|
|
| Line 20: |
Line 20: |
| {{SK}} hypocortisolism; hypocorticism; adrenocortical hypofunction | | {{SK}} hypocortisolism; hypocorticism; adrenocortical hypofunction |
|
| |
|
| ==Overview== | | ==[[Adrenal insufficiency overview|Overview]]== |
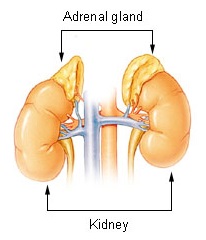
| Adrenal insufficiency is a condition in which the [[adrenal gland]]s, located above the [[kidney]]s, do not produce adequate amounts of [[steroid hormone]]s (chemicals produced by the body that regulate organ function), primarily [[cortisol]], but may also include impaired [[aldosterone]] production (a [[mineralocorticoid]]) which regulates [[sodium]], [[potassium]] and water retention.<ref name="addisons_disease.aspx">{{cite journal | author=Eileen K. Corrigan |title=Adrenal Insufficiency (Secondary Addison's or Addison's Disease)|journal=NIH Publication No. 90-3054 |year=2007 |url=http://www.pituitary.org/disorders/addisons_disease.aspx}}</ref><ref>{{MeshName|Adrenal+Insufficiency}}</ref> Craving for salt or salty foods due to the urinary losses of sodium is common.<ref name="PMID 11443143">{{cite journal |author=Ten S, New M, Maclaren N |title=Clinical review 130: Addison's disease 2001 |journal=J. Clin. Endocrinol. Metab. |volume=86 |issue=7 | pages=2909–22 |year=2001 |pmid=11443143 |url=http://jcem.endojournals.org/cgi/content/full/86/7/2909 |doi=10.1210/jc.86.7.2909}}</ref> | |
|
| |
|
| Adrenal insufficiency can also occur when the [[hypothalamus]] or the [[pituitary gland]], both located at the base of the [[Human skull|skull]], does not make adequate amounts of the hormones that assist in regulating adrenal function.<ref name="addisons_disease.aspx"/><ref name="urlJAMA -- Adrenal Insufficiency, November 16, 2005, Brender et al. 294 (19): 2528">{{cite journal |author=Brender E, Lynm C, Glass RM |title=JAMA patient page. Adrenal insufficiency |journal=JAMA |volume=294 |issue=19 |page=2528 |year=2005 |pmid=16287965 |doi=10.1001/jama.294.19.2528 |url=http://jama.ama-assn.org/cgi/content/full/294/19/2528}}</ref><ref name="urlDorlands Medical Dictionary:adrenal insufficiency">{{cite web |url=http://www.mercksource.com/pp/us/cns/cns_hl_dorlands_split.jsp?pg=/ppdocs/us/common/dorlands/dorland/four/000053970.htm |title=Dorlands Medical Dictionary:adrenal insufficiency |work= |accessdate=}}</ref> This is called secondary adrenal insufficiency and is caused by lack of production of [[ACTH]] in the pituitary or lack of [[Corticotropin-releasing hormone|CRH]] in the hypothalamus.<ref name="urlSecondary Adrenal Insufficiency: Adrenal Disorders: Merck Manual Professional">{{cite web |url=http://www.merck.com/mmpe/sec12/ch153/ch153c.html |title=Secondary Adrenal Insufficiency: Adrenal Disorders: Merck Manual Professional |work= |accessdate=}}</ref>
| | ==[[Adrenal insufficiency historical perspective|Historical Perspective]]== |
|
| |
|
| ==Classification== | | ==[[Adrenal insufficiency pathophysiology|Pathophysiology]]== |
| There are three major types of adrenal insufficiency.
| |
|
| |
|
| * '''Primary adrenal insufficiency''' is due to impairment of the adrenal glands.
| | ==[[Adrenal insufficiency causes|Causes]]== |
| ** One subtype is called [[idiopathic]] or unknown cause of adrenal insufficiency.
| |
| ** 80% are due to an [[autoimmune disease]] called [[Addison's disease]] or [[autoimmune adrenalitis]].
| |
| ** Other cases are due to [[congenital adrenal hyperplasia]] or an [[adenoma]] (tumor) of the adrenal gland.
| |
| * '''Secondary adrenal insufficiency''' is caused by impairment of the [[pituitary gland]] or [[hypothalamus]].<ref name="Hypopituitary">{{cite web |url=http://www.webmd.com/a-to-z-guides/hypopituitary |title=hypopituitary |year=2006}}</ref> The most common cause in the United States is exogenous steroid use. Other causes are a [[pituitary adenoma]] or [[microadenoma]], [[hypothalamic tumor]] (surgical removal of a pituitary tumor can also suppress production of ACTH and lead to adrenal deficiency); [[Sheehan's syndrome]], which is associated with impairment of only the pituitary gland.
