Sarcoidosis differential diagnosis: Difference between revisions
Ahmed Younes (talk | contribs) No edit summary |
No edit summary |
||
| (17 intermediate revisions by 3 users not shown) | |||
| Line 1: | Line 1: | ||
__NOTOC__ | __NOTOC__ | ||
{{Sarcoidosis}} | {{Sarcoidosis}} | ||
{{CMG}} {{AE}} | {{CMG}} {{AE}}{{HK}}Roshan Dinparasti Saleh M.D. | ||
==Overview== | ==Overview== | ||
[[Sarcoidosis]] has many differentials, which can be classified depending on the organ involved, pathologic findings and laboratory findings. | |||
==Differential Diagnosis== | ==Differential Diagnosis== | ||
Sarcoidosis has | [[Sarcoidosis]] has been defined as a multisystem granulomatous disorder of unknown cause<ref name="wasog">Statement on sarcoidosis: Joint Statement of the American Thoracic Society (ATS), the European Respiratory Society (ERS) and the World Association of Sarcoidosis and Other Granulomatous Disorders (WASOG) adopted by the ATS Board of Directors and by the ERS Executive Committee, February 1999. Am J Respir Crit Care Med 160:736–755, 1999.</ref>, but [[granulomatous inflammation]] alone is not sufficient for the diagnosis of [[sarcoidosis]] because alternative etiologies of [[granulomatous inflammation]] need to be excluded. | ||
===Causes of [[granulomatous reaction]] beside [[sarcoidosis]]=== | |||
* [[Mycobacterium tuberculosis]] | |||
* [[Mycoplasma]] | |||
* [[Pneumocystis jiroveci]] | |||
* [[Brucellosis]] | |||
* [[Cat-scratch fever]] | |||
* [[Atypical mycobacteria]] | |||
* [[Toxoplasmosis]] | |||
* [[Berylliosis]] | |||
* [[Hard metal]] | |||
* [[Zirconium]] | |||
* [[Tattoo]] | |||
* [[Hypersensitivity pneumonitis]] | |||
* Medications (e.g., [[methotrexate]]) | |||
* [[ANCA-associated vasculitis]] | |||
* [[Necrotizing sarcoid granuloma]] | |||
* [[Lymphoma]] | |||
* [[Cancer]] | |||
* Granulomatous lesions of unknown significance | |||
* [[Crohn’s disease]] | |||
* [[Lymphocytic interstitial pneumonia]] | |||
* [[Behçet’s disease]] | |||
* [[Rheumatoid nodules]]<ref name="wasog">Statement on sarcoidosis: Joint Statement of the American Thoracic Society (ATS), the European Respiratory Society (ERS) and the World Association of Sarcoidosis and Other Granulomatous Disorders (WASOG) adopted by the ATS Board of Directors and by the ERS Executive Committee, February 1999. Am J Respir Crit Care Med 160:736–755, 1999.</ref> | |||
''' | ===Data supporting the likelihood of [[sarcoidosis]]=== | ||
# '''Demographics''' | |||
## U.S. [[African American]] | |||
## [[Northern European]] | |||
# '''Medical history''' | |||
## [[Non-smoker]] | |||
## No symptoms (in patient with [[bilateral hilar adenopathy]] on [[CXR]]) | |||
## Family history of [[sarcoidosis]] | |||
## Symptoms involving more than two organs commonly involved by [[sarcoidosis]] | |||
# '''Laboratory data''' | |||
## Elevated [[ACE]] level (especially if > 2× ULN) | |||
## Elevated [[calcium]] level | |||
## Elevated [[alkaline phosphatase]] level | |||
## Elevated [[soluble IL-2 receptor]] | |||
## [[Leukopenia]] | |||
# '''Radiographic findings''' | |||
## [[CXR]]: | |||
###[[bilateral hilar adenopathy]] especially if '''without''' symptoms | |||
### Upper lobe disease | |||
## [[HRCT]]: | |||
### Disease along bronchovascular bundle | |||
### Subpleural reticulonodular infiltrates | |||
### [[Mediastinal adenopathy]] | |||
### [[Peribronchial thickening]] | |||
### [[Traction bronchiectasis]] of upper lobe | |||
# '''Skin lesions''' | |||
## [[Lupus pernio]] | |||
## [[Erythema nodosum]] | |||
## Maculopapular lesions | |||
# '''Ocular disease''' | |||
## [[Uveitis]] | |||
## [[Optic neuritis]] | |||
# '''Neurological disease''' | |||
## [[Seventh cranial nerve palsy]] | |||
# '''Renal disease''' | |||
## [[Nephrocalcinosis]] | |||
## [[Interstitial nephritis]]<ref name="judson">Judson MA: The diagnosis of sarcoidosis. Clin Chest Med 29(3):415–427, 2008.</ref> | |||
''' | ===Data weakening the likelihood of [[sarcoidosis]]=== | ||
# '''Demographics''' | |||
## Age< 18 years | |||
# '''Medical history''' | |||
## Exposure to [[tuberculosis]] | |||
## Exposure to [[organic bioaerosol]] | |||
## Exposure to [[beryllium]] | |||
## [[Intravenous drug abuse]] | |||
''' | # '''Laboratory data''' | ||
## Positive [[anti-neutrophil cytoplasm antibody]] ([[ANCA]]) | |||
# '''Radiographic findings''' | |||
## [[CXR]]: | |||
### [[Pleural effusion]] | |||
## [[HRCT]]: | |||
### Subpleural [[honeycombing]] | |||
''' | # '''Ocular disease''' | ||
## [[Episcleritis]] | |||
# '''Renal disease''' | |||
## [[Glomerulonephritis]] <ref name="judson">Judson MA: The diagnosis of sarcoidosis. Clin Chest Med 29(3):415–427, 2008.</ref> | |||
{{familytree/start}} | |||
{{familytree | | | | | | | | | | | | | | A01 | | | | | | | | | |A01=Spirometry}} | |||
{{familytree | | | | | | | | | | | | | | |!| | | | | | | | | | | }} | |||
{{familytree | | | | | | |,|-|-|-|-|-|-|-|^|-|-|-|-|-|-|-|.| | | |}} | |||
{{familytree | | | | | | B01 | | | | | | | | | | | | | | B02 | | | |B01=Low FEV1/FVC ratio|B02=Normal to high FEV1/FVC ratio|}} | |||
{{familytree | | | | | | |!| | | | | | | | | | | | | | | |!| | | | | }} | |||
{{familytree | | | | | | C01 | | | | | | | | | | | | | | C02 | | | |C01=Obstructive Lung Disease|C02=Restrictive Lung Disease|}} | |||
{{familytree | | | | | | |!| | | | | | | | | | | | | | | |!| | | | | }} | |||
{{familytree | | | | | | D01 | | | | | | | | | | | | | | D02 | | | | |D01=Bronchodilator therapy|D02=DLCO}} | |||
{{familytree | | | | | | |!| | | | | | | | | | | | | | | |!| | | | | }} | |||
{{familytree | |,|-|-|-|-|^|-|-|-|-|.| | | | | |,|-|-|-|-|^|-|-|-|-|.| }} | |||
