 January 2020
|
WikiDoc Resources for Smoking cessation |
|
Articles |
|---|
|
Most recent articles on Smoking cessation Most cited articles on Smoking cessation |
|
Media |
|
Powerpoint slides on Smoking cessation |
|
Evidence Based Medicine |
|
Cochrane Collaboration on Smoking cessation |
|
Clinical Trials |
|
Ongoing Trials on Smoking cessation at Clinical Trials.gov Trial results on Smoking cessation Clinical Trials on Smoking cessation at Google
|
|
Guidelines / Policies / Govt |
|
US National Guidelines Clearinghouse on Smoking cessation NICE Guidance on Smoking cessation
|
|
Books |
|
News |
|
Commentary |
|
Definitions |
|
Patient Resources / Community |
|
Patient resources on Smoking cessation Discussion groups on Smoking cessation Patient Handouts on Smoking cessation Directions to Hospitals Treating Smoking cessation Risk calculators and risk factors for Smoking cessation
|
|
Healthcare Provider Resources |
|
Causes & Risk Factors for Smoking cessation |
|
Continuing Medical Education (CME) |
|
International |
|
|
|
Business |
|
Experimental / Informatics |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1];Associate Editor(s)-in-Chief: Seyedmahdi Pahlavani, M.D. [2],Usama Talib, BSc, MD [3],Aravind Kuchkuntla, M.B.B.S[4]
To review the wikidoc chapter on smoking, click here.
Overview
Tobacco use is the leading cause of preventable disease, disability, and death in the United States. Each year, nearly half a million Americans die prematurely of smoking or exposure to secondhand smoke and 16 million live with a serious illness caused by smoking. Smoking can cause repairable damage to various organs including the heart, lungs, kidneys, stomach and intestines. Smoking is associated with the causation of various cancers in the humans. Quitting smoking cuts cardiovascular risks, reduces risk for stroke to about half that of a nonsmoker’s, reduces risks for cancers of the mouth, throat, esophagus, and bladder by half within 5 years and ten years after quitting smoking, the risk for lung cancer drops by half. Smoking cessation can be achieved by some general, non-pharmacological and pharmacological strategies.
Clinical practice guidelines
Clinical practice guidelines by the USPSTF recommend[1]:
- "Adults who are not pregnant: The USPSTF recommends that clinicians ask all adults about tobacco use, advise them to stop using tobacco, and provide behavioral interventions and U.S. Food and Drug Administration – approved pharmacotherapy for cessation to adults who use tobacco. GRADE A"
- "Pregnant women: The USPSTF recommends that clinicians ask all pregnant woment about tobacco use, advise them to stop using tobacco, and provide behavioral interventions for cessation to pregnant women who use tobacco. GRADE A"
- "Pregnant women: The USPSTF concludes that the current evidence is insufficient ot assess the balance of benefits and harms of pharmacotherpay interventions for tobacco cessation in pregnant women. GRADE I"
- "All adults, including pregnant women: The USPSTF concludes that the current evidence is insufficient to recommend electronic nicotine delivery systems for tobacco cessation in adults, incuding pregnant women. The USPSTF recommends that clinicians direct patients who smoke tobacco to other cessation interventions with established effectiveness and safety. GRADE I"
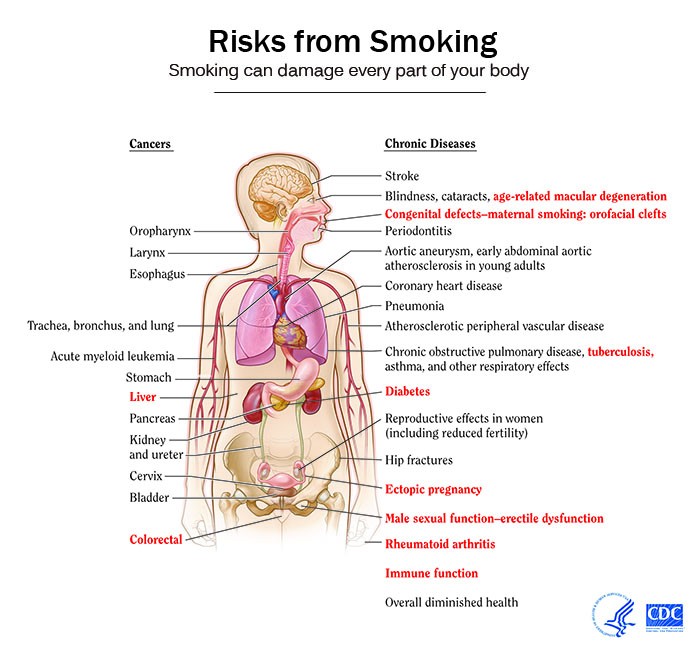
Smoking and Health
The impact of smoking on the health can be summarized as follows:[2][3][4]
Effect of Smoking Cessation on various Risks
- Quitting smoking cuts cardiovascular risks[5]. Just 1 year after quitting smoking, your risk for a heart attack drops sharply.
- Within 2 to 5 years after quitting smoking, your risk for stroke may reduce to about that of a nonsmoker’s.