| |
| * '''Tertiary adrenal insufficiency''' is due to hypothalamic disease and decrease in [[corticotropin releasing factor]] (CRF).<ref>http://www.endotext.org/adrenal/adrenal13/adrenal13.htm</ref>
| |
|
| |
|
| ==Pathophysiology== | | ==[[Adrenal insufficiency differential diagnosis|Differentiating Adrenal insufficiency from other Diseases]]== |
| * '''Primary adrenal insufficiency''':
| |
| Here the defect lies in the [[adrenal glands]]. [[Autoantibodies]], [[infections]], [[drugs]] and [[mutations]] cause destruction of the [[adrenal glands]] leading to deficiency of adrenal hormones and thus causing symptoms.
| |
|
| |
|
| * '''Secondary adrenal insufficiency''':
| | ==[[Adrenal insufficiency epidemiology and demographics|Epidemiology and Demographics]]== |
| [[ACTH]] deficiency caused by diseases of the [[pituitary gland]] is the main cause for adrenal insufficiency. ACTH deficiency leads to loss of stimulus for the production of adrenal hormones. [[ACTH]] levels in the blood can differentiate primary adrenal insufficiency from the secondary form. In the primary form the ACTH levels are high because of the loss of negative feedback from the adrenal hormones.
| |
|
| |
|
| * '''Tertiary adrenal insufficiency''':
| | ==[[Adrenal insufficiency risk factors|Risk Factors]]== |
| The [[hypothalamus]] in the brain secretes a hormone called [[corticotropin releasing factor]] (CRF). This hormone provides the necessary stimulus to the [[pituitary]] for secreting [[ACTH]] which in turn activates the process of production of adrenal hormones. In diseases of the [[hypothalamus]], the CRF is not produced leading to a decreased production of ACTH and in turn the adrenal hormones.
| |
|
| |
|
| == Causes == | | ==[[Adrenal insufficiency natural history, complications and prognosis|Natural History, Complications and Prognosis]]== |
| ===Common Causes===
| |
| * '''Acute adrenal insufficiency'''
| |
| ** [[Addison's disease]] ([[autoimmune adrenalitis]])
| |
| ** [[Septic shock]]
| |
| ** [[Waterhouse-Friderichsen syndrome]]
| |
| ** [[Addison's disease#Addisonian crisis|Addisonian crisis]] in case of:
| |
| *** Discontinuing [[corticosteroid]] therapy without tapering the dosage
| |
| *** Surgery, illness or any other form of stress in patients with long-term [[corticosteroid]] therapy
| |
| * '''Chronic adrenal insufficiency'''
| |
| ** [[Addison's disease]]
| |
| ** [[Congenital adrenal hyperplasia|Congenital Adrenal Hyperplasia]]
| |
| ** [[Antiphospholipid syndrome]]
| |
| ** [[Haemochromatosis]]
| |
| | |
| ===Causes by Organ System===
| |
| {|style="width:80%; height:100px" border="1"
| |
| |style="height:100px"; style="width:25%" border="1" bgcolor="LightSteelBlue" | '''Cardiovascular'''
| |
| |style="height:100px"; style="width:75%" border="1" bgcolor="Beige" | [[Arteritis]], [[Hypotension]], [[Hemorrhage]], [[Infarction]]
| |
| |-
| |
| |-bgcolor="LightSteelBlue"
| |
| | '''Chemical / poisoning'''
| |
| |bgcolor="Beige"| No underlying causes
| |
| |-
| |
| |-bgcolor="LightSteelBlue"
| |
| | '''Dermatologic'''
| |
| |bgcolor="Beige"| [[POEMS syndrome]]
| |
| |-
| |
| |-bgcolor="LightSteelBlue"
| |
| | '''Drug Side Effect'''
| |
| |bgcolor="Beige"| [[Aminoglutethimide]], [[Corticosteroid]] withdrawal, [[Trilostane]]
| |
| |-
| |
| |-bgcolor="LightSteelBlue"
| |
| | '''Ear Nose Throat'''
| |
| |bgcolor="Beige"| No underlying causes
| |
| |-
| |
| |-bgcolor="LightSteelBlue"
| |
| | '''Endocrine'''
| |
| |bgcolor="Beige"| [[Allgrove syndrome]], [[Achalasia-addisonian syndrome]], [[Adrenal aplasia]] / [[adrenal hypoplasia]], [[Adrenal metastases]], After surgery of [[cortisol-secreting tumor]], [[Autoimmune polyendocrine syndrome type 2]], [[Bilateral adrenalectomy ]], [[Congenital adrenal hyperplasia]], [[Glucocorticoid deficiency 1]], [[IMAGE syndrome]], [[POEMS syndrome]], [[X-linked adrenal hypoplasia congenita]]
| |