{{familytree | E01 | | | | | | | | E02 | | | | E03 | | | | | | | | E04 | | |E01=Increased FEV1|E02=No change in FEV1|E03=Normal DLCO|E04=Decreased DLCO|}} | |||
{{familytree | |!| | | | | | | | | |!| | | | | |!| | | | | | | | | |!| | | }} | |||
{{familytree | F01 | | | | | | | | F02 | | | | F03 | | | | | | | | F04 | | |F01=Asthma|F02=COPD|F03=Chest wall disorders|F04=Interstitial Lung Disease|}} | |||
{{familytree/end}} | |||
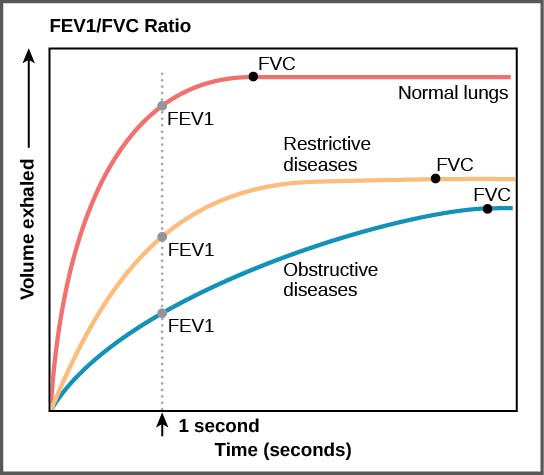
==Differential diagnosis== | ====Spirometry Findings in Various Lung Conditions==== | ||
[[image:Figure 39 03 05f.jpg|thumb|center|Spirometry showing Obstructive and Restrictive Lung Disease ([Source:By CNX OpenStax [CC BY 4.0 (http://creativecommons.org/licenses/by/4.0)], via Wikimedia Commons])]] | |||
{| | |||
|- style="background: #4479BA; color: #FFFFFF; text-align: center;" | |||
! colspan="2" rowspan="3" |Disease | |||
! colspan="11" |Clinical manifestations | |||
! colspan="5" |Diagnosis | |||
|- style="background: #4479BA; color: #FFFFFF; text-align: center;" | |||
! colspan="4" |Symptoms | |||
! colspan="7" |Physical exam | |||
! rowspan="2" |Lab findings | |||
! colspan="3" |Imaging | |||
!Gold standard | |||
|- style="background: #4479BA; color: #FFFFFF; text-align: center;" | |||
!Cough | |||
!Dyspnea | |||
!Hemoptysis | |||
!Fever | |||
!History/Exposure | |||
!Cyanosis | |||
!Clubbing | |||
!JVD | |||
!Peripheral edema | |||
!Auscultation | |||
!Other prominent findings | |||
!CXR | |||
!CT | |||
!DLCco | |||
! | |||
|- style="background: #DCDCDC; padding: 5px; text-align: center;" | | |||
| colspan="2" |Hypersensitivity Pneumonitis | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" |<nowiki>+</nowiki> | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" |<nowiki>+</nowiki> | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" |<nowiki>-</nowiki> | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" |<nowiki>+</nowiki> | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="left" | | |||
* History of [[allergen]] exposure | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" |<nowiki>-</nowiki> | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" |<nowiki>+</nowiki> | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" |<nowiki>-</nowiki> | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" |<nowiki>-</nowiki> | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="left" | | |||
* Diffuse fine bibasilar [[crackles]] | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="left" | | |||
* Constitutional symptoms | |||
** [[Weight loss]] | |||
** Anorexia | |||
** Muscle weakness | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="left" | | |||
* Neutrophilia | |||
* Elevated [[ESR]] | |||
* Elevated [[CRP]] | |||
* Elevated [[immunoglobulin]] | |||
* No peripheral blood [[eosinophilia]] | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="left" | | |||
* Poorly defined micronodular or diffuse interstitial pattern | |||
* In chronic form | |||
** Fibrosis | |||
** Loss of lung volume | |||
** Coarse linear opacities | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="left" | | |||
* Ground-glass opacities '''or''' | |||
* Diffusely increased radiodensities | |||
* Diffuse micronodules | |||
* Focal air trapping | |||
* Mosaic perfusion | |||
* Occasionaly thin-walled cysts | |||
* Mild fibrotic changes | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" |''↓'' | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" | | |||
*Clinical diagnosis | |||
|- style="background: #DCDCDC; padding: 5px; text-align: center;" | | |||
| colspan="2" |[[Acute respiratory distress syndrome|Acute Respiratory Distress Syndrome]] ([[Acute respiratory distress syndrome|ARDS]]) | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" | - | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" | + | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" | - | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" | - | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="left" | | |||
* [[Trauma]] | |||
* [[Sepsis]] | |||
* [[Drug overdose]] | |||
* [[Blood transfusion|Massive transfusion]] | |||
* [[Acute pancreatitis]] [[Aspiration]] | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" | + | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" | - | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" | - | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" | - | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="left" | | |||
* Coarse [[breath sounds]] | |||
* Rhonchi [[crackles]] | |||
* Decreased [[breath sounds]] | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="left" | | |||
* Initially [[respiratory alkalosis]] transforming to respiratory acidosis | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="left" | | |||
* [[BNP]] level of less than 100 pg/mL | |||
* PaO<sub>2</sub> '''/''' FiO<sub>2</sub> <300 | |||
* [[Leukopenia]] | |||
* [[Leukocytosis]] | |||
* [[Thrombocytopenia]] | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="left" | | |||
* Bilateral pulmonary infiltrates | |||
** Initially patchy peripheral | |||
** Later diffuse bilateral | |||
* Ground glass | |||
* Frank alveolar infiltrate | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="left" | | |||
* Bronchial dilatation within areas of ground-glass opacification | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" |''↓'' | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="left" | | |||
* PaO<sub>2</sub> '''/''' FiO<sub>2</sub> <300 | |||
|- style="background: #DCDCDC; padding: 5px; text-align: center;" | | |||
| rowspan="2" |[[Bronchitis]] | |||