- If you quit smoking, your risks for cancers of the mouth, throat, esophagus, and bladder drop by half within 5 years.
- Ten years after you quit smoking, your risk for lung cancer drops by half.
Smoking cessation
General Principles
The 5As are an evidence-based framework for structuring smoking cessation in health care settings. The 5As include: Ask, Assess, Advise, Assist and Arrange follow-up.
|
Pharmacological
First-line pharmacotherapy includes the multiple forms of nicotine replacement therapy (patch, nasal spray, losenge, gum, inhaler), sustained- release bupropion hydrochloride, and varenicline. Second line therapy includes clonidine and nortriptyline and have been found to be efficacious.[6]
The following is a description of the various treatment modalities available:[7]
- Sustained release bupropion hydrochloride:
- Nicotine gum:
- Dose: 1–24 cigarettes/day: 2mg gum (up to 24 pieces/day). ≥ 25 cigarettes/day: 4 mg gum (up to 24 pieces/day).
- Duration: Up to 12 weeks
- Adverse effects: Mouth soreness and dyspepsia
- Nicotine inhaler:
- Dose: 6–16 cartridges/day
- Duration: Up to 6 months
- Adverse effects: Local irritation of mouth and throat
- Nicotine lozenges:
- Nicotine nasal spray:
- Dose: 8–40 doses/day
- Duration: 3–6 months
- Adverse effects: Nasal irritation
- Varenicline:
- Dose: 0.5 mg/day for 3 days followed by 0.5 mg twice/day for 4 days. Then, 1 mg twice/day
- Duration: 3–6 months
- Adverse effects: Nausea, trouble sleeping, vivid/strange dreams and depressed mood
- Number needed to treat: 11[8]
Cost-effectiveness
The cost per year of life save from smoking cessation[9][10] is less than the costs per year of life saved from screening for lung cancer with low-dose computed tomography[11][12].
See also
- Nicotine Anonymous
- Health promotion
- NicVAX
- Nicotine replacement therapy
- Tobacco cessation clinic
- Tobacco and health
References
- ↑ USPSTF (2015). Tobacco Smoking Cessation in Adults, Including Pregnant Women: Behavioral and Pharmacotherapy Interventions
- ↑ "CDC - 2010 Surgeon General's Report - Consumer Booklet - Smoking & Tobacco Use".
- ↑ "QuickStats: Number of Deaths from 10 Leading Causes — National Vital Statistics System, United States, 2010".
- ↑ "CDC - 2014 Surgeon General's Report - Smoking & Tobacco Use".
- ↑ Duncan MS, Freiberg MS, Greevy RA, Kundu S, Vasan RS, Tindle HA (2019). "Association of Smoking Cessation With Subsequent Risk of Cardiovascular Disease". JAMA. 322 (7): 642–650. doi:10.1001/jama.2019.10298. PMC 6704757 Check
|pmc=value (help). PMID 31429895. - ↑ "www.vapremier.com" (PDF).
- ↑ Clinical Practice Guideline Treating Tobacco Use and Dependence 2008 Update Panel, Liaisons, and Staff (2008). "A clinical practice guideline for treating tobacco use and dependence: 2008 update. A U.S. Public Health Service report". Am J Prev Med. 35 (2): 158–76. doi:10.1016/j.amepre.2008.04.009. PMC 4465757. PMID 18617085.
- ↑ 8.0 8.1 Cahill K, Lindson-Hawley N, Thomas KH, Fanshawe TR, Lancaster T (2016). "Nicotine receptor partial agonists for smoking cessation". Cochrane Database Syst Rev (5): CD006103. doi:10.1002/14651858.CD006103.pub7. PMID 27158893.
- ↑ Cromwell J, Bartosch WJ, Fiore MC, Hasselblad V, Baker T (1997). "Cost-effectiveness of the clinical practice recommendations in the AHCPR guideline for smoking cessation. Agency for Health Care Policy and Research". JAMA. 278 (21): 1759–66. PMID 9388153.
- ↑ Kaper J, Wagena EJ, van Schayck CP, Severens JL (2006). "Encouraging smokers to quit: the cost effectiveness of reimbursing the costs of smoking cessation treatment". Pharmacoeconomics. 24 (5): 453–64. doi:10.2165/00019053-200624050-00004. PMID 16706571.
- ↑ Criss SD, Cao P, Bastani M, Ten Haaf K, Chen Y, Sheehan DF; et al. (2019). "Cost-Effectiveness Analysis of Lung Cancer Screening in the United States: A Comparative Modeling Study". Ann Intern Med. doi:10.7326/M19-0322. PMID 31683314.
- ↑ Black WC, Gareen IF, Soneji SS, Sicks JD, Keeler EB, Aberle DR; et al. (2014). "Cost-effectiveness of CT screening in the National Lung Screening Trial". N Engl J Med. 371 (19): 1793–802. doi:10.1056/NEJMoa1312547. PMC 4335305. PMID 25372087. Review in: Evid Based Med. 2015 Apr;20(2):78