| |-
| |
| |-bgcolor="LightSteelBlue"
| |
| | '''Environmental'''
| |
| |bgcolor="Beige"| No underlying causes
| |
| |-
| |
| |-bgcolor="LightSteelBlue"
| |
| | '''Gastroenterologic'''
| |
| |bgcolor="Beige"| [[Allgrove syndrome]], [[Achalasia-addisonian syndrome]], [[Hemochromatosis ]]
| |
| |-
| |
| |-bgcolor="LightSteelBlue"
| |
| | '''Genetic'''
| |
| |bgcolor="Beige"| [[Congenital adrenal hyperplasia]], [[Cytochrome P450 oxidoreductase deficiency]], [[Glycerol kinase deficiency]], [[Hereditary ACTH resistance]], [[IMAGE syndrome]], [[X-linked adrenal hypoplasia congenita]]
| |
| |-
| |
| |-bgcolor="LightSteelBlue"
| |
| | '''Hematologic'''
| |
| |bgcolor="Beige"| [[Anticoagulation]], [[Coagulopathy ]], [[Embolus]], [[Leukemia]], [[Lymphoma ]], [[Thrombosis]]
| |
| |-
| |
| |-bgcolor="LightSteelBlue"
| |
| | '''Iatrogenic'''
| |
| |bgcolor="Beige"| [[Iatrogenic]], [[Radiation therapy]]
| |
| |-
| |
| |-bgcolor="LightSteelBlue"
| |
| | '''Infectious Disease'''
| |
| |bgcolor="Beige"| [[AIDS]], [[Blastomycosis]], [[CMV]], [[Coccidiomycosis]], [[Cryptococcosis]], [[Histoplasmosis ]], [[Mycobacterium avium intracellulaire]] ([[MAI]]), [[Sepsis]], [[Syphilis]], [[Toxoplasmosis]], [[Tuberculosis]], [[Waterhouse-Friderichson syndrome ]]
| |
| |-
| |
| |-bgcolor="LightSteelBlue"
| |
| | '''Musculoskeletal / Ortho'''
| |
| |bgcolor="Beige"| [[IMAGE syndrome]]
| |
| |-
| |
| |-bgcolor="LightSteelBlue"
| |
| | '''Neurologic'''
| |
| |bgcolor="Beige"| [[Adrenoleukodystrophy]], [[Coma]], [[Craniopharyngioma]], [[Panhypopituitarism]], [[POEMS syndrome]]
| |
| |-
| |
| |-bgcolor="LightSteelBlue"
| |
| | '''Nutritional / Metabolic'''
| |
| |bgcolor="Beige"| No underlying causes
| |
| |-
| |
| |-bgcolor="LightSteelBlue"
| |
| | '''Obstetric/Gynecologic'''
| |
| |bgcolor="Beige"| No underlying causes
| |
| |-
| |
| |-bgcolor="LightSteelBlue"
| |
| | '''Oncologic'''
| |
| |bgcolor="Beige"| [[Craniopharyngioma]], [[Kaposi's sarcoma]], [[Leukemia]], [[Lymphoma ]]
| |
| |-
| |
| |-bgcolor="LightSteelBlue"
| |
| | '''Opthalmologic'''
| |
| |bgcolor="Beige"| No underlying causes
| |
| |-
| |
| |-bgcolor="LightSteelBlue"
| |
| | '''Overdose / Toxicity'''
| |
| |bgcolor="Beige"| No underlying causes
| |
| |-
| |
| |-bgcolor="LightSteelBlue"
| |
| | '''Psychiatric'''
| |
| |bgcolor="Beige"| No underlying causes
| |
| |-
| |
| |-bgcolor="LightSteelBlue"
| |
| | '''Pulmonary'''
| |
| |bgcolor="Beige"| [[Sarcoidosis]],
| |
| |-
| |
| |-bgcolor="LightSteelBlue"
| |
| | '''Renal / Electrolyte'''
| |
| |bgcolor="Beige"| [[Uremia]], [[Waterhouse-Friderichson syndrome ]]
| |
| |-
| |
| |-bgcolor="LightSteelBlue"
| |
| | '''Rheum / Immune / Allergy'''
| |
| |bgcolor="Beige"| [[Autoimmune]], [[Autoimmune polyendocrine syndrome type 2]], [[Sarcoidosis]]
| |
| |-
| |
| |-bgcolor="LightSteelBlue"
| |
| | '''Sexual'''
| |
| |bgcolor="Beige"| No underlying causes
| |
| |-
| |
| |-bgcolor="LightSteelBlue"
| |
| | '''Trauma'''
| |
| |bgcolor="Beige"| [[Trauma]]
| |
| |-
| |
| |-bgcolor="LightSteelBlue"
| |
| | '''Urologic'''
| |
| |bgcolor="Beige"| No underlying causes
| |
| |-
| |
| |-bgcolor="LightSteelBlue"
| |
| | '''Dental'''
| |
| |bgcolor="Beige"| No underlying causes
| |
| |-
| |
| |-bgcolor="LightSteelBlue"
| |
| | '''Miscellaneous'''
| |
| |bgcolor="Beige"| [[Amyloidosis]], [[Idiopathic]], [[Iatrogenic]], [[Radiation therapy]], [[Surgery]], Surgical removal of [[pituitary]], Surgical removal of [[hypothalamus]]
| |
| |-
| |
| |}
| |
| | |
| ===Causes in Alphabetical Order===
| |
| | |
| {{MultiCol}}
| |
| *[[Achalasia-addisonian syndrome]]<ref name="pmid11196451">{{cite journal |author=Huebner A, Yoon SJ, Ozkinay F, ''et al.'' |title=Triple A syndrome--clinical aspects and molecular genetics |journal=Endocr. Res. |volume=26 |issue=4 |pages=751–9 |year=2000 |month=November |pmid=11196451 |doi= |url=}}</ref>
| |
| *[[Adrenal aplasia]] / [[Adrenal hypoplasia]]