|Acute | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" |<nowiki>+</nowiki> | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" |<nowiki>-</nowiki> | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" |<nowiki>+/-</nowiki> | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" |<nowiki>+</nowiki> | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" |<nowiki>-</nowiki> | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" |<nowiki>-</nowiki> | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" |<nowiki>-</nowiki> | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" |<nowiki>-</nowiki> | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" |<nowiki>-</nowiki> | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="left" | | |||
* Diffuse [[Wheeze|wheezes]] | |||
* High-pitched continuous sounds | |||
* The use of accessory muscles | |||
* Prolonged expiration | |||
* [[Rhonchi]] | |||
* [[Rales]] | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="left" | | |||
* [[Hoarseness]] | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="left" | | |||
* N/A | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="left" | | |||
* Normal | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="left" | | |||
* N/A | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" | - | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="left" | | |||
* Clinical diagnosis | |||
|- style="background: #DCDCDC; padding: 5px; text-align: center;" | | |||
|Chronic | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" | + | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" | + | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" | - | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" | - | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="left" | | |||
* A positive history of chronic productive [[cough]] | |||
* Shortness of breath | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" | + | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" | - | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" | + | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" | + | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="left" | | |||
* Prolonged expiration; [[wheezing]] | |||
* Diffusely decreased breath sound | |||
* Coarse [[crackles]] with inspiration | |||
* Coarse [[rhonchi]] | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="left" | | |||
* N/A | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="left" | | |||
* Chronic [[hypoxemia]] may lead to [[polycythemia]] | |||
* Increase in [[Neutrophil|Neutrophils]] count | |||
* Chronic [[respiratory acidosis]]. | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="left" | | |||
* Radiolucency | |||
* Diaphragmatic flattening due to hyperinflation | |||
* Increased retrosternal airspace on the lateral radiograph | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="left" | | |||
* N/A | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" |''↓'' | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="left" | | |||
*N/A | |||
|- style="background: #DCDCDC; padding: 5px; text-align: center;" | | |||
| rowspan="4" |[[Occupational lung disease|Pneumoconiosis]]<ref name="pmid9563720">{{cite journal |vauthors=Gay SE, Kazerooni EA, Toews GB, Lynch JP, Gross BH, Cascade PN, Spizarny DL, Flint A, Schork MA, Whyte RI, Popovich J, Hyzy R, Martinez FJ |title=Idiopathic pulmonary fibrosis: predicting response to therapy and survival |journal=Am. J. Respir. Crit. Care Med. |volume=157 |issue=4 Pt 1 |pages=1063–72 |year=1998 |pmid=9563720 |doi=10.1164/ajrccm.157.4.9703022 |url=}}</ref> | |||
|[[Occupational lung disease|SIlicosis]]<ref name="pmid16545629">{{cite journal |vauthors=du Bois RM |title=Evolving concepts in the early and accurate diagnosis of idiopathic pulmonary fibrosis |journal=Clin. Chest Med. |volume=27 |issue=1 Suppl 1 |pages=S17–25, v–vi |year=2006 |pmid=16545629 |doi=10.1016/j.ccm.2005.08.001 |url=}}</ref><ref name="pmid21996929">{{cite journal |vauthors=Neghab M, Mohraz MH, Hassanzadeh J |title=Symptoms of respiratory disease and lung functional impairment associated with occupational inhalation exposure to carbon black dust |journal=J Occup Health |volume=53 |issue=6 |pages=432–8 |year=2011 |pmid=21996929 |doi= |url=}}</ref> | |||
| rowspan="4" style="padding: 5px 5px; background: #F5F5F5;" align="center" | + | |||
| rowspan="4" style="padding: 5px 5px; background: #F5F5F5;" align="center" | + | |||
| rowspan="4" style="padding: 5px 5px; background: #F5F5F5;" align="center" | +/- | |||
| rowspan="4" style="padding: 5px 5px; background: #F5F5F5;" align="center" | - | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="left" | | |||
* Occupational history | |||
** Sandblasting | |||
** Bystanders | |||
** Quartzite miller | |||
** Tunnel workers | |||
** Silica flour workers | |||
** Workers in the scouring powder industry | |||
| rowspan="4" style="padding: 5px 5px; background: #F5F5F5;" align="center" | + | |||
| rowspan="4" style="padding: 5px 5px; background: #F5F5F5;" align="center" | + | |||
| rowspan="4" style="padding: 5px 5px; background: #F5F5F5;" align="center" | + | |||
| rowspan="4" style="padding: 5px 5px; background: #F5F5F5;" align="center" | - | |||
| rowspan="4" style="padding: 5px 5px; background: #F5F5F5;" align="left" | | |||
**Hyperresonant | |||
**Fine [[crackles]] | |||
**Rhonchi | |||
**Bronchial breath sounds | |||
**Expiratory wheezing | |||
**Increased [[tactile fremitus]]. | |||
**Loud P2 | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="left" | | |||
*Increased susceptiblity to [[tuberculosis]]. | |||
| rowspan="4" style="padding: 5px 5px; background: #F5F5F5;" align="left" | | |||
*[[Respiratory acidosis]] | |||
*[[Abnormal sputum]] | |||
*[[Anemia]] | |||
*[[Neutrophilia]] | |||
*Elevated [[ESR]] | |||
*Elevated [[CRP]] | |||
*Elevated [[immunoglobulin]] | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="left" | | |||
* Small round opacities | |||
** Symmetrically distributed | |||
** Upper-zone predominance | |||
* Diffuse interstitial pattern of fibrosis without the typical nodular opacities in chronic case | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="left" | | |||
* Nodular changes in lung parenchyma | |||
* Progressive massive fibrosis | |||
* Bullae, emphysema | |||
* Pleural, mediastinal, and hilar changes | |||
| rowspan="4" style="padding: 5px 5px; background: #F5F5F5;" align="center" |''↓'' | |||
| rowspan="4" style="padding: 5px 5px; background: #F5F5F5;" align="left" | | |||
* [[Biopsy|Lung biopsy]] | |||
|- style="background: #DCDCDC; padding: 5px; text-align: center;" | | |||
|[[Asbestosis]] | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="left" | | |||
* Shipyard workers | |||
* Pipe fitting | |||
* Insulators | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="left" | | |||
* [[Lung cancer]] | |||
* [[Mesothelioma]] | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="left" | | |||
* Predilection to lower lobes | |||
* Fine and coarse linear, peripheral, reticular opacities | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="left" | | |||
* Subpleural linear opacities seen parallel to the pleura | |||
* Basilar lung fibrosis | |||
* Peribronchiolar, intralobular, and interlobular septal fibrosis; | |||
* Honeycombing | |||
* Pleural plaques. | |||
|- style="background: #DCDCDC; padding: 5px; text-align: center;" | | |||
|[[Berylliosis]] | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="left" | | |||
* Electronic manufactures | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" | - | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="left" | | |||
* Hilar adenopathy | |||
* Increased interstitial markings. | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="left" | | |||
* Ground glass opacification | |||
* Parenchymal nodules | |||
* Septal lines | |||
|- style="background: #DCDCDC; padding: 5px; text-align: center;" | | |||
|[[Byssinosis]] | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="left" | | |||
* Cotton wool workers | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="left" | | |||
* Increased susceptibility to ''[[Actinomyces]]'' and ''[[Aspergillus]]'' infection. | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="left" | | |||
* Diffuse air-space consolidation | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="left" | | |||
* Pulmonary fibrosis with honeycombing | |||
* Peri bronchovascular distribution of nodules | |||
* Ground-glass attenuations | |||
|- style="background: #DCDCDC; padding: 5px; text-align: center;" | | |||
| colspan="2" |[[Sarcoidosis]] | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" |<nowiki>+</nowiki> | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" |<nowiki>+</nowiki> | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" |<nowiki>+</nowiki> | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" |<nowiki>+</nowiki> | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="left" | | |||
* African Americans | |||
* [[Autoimmune]] | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" |<nowiki>-</nowiki> | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" |<nowiki>-</nowiki> | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" |<nowiki>-</nowiki> | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" |<nowiki>-</nowiki> | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="left" | | |||
* Usually normal | |||
* Occasional crackles | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="left" | | |||
* [[Dermatological lesions|Dermatologic manifestations]] | |||
* Ocular involvement | |||
* Osseous involvement | |||
* Heart failure from [[cardiomyopathy]] | |||
* Lymphocytic [[meningitis]] | |||
* [[Cranial nerve palsies]] | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="left" | | |||
* [[Hypercalcemia]] or [[hypercalciuria]] | |||
* Elevated [[Vitamin D|1, 25-dihydroxyvitamin D levels]] | |||
* Elevated [[angiotensin-converting enzyme]] (ACE) | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="left" | | |||
* Bilateral hilar lymphadenopathy | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="left" | | |||
* High-resolution CT (HRCT) scanning of the chest may identify | |||
** Active alveolitis | |||
** Fibrosis | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" |''↓'' | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="left" | | |||
* [[Biopsy]] | |||
|- style="background: #DCDCDC; padding: 5px; text-align: center;" | | |||
| colspan="2" |[[Pleural effusion|Pleural Effusion]] | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" |<nowiki>+</nowiki> | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" |<nowiki>+</nowiki> | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" |<nowiki>+/-</nowiki> | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" |<nowiki>+/-</nowiki> | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="left" |'''Transudate''' | |||
* [[Congestive heart failure|CHF]] | |||
* [[Cirrhosis]] | |||
'''Exudate''' | |||
* [[Parapneumonic effusion|Parapneumonic causes]] | |||
* [[Malignancy]] | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" |<nowiki>+/-</nowiki> | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" |<nowiki>+/-</nowiki> | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" |<nowiki>+/-</nowiki> | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" |<nowiki>+/-</nowiki> | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="left" | | |||
* Decreased [[tactile fremitus]] | |||