| |
| *[[Adrenal metastases]]
| |
| *[[Adrenoleukodystrophy]]<ref name="pmid8441467">{{cite journal |author=Mosser J, Douar AM, Sarde CO, ''et al.'' |title=Putative X-linked adrenoleukodystrophy gene shares unexpected homology with ABC transporters |journal=Nature |volume=361 |issue=6414 |pages=726–30 |year=1993 |month=February |pmid=8441467 |doi=10.1038/361726a0 |url=}}</ref>
| |
| *After surgery of [[cortisol-secreting tumor]]
| |
| *[[AIDS]]<ref name="pmid22629505">{{cite journal |author=Shashidhar PK, Shashikala GV |title=Low dose adrenocorticotropic hormone test and adrenal insufficiency in critically ill acquired immunodeficiency syndrome patients |journal=Indian J Endocrinol Metab |volume=16 |issue=3 |pages=389–94 |year=2012 |month=May |pmid=22629505 |pmc=3354846 |doi=10.4103/2230-8210.95680 |url=}}</ref><ref name="pmid11217816">{{cite journal |author=Eledrisi MS, Verghese AC |title=Adrenal insufficiency in HIV infection: a review and recommendations |journal=Am. J. Med. Sci. |volume=321 |issue=2 |pages=137–44 |year=2001 |month=February |pmid=11217816 |doi= |url=}}</ref>
| |
| *[[Allgrove syndrome]]<ref name="pmid11196451">{{cite journal |author=Huebner A, Yoon SJ, Ozkinay F, ''et al.'' |title=Triple A syndrome--clinical aspects and molecular genetics |journal=Endocr. Res. |volume=26 |issue=4 |pages=751–9 |year=2000 |month=November |pmid=11196451 |doi= |url=}}</ref>
| |
| *[[Aminoglutethimide]]
| |
| *[[Amyloidosis]]
| |
| *[[Anticoagulation]]
| |
| *[[Arteritis]]
| |
| *[[Autoimmune]]
| |
| *[[Autoimmune polyendocrine syndrome type 2]]<ref name="pmid22506635">{{cite journal |author=Cocco C, Meloni A, Mariotti S, ''et al.'' |title=Novel neuronal and endocrine autoantibody targets in autoimmune polyendocrine syndrome type 1 |journal=Autoimmunity |volume=45 |issue=6 |pages=485–94 |year=2012 |month=September |pmid=22506635 |doi=10.3109/08916934.2012.680632 |url=}}</ref>
| |
| *[[Bilateral adrenalectomy]]
| |
| *[[Blastomycosis]]<ref name="pmid6266250">{{cite journal |author=Osa SR, Peterson RE, Roberts RB |title=Recovery of adrenal reserve following treatment of disseminated South American blastomycosis |journal=Am. J. Med. |volume=71 |issue=2 |pages=298–301 |year=1981 |month=August |pmid=6266250 |doi= |url=}}</ref>
| |
| *[[CMV]]<ref name="pmid19765472">{{cite journal |author=Ardalan M, Shoja MM |title=Cytomegalovirus-induced adrenal insufficiency in a renal transplant recipient |journal=Transplant. Proc. |volume=41 |issue=7 |pages=2915–6 |year=2009 |month=September |pmid=19765472 |doi=10.1016/j.transproceed.2009.07.024 |url=}}</ref>
| |
| *[[Coagulopathy]]
| |
| *[[Coccidiomycosis]]
| |
| *[[Coma]]
| |
| *[[Congenital adrenal hyperplasia]]
| |
| *[[Corticosteroid]] withdrawal
| |
| *[[Craniopharyngioma]]<ref name="pmid18050601">{{cite journal |author=Mihalache A, Lamy O, Waeber G, Schneider A |title=[Adrenal insufficiency and hypercalcemia--an unusual presentation] |language=German |journal=Praxis (Bern 1994) |volume=96 |issue=45 |pages=1761–5 |year=2007 |month=November |pmid=18050601 |doi= |url=}}</ref>
| |
| *[[Cryptococcosis]]<ref name="pmid9671046">{{cite journal |author=Kawamura M, Miyazaki S, Mashiko S, ''et al.'' |title=Disseminated cryptococcosis associated with adrenal masses and insufficiency |journal=Am. J. Med. Sci. |volume=316 |issue=1 |pages=60–4 |year=1998 |month=July |pmid=9671046 |doi= |url=}}</ref>
| |
| *[[Cytochrome P450 oxidoreductase deficiency]]
| |
| *[[Embolus]]
| |
| *[[Glucocorticoid deficiency 1]]<ref name="pmid22337906">{{cite journal |author=Turan S, Hughes C, Atay Z, ''et al.'' |title=An atypical case of familial glucocorticoid deficiency without pigmentation caused by coexistent homozygous mutations in MC2R (T152K) and MC1R (R160W) |journal=J. Clin. Endocrinol. Metab. |volume=97 |issue=5 |pages=E771–4 |year=2012 |month=May |pmid=22337906 |pmc=3396854 |doi=10.1210/jc.2011-2414 |url=}}</ref>