* Diminished or inaudible [[breath sounds]] | |||
* Pleural [[friction rub]] | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="left" | | |||
* Peripheral edema, distended neck veins, and S<sub>3</sub> gallop suggest [[congestive heart failure]]. | |||
* Edema may also be a manifestation of nephrotic syndrome, pericardial disease, or, when combined with yellow nailbeds, the yellow nail syndrome. | |||
* Cutaneous changes and ascites suggest liver disease. | |||
* Lymphadenopathy or a palpable mass suggests malignancy. | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="left" | | |||
* Thoracentesis | |||
** [[Exudate]] | |||
** [[Transudate]] | |||
** [[LDH]], [[glucose]], [[cytology]] | |||
* Other specific labs of underlying etiology | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="left" |Supine | |||
* Blunting of the costophrenic angle | |||
* Homogenous increase in density spread over the lower lung fields | |||
Lateral decubitus | |||
* Free flowing effusion as layers | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="left" | | |||
* Thickened pleura | |||
* Mild effusions can aslo be detected | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" |''↓'' | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="left" | | |||
* [[Thoracocentesis]] | |||
|- style="background: #DCDCDC; padding: 5px; text-align: center;" | | |||
| colspan="2" |Interstitial (Nonidiopathic) [[Idiopathic pulmonary fibrosis|Pulmonary Fibrosis]] | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" | + | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" | ++ | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" | + | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" | - | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="left" | | |||
* [[Connective tissue disorder|Connective-tissue disorder]] | |||
* [[Pneumoconiosis]] | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" | + | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" | + | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" | + | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" | + | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="left" | | |||
* [[Wheezing]] | |||
* [[S3]] | |||
* [[P2]] | |||
* End-inspiratory rales | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="left" | | |||
* Increased A-a gradient | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="left" | | |||
* Elevated [[ESR]] | |||
* Serologic testing for [[ANA]], [[RF]], [[Anti-neutrophil cytoplasmic antibody|ANCA]] & ASCA may be positive | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="left" | | |||
* Reticular and/or nodular opacities | |||
* Honeycomb appearance (late finding) | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="left" | | |||
* Bilateral reticular and nodular interstitial infiltrates | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" |''↓'' | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" |Video-assisted thoracoscopic lung biopsy | |||
|- style="background: #DCDCDC; padding: 5px; text-align: center;" | | |||
| colspan="2" |[[Interstitial Pneumonia|Lymphocytic Interstitial Pneumonia]]<ref name="pmid10397102">{{cite journal |vauthors=Honda O, Johkoh T, Ichikado K, Tomiyama N, Maeda M, Mihara N, Higashi M, Hamada S, Naito H, Yamamoto S, Nakamura H |title=Differential diagnosis of lymphocytic interstitial pneumonia and malignant lymphoma on high-resolution CT |journal=AJR Am J Roentgenol |volume=173 |issue=1 |pages=71–4 |year=1999 |pmid=10397102 |doi=10.2214/ajr.173.1.10397102 |url=}}</ref> | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" | + | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" | + | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" | + | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" | + | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="left" | | |||
* [[Autoimmune]] | |||
* [[Lymphoproliferative disorders]] | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" | - | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" | + | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" | - | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" | - | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="left" | | |||
* [[Wheezing]] | |||
* [[Rales]] | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="left" | | |||
* Increased A-a gradient | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="left" | | |||
* Polyclonal hypergammaglobulinemia | |||
* Increased [[LDH]] | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="left" | | |||
* Bibasilar interstitial or micronodular infiltrates | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="left" | | |||
* Determines the degree of fibrosis | |||
* Cysts (characterstic) | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" |N | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" |Open lung biopsy | |||
|- style="background: #DCDCDC; padding: 5px; text-align: center;" | | |||
| colspan="2" |[[Obesity]]<ref name="pmid21116339">{{cite journal |vauthors=Zammit C, Liddicoat H, Moonsie I, Makker H |title=Obesity and respiratory diseases |journal=Int J Gen Med |volume=3 |issue= |pages=335–43 |year=2010 |pmid=21116339 |pmc=2990395 |doi=10.2147/IJGM.S11926 |url=}}</ref><ref name="O’Neill2015">{{cite journal|last1=O’Neill|first1=Donal|title=Measuring obesity in the absence of a gold standard|journal=Economics & Human Biology|volume=17|year=2015|pages=116–128|issn=1570677X|doi=10.1016/j.ehb.2015.02.002}}</ref> | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" | + | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" | + | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" | - | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" | - | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="left" | | |||
* Overweight | |||
* [[Diabetes mellitus]] | |||
* [[Asthma]] | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" | - | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" | - | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" | - | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" | + | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="left" | | |||
* [[Wheezing]] | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" | - | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="left" | | |||
* [[Polycythemia|Increased hematocrit]] | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="left" | | |||
* X ray findings are often limited due to body habitus | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="left" | | |||
* CT findings are variable and depends upon severity of obesity | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" |N | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" |Clinical | |||
|- style="background: #DCDCDC; padding: 5px; text-align: center;" | | |||
| colspan="2" |[[Eosinophilia|Pulmonary Eosinophilia]]<ref name="pmid19706907">{{cite journal |vauthors=de Górgolas M, Casado V, Renedo G, Alen JF, Fernández Guerrero ML |title=Nodular lung schistosomiais lesions after chemotherapy for dysgerminoma |journal=Am. J. Trop. Med. Hyg. |volume=81 |issue=3 |pages=424–7 |year=2009 |pmid=19706907 |doi= |url=}}</ref> | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" | + | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" | + | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" | + | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" | + | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="left" |Infections | |||
* [[Parasitic]] | |||
* [[Fungal]] | |||
* [[Mycobacterial]] | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" | + | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" | - | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" | + | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" | + | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="left" | | |||
* [[Wheezing]] | |||
* [[Rales]] | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="left" | | |||
* Increased A-a gradient | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="left" | | |||
* [[Leukocytosis]] with [[eosinophilia]] (> 250/µL) | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" | | |||
* Interstitial or diffuse nodular densities | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="left" | | |||
* Determines extent and distribution of the disease | |||
* Interstitial infiltrates | |||
* Cysts and nodules | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" |''↓'' | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" |Biopsy of lesion (skin or lung) | |||
|- style="background: #DCDCDC; padding: 5px; text-align: center;" | | |||
| rowspan="4" |Neuromuscular disease | |||
|Scoliosis | |||
|- | | style="padding: 5px 5px; background: #F5F5F5;" align="center" | - | ||
| | | style="padding: 5px 5px; background: #F5F5F5;" align="center" | + | ||
*[[ | | style="padding: 5px 5px; background: #F5F5F5;" align="center" | - | ||
| | | style="padding: 5px 5px; background: #F5F5F5;" align="center" | - | ||
| style="padding: 5px 5px; background: #F5F5F5;" align="left" | | |||
* Postural abnormality | |||
* | | style="padding: 5px 5px; background: #F5F5F5;" align="center" | - | ||
* | | style="padding: 5px 5px; background: #F5F5F5;" align="center" | - | ||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" | - | |||
| | | style="padding: 5px 5px; background: #F5F5F5;" align="center" | - | ||
*A | | style="padding: 5px 5px; background: #F5F5F5;" align="left" | | ||
*[[ | * Decreased [[breath sounds]] | ||
| | | style="padding: 5px 5px; background: #F5F5F5;" align="left" | | ||
* In severe scoliosis, the rib cage may press against the lungs making it more difficult to breathe. | |||
|- | | style="padding: 5px 5px; background: #F5F5F5;" align="left" | | ||
| | * R/0 genetic conditions | ||
** [[Marfan's syndrome]] | |||
| | ** [[Edwards syndrome|Edward's syndrome]] | ||
* | * Total [[Lymphocyte|lymphocyte count]] (should be >1500/μL) | ||
* | * Nutritional status must be assessed | ||
| | | style="padding: 5px 5px; background: #F5F5F5;" align="left" | | ||
* Accurate depiction of the true magnitude of the spinal deformity can be assessed by supine anteroposterior (AP) and lateral spinal radiographs | |||
| | | style="padding: 5px 5px; background: #F5F5F5;" align="left" | | ||
* N/A | |||
|- | | style="padding: 5px 5px; background: #F5F5F5;" align="center" |N | ||
| | | style="padding: 5px 5px; background: #F5F5F5;" align="left" | | ||
*[[ | * Clinical | ||
| | * Radiographs | ||
* | |- style="background: #DCDCDC; padding: 5px; text-align: center;" | | ||
* | |[[Muscular dystrophy]] | ||
* | | style="padding: 5px 5px; background: #F5F5F5;" align="center" |<nowiki>-</nowiki> | ||
* | | style="padding: 5px 5px; background: #F5F5F5;" align="center" |<nowiki>+</nowiki> | ||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" |<nowiki>-</nowiki> | |||
| | | style="padding: 5px 5px; background: #F5F5F5;" align="center" |<nowiki>-</nowiki> | ||
| style="padding: 5px 5px; background: #F5F5F5;" align="left" | | |||
*[[ | * Proximal muscle weakness | ||
| | | style="padding: 5px 5px; background: #F5F5F5;" align="center" |<nowiki>-</nowiki> | ||
*[[ | | style="padding: 5px 5px; background: #F5F5F5;" align="center" |<nowiki>-</nowiki> | ||
| | | style="padding: 5px 5px; background: #F5F5F5;" align="center" |<nowiki>-</nowiki> | ||
| | | style="padding: 5px 5px; background: #F5F5F5;" align="center" | - | ||