| |
| *[[Glycerol kinase deficiency]]<ref name="pmid2883886">{{cite journal |author=Francke U, Harper JF, Darras BT, ''et al.'' |title=Congenital adrenal hypoplasia, myopathy, and glycerol kinase deficiency: molecular genetic evidence for deletions |journal=Am. J. Hum. Genet. |volume=40 |issue=3 |pages=212–27 |year=1987 |month=March |pmid=2883886 |pmc=1684111 |doi= |url=}}</ref>
| |
| *[[Hemochromatosis]]<ref name="pmid8650756">{{cite journal |author=Pedersen-Bjergaard U, Thorsteinsson B, Kirkegaard BC |title=[Pituitary function in hemochromatosis] |language=Danish |journal=Ugeskr. Laeg. |volume=158 |issue=13 |pages=1818–22 |year=1996 |month=March |pmid=8650756 |doi= |url=}}</ref>
| |
| {{ColBreak}}
| |
| *[[Hemorrhage]]
| |
| *[[Hereditary ACTH resistance]]
| |
| *[[Histoplasmosis]]
| |
| *[[Hypotension]]
| |
| *[[Iatrogenic]]
| |
| *[[Idiopathic]]
| |
| *[[IMAGE syndrome]]<ref name="pmid14760276">{{cite journal |author=Pedreira CC, Savarirayan R, Zacharin MR |title=IMAGe syndrome: a complex disorder affecting growth, adrenal and gonadal function, and skeletal development |journal=J. Pediatr. |volume=144 |issue=2 |pages=274–7 |year=2004 |month=February |pmid=14760276 |doi=10.1016/j.jpeds.2003.09.052 |url=}}</ref>
| |
| *[[Infarction]]
| |
| *[[Kaposi's sarcoma]]
| |
| *[[Leukemia]]
| |
| *[[Lymphoma]]
| |
| *[[Mycobacterium avium intracellulaire]] ([[MAI]])<ref name="pmid1758516">{{cite journal |author=Weits J, Sprenger HG, Ilic P, van Klingeren B, Elema JD, Steensma JT |title=[Mycobacterium avium disease in AIDS patients; diagnosis and therapy] |language=Dutch; Flemish |journal=Ned Tijdschr Geneeskd |volume=135 |issue=52 |pages=2485–9 |year=1991 |month=December |pmid=1758516 |doi= |url=}}</ref>
| |
| *[[Panhypopituitarism]]
| |
| *[[POEMS syndrome]]<ref name="pmid12456500">{{cite journal |author=Dispenzieri A, Kyle RA, Lacy MQ, ''et al.'' |title=POEMS syndrome: definitions and long-term outcome |journal=Blood |volume=101 |issue=7 |pages=2496–506 |year=2003 |month=April |pmid=12456500 |doi=10.1182/blood-2002-07-2299 |url=}}</ref>
| |
| *[[Radiation therapy]]
| |
| *[[Sarcoidosis]]<ref name="pmid16526262">{{cite journal |author=Gostiljac DM, Dordević PB, Maric-zivković J, Canović F |title=[Sarcoidosis localized in endocrine glands] |journal=Med. Pregl. |volume=58 Suppl 1 |issue= |pages=25–9 |year=2005 |pmid=16526262 |doi= |url=}}</ref>
| |
| *[[Sepsis]]
| |
| *[[Surgery]]
| |
| *Surgical removal of [[hypothalamus]]
| |
| *Surgical removal of [[pituitary]]
| |
| *[[Syphilis]]
| |
| *[[Thrombosis]]
| |
| *[[Toxoplasmosis]]
| |
| *[[Trauma]]
| |
| *[[Trilostane]]
| |
| *[[Tuberculosis]]
| |
| *[[Uremia]]
| |
| *[[Waterhouse-Friderichson syndrome ]]
| |
| *[[X-linked adrenal hypoplasia congenita]]
| |
| {{EndMultiCol}}
| |
| | |
| ==Differentiating Adrenal insufficiency from other Diseases==
| |
| Diseases with similar symptoms include:
| |
| * [[Riehl's melanosis]]
| |
| * [[Hepatic cirrhosis]]
| |
| * [[Hemochromatosis]]
| |
| * [[Acanthosis nigricans]]
| |
| | |
| ==Risk Factors==
| |
| The following conditions increase the risk of adrenal insufficiency:
| |
| | |
| * Genetic defects of [[adrenal gland]]
| |
| * Underactive [[parathyroid gland]]s
| |
| * [[Pernicious anemia]]
| |
| * Chronic [[fungal infection]]s
| |
| * [[Chronic active hepatitis]]
| |
| * [[Diabetes]]
| |
| * [[Vitiligo]]
| |
| * [[Tuberculosis]]
| |
| * [[Amyloidosis]]
| |
| * [[AIDS]]-associated [[infection]]s
| |
| * [[Cancer]]
| |
| | |
| ==Natural History, Complications and Prognosis==
| |
| ===Complications===
| |
| Complications of adrenal insufficiency include:
| |
| * Cardiac [[arrhythmias]] - due to [[hyperkalemia]]
| |
| * [[Psychosis]]
| |
| * [[Addisonian crisis]]
| |
| | |
| ===Prognosis===
| |
| The prognosis of adrenal insufficiency depends on:
| |
| * Whether the patient has received hormone replacement or not.
| |
| * When stress happens on the patients with adrenal insufficiency, whether the treatment protocols are adjusted or not.
| |
|
| |
|
| ==Diagnosis== | | ==Diagnosis== |
| ===Symptoms===
| | [[Adrenal insufficiency history and symptoms| History and Symptoms]] | [[Adrenal insufficiency physical examination | Physical Examination]] | [[Adrenal insufficiency laboratory findings|Laboratory Findings]] | [[Adrenal insufficiency electrocardiogram|Electrocardiogram]] | [[Adrenal insufficiency x ray|X Ray]] | [[Adrenal insufficiency CT|CT]] | [[Adrenal insufficiency MRI|MRI]] | [[Adrenal insufficiency echocardiography or ultrasound|Echocardiography or Ultrasound]] | [[Adrenal insufficiency other imaging findings|Other Imaging Findings]] | [[Adrenal insufficiency other diagnostic studies|Other Diagnostic Studies]] |
| There is often the slow insidious onset of the following symptoms:
| |
| * [[Dehydration]]
| |
| * [[Diarrhea]]
| |
| * [[Abdominal pain]]
| |
| * [[Disorientation]]
| |
| * [[Dizziness]]
| |
| * [[Muscle aches]]
| |
| * [[Nausea]]
| |
| * [[Tanning]] of the skin that may be patchy or even all over the body. Characteristic sites of tanning are skin creases (e.g. of the hands) and the inside of the cheek ([[buccal mucosa]]).
| |
| * [[Tiredness]] - [[fatigue]]
| |
| * [[Vomiting]]
| |
| * [[Weakness]]
| |
| * [[Weight loss]]
| |
| | |
| ===Physical Examination===
| |
| ====Appearance====
| |
| * The patient may be [[dehydrated]] and [[lethargic]].
| |
| | |
| ====Vital Signs====
| |
| * [[Hypotension|Low blood pressure]] that falls further when standing ([[orthostatic hypotension]])
| |
| * [[Cardiovascular collapse]] may be present
| |
| | |
| ====Skin====
| |
| * There can be tanning of the skin. [[Tanning]] of the skin that may be patchy or even all over the body. Characteristic sites of tanning are skin creases (e.g. of the hands) and the inside of the cheek ([[buccal mucosa]]).
| |
| * [[Vitiligo]] may also be present.
| |
| * Absence of axillary and pubic hair in females as a result of loss of adrenal [[androgens]].
| |
| * [[Pallor]] may be present.
| |
| | |
| ====Neck====
| |
| * [[Goitre]] may be present
| |
| | |
| ===Extremities===
| |
| * [[Weakness]]
| |
| | |
| ===Neurologic===
| |
| * [[Confusion]] may be present
| |
| * [[Seizures]] may be present.
| |
| | |
| ===Laboratory Findings===
| |
| ====ACTH Stimulation Test====
| |
| If the person is in [[adrenal crisis]], the [[ACTH stimulation test]]<ref>{{cite journal|pmid=21656493 | doi=10.1024/0040-5930/a000174 | volume=68 | issue=6 | title=[Adrenal insufficiency--diagnosis and treatment in clinical practice] | year=2011 | month=June | author=Henzen C | journal=Ther Umsch | pages=337–43}}</ref> may be given. If not in crisis, cortisol, ACTH, aldosterone, [[renin]], potassium and sodium are tested from a blood sample before the decision is made if the ACTH stimulation test needs to be performed. X-rays or CT of the adrenals may also be done.<ref name="addisons_disease.aspx"/> The best test for adrenal insufficiency of autoimmune origin, representing more than ninety percent of all cases in a Western population, is measurement of 21-hydroxylase autoantibodies.