* | | style="padding: 5px 5px; background: #F5F5F5;" align="left" | | ||
| | * Decreased [[breath sounds]] | ||
| style="padding: 5px 5px; background: #F5F5F5;" align="left" | | |||
* [[Rash]] | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="left" | | |||
* Elevated [[CPK]] and [[aldolase]] | |||
* [[Antinuclear antibodies|+ANA]] | |||
* +Anti-Jo abs | |||
* Elevated [[ESR]], [[C-reactive protein|CRP]] and [[RF]] | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="left" | | |||
* N/A | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="left" | | |||
* N/A | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" |N | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="left" | | |||
* [[Muscle biopsy]] | |||
|- style="background: #DCDCDC; padding: 5px; text-align: center;" | | |||
|[[ALS]] | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" |<nowiki>-</nowiki> | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" |<nowiki>+</nowiki> | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" |<nowiki>-</nowiki> | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" |<nowiki>-</nowiki> | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="left" | | |||
* Muscle weakness | |||
* Neurological deficit | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" |<nowiki>-</nowiki> | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" |<nowiki>-</nowiki> | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" |<nowiki>-</nowiki> | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" |<nowiki>-</nowiki> | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="left" | | |||
* Decreased [[breath sounds]] | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="left" | | |||
* Symptoms begin with limb involvement diue to muscle weakness and atrophy. | |||
* Cognitive or behavioral dysfunction | |||
* Sensory nerves and the autonomic nervous system are generally unaffected | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" |N/A | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" |Not significant/diagnostic | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" |Not significant/diagnostic | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" |<nowiki>-</nowiki> | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="left" | | |||
* Clinical diagnosis | |||
* Nerve conduction studies and needle [[electromyography]] (EMG) | |||
|- style="background: #DCDCDC; padding: 5px; text-align: center;" | | |||
|[[Myasthenia gravis]] | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" | - | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" | + | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" | - | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" | + | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="left" |H/O of difficulty getting up from chair | |||
* Combing | |||
* [[Dysphagia|Difficulty in swallowing]] | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" | - | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" | - | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" | - | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" | - | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="left" | | |||
* Decreased [[breath sounds]] | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="left" | | |||
* Extraocular, bulbar, or proximal limb muscles. | |||
* Breathing as rapid and shallow | |||
* Respiratory muscle weakness can lead to acute respiratory failure may require immediate intubation. | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="left" | | |||
* Anti–acetylcholine receptor (AChR) antibody (Ab) test + | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="left" | | |||
* [[Thymoma]] as an anterior mediastinal mass. | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="left" | | |||
* [[Thymoma]] as an anterior mediastinal mass. | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="center" |N | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="left" | | |||
* [[Electromyography]] | |||
|} | |||
==References== | |||
Latest revision as of 21:58, 27 October 2019
|
Sarcoidosis Microchapters |
|
Diagnosis |
|---|
|
Treatment |
|
Case Studies |
|
Sarcoidosis differential diagnosis On the Web |
|
American Roentgen Ray Society Images of Sarcoidosis differential diagnosis |
|
Risk calculators and risk factors for Sarcoidosis differential diagnosis |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1] Associate Editor(s)-in-Chief: Syed Hassan A. Kazmi BSc, MD [2]Roshan Dinparasti Saleh M.D.
Overview
Sarcoidosis has many differentials, which can be classified depending on the organ involved, pathologic findings and laboratory findings.
Differential Diagnosis
Sarcoidosis has been defined as a multisystem granulomatous disorder of unknown cause[1], but granulomatous inflammation alone is not sufficient for the diagnosis of sarcoidosis because alternative etiologies of granulomatous inflammation need to be excluded.
Causes of granulomatous reaction beside sarcoidosis
- Mycobacterium tuberculosis
- Mycoplasma
- Pneumocystis jiroveci
- Brucellosis
- Cat-scratch fever
- Atypical mycobacteria
- Toxoplasmosis
- Berylliosis
- Hard metal
- Zirconium
- Tattoo
- Hypersensitivity pneumonitis
- Medications (e.g., methotrexate)
- ANCA-associated vasculitis
- Necrotizing sarcoid granuloma
- Lymphoma
- Cancer
- Granulomatous lesions of unknown significance
- Crohn’s disease
- Lymphocytic interstitial pneumonia
- Behçet’s disease
- Rheumatoid nodules[1]
Data supporting the likelihood of sarcoidosis
- Demographics
- Medical history
- Non-smoker
- No symptoms (in patient with bilateral hilar adenopathy on CXR)
- Family history of sarcoidosis