| |
| {| border="4" cellspacing="1" cellpadding="4" style="text-align:center; margin:10px;"
| |
| |-
| |
| | style="background:#ddcef2" | '''Source of pathology|| style="background:#cef2e0" |'''CRH|| style="background:#cef2e0" |'''ACTH|| style="background:#cef2e0" |'''DHEA|| style="background:#cef2e0" |'''DHEA-S|| style="background:#cef2e0" |'''cortisol||style="background:#cef2e0;" |'''aldosterone|| style="background:#cef2e0" |'''renin|| style="background:#cef2e0" |'''Na|| style="background:#cef2e0" |'''K|| style="background:#f2e0ce" |'''Causes'''<sup>5</sup>
| |
| |-
| |
| | style="background:#cedff2" | '''hypothalamus'''<br>(tertiary)<sup>1</sup>|| style="background:#F8F8F8" |low|| style="background:#F8F8F8"|low|| style="background:#F8F8F8" |low|| style="background:#F8F8F8" |low|| style="background:#F8F8F8" |low<sup>3</sup>||style="background:#F8F8F8" |low|| style="background:#F8F8F8" |low|| style="background:#F8F8F8" |low|| style="background:#F8F8F8" |low||style="background:#F8F8F8" |tumor of the hypothalamus ([[adenoma]]), [[antibodies]], [[environment (biophysical)|environment]] (i.e. toxins), [[head injury]]
| |
| |-
| |
| | style="background:#cedff2" | '''pituitary'''<br>(secondary)|| style="background:#F8F8F8" |high<sup>2</sup>|| style="background:#F8F8F8"|low|| style="background:#F8F8F8" |low|| style="background:#F8F8F8" |low|| style="background:#F8F8F8" |low<sup>3</sup>||style="background:#F8F8F8" |low|| style="background:#F8F8F8" |low|| style="background:#F8F8F8" |low|| style="background:#F8F8F8" |low||style="background:#F8F8F8" |tumor of the pituitary ([[adenoma]]), antibodies, environment, head injury,<br>'''surgical removal'''<sup>6</sup>, [[Sheehan's syndrome]]
| |
| |-
| |
| | style="background:#cedff2" | '''adrenal glands'''<br>(primary)<sup>7</sup>|| style="background:#F8F8F8" |high|| style="background:#F8F8F8"|high|| style="background:#F8F8F8" |high|| style="background:#F8F8F8" |high|| style="background:#F8F8F8" |low<sup>4</sup>||style="background:#F8F8F8" |low|| style="background:#F8F8F8" |high|| style="background:#F8F8F8" |low|| style="background:#F8F8F8" |high||style="background:#F8F8F8" |tumor of the adrenal (adenoma), [[Stress (biology)|stress]], antibodies, environment, [[Addison's Disease]], [[Physical trauma|trauma]], surgical removal ([[Segmental resection|resection]]), [[wikt:miliary|miliary]] [[tuberculosis]] of the adrenal
| |
| |}
| |
| | |
| {| border="2" cellspacing="1" cellpadding="2" style="margin:10px;"
| |
| |-
| |
| | '''1'''|| Automatically includes diagnosis of secondary ([[hypopituitarism]])
| |
| |-
| |
| | '''2'''|| Only if CRH production in the hypothalamus is intact
| |
| |-
| |
| | '''3'''|| Value doubles or more in stimulation
| |
| |-
| |
| | '''4'''|| Value less than doubles in stimulation
| |
| |- | |
| | '''5'''|| Most common, does not include all possible causes
| |
| |-
| |
| | '''6'''|| Usually because of very large tumor ([[macroadenoma]])
| |
| |- | |
| | '''7'''|| Includes [[Addison's disease]]
| |
| |}
| |
| | |
| ====Routine Investigations====
| |
| * [[Complete blood count]] and differential count - [[Eosinophilia]] and [[lymphocytosis]] (increased number of [[eosinophil]]s or [[lymphocyte]]s, two types of [[white blood cell]]s). [[Normocytic anemia]] may be present.
| |
| * Serum [[ACTH]] levels - elevated in primary adrenal insufficiency and decreased in secondary form.
| |
| * [[Hypoglycemia]] - low blood sugar (worse in children)
| |
| * [[Serum electrolytes]]:
| |
| ** [[Hyponatraemia]] - (low blood sodium levels)
| |
| ** [[Hyperkalemia]] - (raised blood [[potassium]] levels), due to loss of production of the hormone [[aldosterone]]
| |
| ** Mild [[hypercalcemia]] - in 20% patients
| |
| ** Mild non–anion-gap [[metabolic acidosis]]
| |
| * Serum [[cortisol]] - decreased (<25mcg/dL)
| |
| * Urine and sweat [[sodium]] - elevated
| |
| * Elevated [[BUN]] and [[creatinine]] - when [[hypovolemia]] is the cause.
| |
| * [[Prolactin]] - mild elevation may be present.
| |
| | |
| ===Imaging===
| |
| ====X-ray====
| |
| * Chest X-ray may show the following findings:
| |
| :* Size of the heart appears to be decreased.
| |
| :* [[Infection]]s either earlier or current ([[TB]], fungal) can be diagnosed using chest x-ray when they are the cause of Addison's disease.
| |
| * X-ray exams of the abdomen may be taken to see if the adrenals have any signs of calcium deposits. Calcium deposits may indicate [[tuberculosis]] ([[TB]])
| |
| | |
| ====CT Scan====
| |
| * [[CT]] scan findings in '''primary adrenal insufficiency''' include:
| |
| :* Small adrenal remnants bilaterally
| |
| :* Dense calcification in one or both adrenal beds without evidence of normal glandular remnants - in [[TB]]<ref name="pmid7119194">{{cite journal |author=Doppman JL, Gill JR, Nienhuis AW, Earll JM, Long JA |title=CT findings in Addison's disease |journal=J Comput Assist Tomogr |volume=6 |issue=4 |pages=757–61 |year=1982 |month=August |pmid=7119194 |doi= |url=}}</ref>
| |
| :* Enlarged nonhomogeneous glands of normal contour - in [[Histoplasmosis]]
| |
| :* Atrophic adrenal glands - in [[idiopathic]] [[autoimmune]] [[Addison's disease]].
| |
| * In '''secondary and tertiary adrenal insufficiency''' the following findings may be seen on CT head:
| |
| :* Calcified [[pituitary]] and/or [[hypothalamus]].
| |
| :* [[Pituitary adenomas]] - micro / macro
| |
| :* Absent pituitary and/or hypothalamus - surgical removal
| |
| | |
| ====MRI Scan====
| |
| * [[MRI]] findings in '''primary adrenal insufficiency''' include:
| |
| :* [[Adrenal hemorrhages]]
| |
| :* Adrenal masses:
| |
| :** [[Granulomatous disease]]
| |
| :** Adrenal [[lymphoma]]
| |
| :** Adrenal [[metastases]]
| |
| * [[MRI]] findings in '''secondary adrenal insufficiency''' include:
| |
| :* Pituitary adenomas
| |
|
| |
|
| ==Treatment== | | ==Treatment== |
| *;Adrenal crisis
| | [[Adrenal insufficiency medical therapy|Medical Therapy]] | [[Adrenal insufficiency surgery|Surgery]] | [[Adrenal insufficiency primary prevention|Primary Prevention]] | [[Adrenal insufficiency secondary prevention|Secondary Prevention]] | [[Adrenal insufficiency cost-effectiveness of therapy|Cost-Effectiveness of Therapy]] | [[Adrenal insufficiency future or investigational therapies|Future or Investigational Therapies]] |
| ** [[Intravenous fluids]]
| |
| ** Intravenous steroid ([[Solu-Cortef]]/injectable hydrocortisone) later hydrocortisone, prednisone or methylpredisolone tablets
| |
| ** Rest
| |
| | |
| *;Cortisol deficiency (primary and secondary)
| |
| ** [[Hydrocortisone]] (Cortef)
| |
| ** [[Prednisone]] (Deltasone)
| |
| ** [[Prednisolone]] (Delta-Cortef)
| |
| ** [[Methylprednisolone]] (Medrol)
| |
| ** [[Dexamethasone]] (Decadron)
| |
| | |
| *;Mineralocorticoid deficiency ([[low aldosterone]])
| |
| ** [[Fludrocortisone]] acetate
| |
| (To balance [[sodium]], [[potassium]] and increase water retention)
| |
| | |
| ==Prevention==
| |
| Acute adrenal insufficiency is fatal. When patients with adrenal insufficiency experience the following stress, they must be very careful.
| |
|
| |
| * Surgery: People who are not currently taking glucocorticoids but who have taken long-term glucocorticoids in the past year, and people with chronic adrenal insufficiency should tell their doctor before surgery. These patients must be treated with intravenous glucocorticoids and saline before surgery and continues until the patient is fully awake after surgery and able to take medication by mouth.
| |
| * Illness: Patients with adrenal insufficiency should know the essentiality of increasing medication during such periods of stress. During illness, oral dosing of glucocorticoid needs to be adjusted to mimic the normal response of the adrenal glands on the body. When significant [[fever]] or [[injury]] happen, the patients may require triple oral dosing. Once recovery from the stress event, doses can be returned to maintenance levels. Be careful, when the conditions of severe [[infection]]s, [[vomiting]], or [[diarrhea]] occur, these signs suggest the possibility of [[addisonian crisis]].
| |
| * Pregnancy: If [[nausea]] and [[vomiting]] in early pregnant woman with adrenal insufficiency interfere with taking medication by mouth, injections of the hormone may be necessary. During delivery, treatment is similar to that of people needing surgery.
| |
|
| |
|
| ==See also== | | ==See also== |
| Line 415: |
Line 48: |
| * [[Insulin tolerance test]], another test used to identify sub-types of [[adrenal insufficiency]]. | | * [[Insulin tolerance test]], another test used to identify sub-types of [[adrenal insufficiency]]. |
| * [[Adrenal fatigue]] (hypoadrenia), a term used in [[alternative medicine]] to describe a believed exhaustion of the [[adrenal glands]]. | | * [[Adrenal fatigue]] (hypoadrenia), a term used in [[alternative medicine]] to describe a believed exhaustion of the [[adrenal glands]]. |
|
| |
| ==References==
| |
| {{Reflist|2}}
| |
|
| |
|
| {{Endocrine pathology}} | | {{Endocrine pathology}} |