- Symptoms involving more than two organs commonly involved by sarcoidosis
- Laboratory data
- Elevated ACE level (especially if > 2× ULN)
- Elevated calcium level
- Elevated alkaline phosphatase level
- Elevated soluble IL-2 receptor
- Leukopenia
- Radiographic findings
- CXR:
- bilateral hilar adenopathy especially if without symptoms
- Upper lobe disease
- HRCT:
- Disease along bronchovascular bundle
- Subpleural reticulonodular infiltrates
- Mediastinal adenopathy
- Peribronchial thickening
- Traction bronchiectasis of upper lobe
- CXR:
- Skin lesions
- Lupus pernio
- Erythema nodosum
- Maculopapular lesions
- Ocular disease
- Neurological disease
- Renal disease
Data weakening the likelihood of sarcoidosis
- Demographics
- Age< 18 years
- Medical history
- Exposure to tuberculosis
- Exposure to organic bioaerosol
- Exposure to beryllium
- Intravenous drug abuse
- Laboratory data
- Positive anti-neutrophil cytoplasm antibody (ANCA)
- Radiographic findings
- CXR:
- HRCT:
- Subpleural honeycombing
- Ocular disease
- Renal disease
| Spirometry | |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| Low FEV1/FVC ratio | Normal to high FEV1/FVC ratio | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| Obstructive Lung Disease | Restrictive Lung Disease | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| Bronchodilator therapy | DLCO | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| Increased FEV1 | No change in FEV1 | Normal DLCO | Decreased DLCO | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| Asthma | COPD | Chest wall disorders | Interstitial Lung Disease | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
Spirometry Findings in Various Lung Conditions
| Disease | Clinical manifestations | Diagnosis | |||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Symptoms | Physical exam | Lab findings | Imaging | Gold standard | |||||||||||||
| Cough | Dyspnea | Hemoptysis | Fever | History/Exposure | Cyanosis | Clubbing | JVD | Peripheral edema | Auscultation | Other prominent findings | CXR | CT | DLCco | ||||
| Hypersensitivity Pneumonitis | + | + | - | + |
|
- | + | - | - |
|
|
|
|
|
↓ |
| |
| Acute Respiratory Distress Syndrome (ARDS) | - | + | - | - | + | - | - | - |
|
|
|
|
|
↓ |
| ||
| Bronchitis | Acute | + | - | +/- | + | - | - | - | - | - |
|
|
|
- |
| ||
| Chronic | + | + | - | - |
|
+ | - | + | + |
|
|
|
|
↓ |
| ||
| Pneumoconiosis[3] | SIlicosis[4][5] | + | + | +/- | - |
|
+ | + | + | - |
|
|
|
|
|
↓ | |
| Asbestosis |
|
|
| ||||||||||||||
| Berylliosis |
|
- |
|
| |||||||||||||
| Byssinosis |
|
|
|
| |||||||||||||
| Sarcoidosis | + | + | + | + |
|
- | - | - | - |
|
|
|
|
|
↓ | ||
| Pleural Effusion | + | + | +/- | +/- | Transudate
Exudate |
+/- | +/- | +/- | +/- |
|
|
|
Supine
Lateral decubitus
|
|
↓ | ||
| Interstitial (Nonidiopathic) Pulmonary Fibrosis | + | ++ | + | - | + | + | + | + |
|
|
|
↓ | Video-assisted thoracoscopic lung biopsy | ||||
| Lymphocytic Interstitial Pneumonia[6] | + | + | + | + | - | + | - | - |
|
|
|
|
N | Open lung biopsy | |||
| Obesity[7][8] | + | + | - | - |
|
- | - | - | + | - |
|
|
N | Clinical | |||
| Pulmonary Eosinophilia[9] | + | + | + | + | Infections | + | - | + | + |
|
|
|
|
↓ | Biopsy of lesion (skin or lung) | ||
| Neuromuscular disease | Scoliosis | - | + | - | - |
|
- | - | - | - |
|
|
|
|
|
N |
|
| Muscular dystrophy | - | + | - | - |
|
- | - | - | - |
|
|
|
N | ||||
| ALS | - | + | - | - |
|
- | - | - | - |
|
|
N/A | Not significant/diagnostic | Not significant/diagnostic | - |
| |
| Myasthenia gravis | - | + | - | + | H/O of difficulty getting up from chair
|
- | - | - | - |
|
|
|
|
|
N | ||
References
- ↑ 1.0 1.1 Statement on sarcoidosis: Joint Statement of the American Thoracic Society (ATS), the European Respiratory Society (ERS) and the World Association of Sarcoidosis and Other Granulomatous Disorders (WASOG) adopted by the ATS Board of Directors and by the ERS Executive Committee, February 1999. Am J Respir Crit Care Med 160:736–755, 1999.
- ↑ 2.0 2.1 Judson MA: The diagnosis of sarcoidosis. Clin Chest Med 29(3):415–427, 2008.
- ↑ Gay SE, Kazerooni EA, Toews GB, Lynch JP, Gross BH, Cascade PN, Spizarny DL, Flint A, Schork MA, Whyte RI, Popovich J, Hyzy R, Martinez FJ (1998). "Idiopathic pulmonary fibrosis: predicting response to therapy and survival". Am. J. Respir. Crit. Care Med. 157 (4 Pt 1): 1063–72. doi:10.1164/ajrccm.157.4.9703022. PMID 9563720.
- ↑ du Bois RM (2006). "Evolving concepts in the early and accurate diagnosis of idiopathic pulmonary fibrosis". Clin. Chest Med. 27 (1 Suppl 1): S17–25, v–vi. doi:10.1016/j.ccm.2005.08.001. PMID 16545629.
- ↑ Neghab M, Mohraz MH, Hassanzadeh J (2011). "Symptoms of respiratory disease and lung functional impairment associated with occupational inhalation exposure to carbon black dust". J Occup Health. 53 (6): 432–8. PMID 21996929.
- ↑ Honda O, Johkoh T, Ichikado K, Tomiyama N, Maeda M, Mihara N, Higashi M, Hamada S, Naito H, Yamamoto S, Nakamura H (1999). "Differential diagnosis of lymphocytic interstitial pneumonia and malignant lymphoma on high-resolution CT". AJR Am J Roentgenol. 173 (1): 71–4. doi:10.2214/ajr.173.1.10397102. PMID 10397102.
- ↑ Zammit C, Liddicoat H, Moonsie I, Makker H (2010). "Obesity and respiratory diseases". Int J Gen Med. 3: 335–43. doi:10.2147/IJGM.S11926. PMC 2990395. PMID 21116339.
- ↑ O’Neill, Donal (2015). "Measuring obesity in the absence of a gold standard". Economics & Human Biology. 17: 116–128. doi:10.1016/j.ehb.2015.02.002. ISSN 1570-677X.
- ↑ de Górgolas M, Casado V, Renedo G, Alen JF, Fernández Guerrero ML (2009). "Nodular lung schistosomiais lesions after chemotherapy for dysgerminoma". Am. J. Trop. Med. Hyg. 81 (3): 424–7. PMID 19706907.