Rosuvastatin: Difference between revisions
No edit summary |
No edit summary |
||
| Line 135: | Line 135: | ||
Cases of [[myopathy]], including [[rhabdomyolysis]], have been reported with [[HMG‑CoA reductase inhibitors]], including rosuvastatin, coadministered with [[colchicine]], and caution should be exercised when prescribing rosuvastatin with [[colchicine]]. | Cases of [[myopathy]], including [[rhabdomyolysis]], have been reported with [[HMG‑CoA reductase inhibitors]], including rosuvastatin, coadministered with [[colchicine]], and caution should be exercised when prescribing rosuvastatin with [[colchicine]]. | ||
|FDAPregCat=X | |||
|useInPregnancyFDA=Rosuvastatin is contraindicated in women who are or may become pregnant. Serum [[cholesterol]] and [[triglycerides]] increase during normal [[pregnancy]], and [[cholesterol]] products are essential for [[fetal development]]. [[Atherosclerosis]] is a chronic process and discontinuation of [[lipid-lowering drugs]] during [[pregnancy]] should have little impact on long-term outcomes of primary [[hyperlipidemia]] therapy | |||
There are no adequate and well-controlled studies of rosuvastatin in [[pregnant]] women. There have been rare reports of congenital anomalies following intrauterine exposure to [[HMG CoA reductase inhibitors]]. In a review of about 100 prospectively followed pregnancies in women exposed to other [[HMG CoA reductase inhibitors]], the incidences of [[congenital anomalies]], spontaneous [[abortion]]s, and fetal deaths/[[stillbirth]]s did not exceed the rate expected in the general population. However, this study was only able to exclude a three-to-fourfold increased risk of [[congenital anomalies]] over background incidence. In 89% of these cases, drug treatment started before pregnancy and stopped during the first trimester when pregnancy was identified. | |||
Rosuvastatin crosses the placenta in rats and rabbits. In rats, rosuvastatin was not [[teratogenic]] at systemic exposures equivalent to a human therapeutic dose of 40 mg/day. At 10 12 times the human dose of 40 mg/day, there was decreased pup survival, decreased fetal body weight among female pups, and delayed ossification. In rabbits, pup viability decreased and maternal mortality increased at doses equivalent to the human dose of 40 mg/day | |||
Rosuvastatin may cause fetal harm when administered to a [[pregnant]] woman. If the patient becomes pregnant while taking rosuvastatin, the patient should be apprised of the potential risks to the fetus and the lack of known clinical benefit with continued use during [[pregnancy]]. | |||
|AUSPregCat=D | |||
|useInNursing=It is not known whether rosuvastatin is excreted in human milk, but a small amount of another drug in this class does pass into breast milk. In rats, [[breast milk]] concentrations of rosuvastatin are three times higher than plasma levels; however, animal [[breast milk]] drug levels may not accurately reflect human breast milk levels. Because another drug in this class passes into human milk and because [[HMG‑CoA reductase inhibitors]] have a potential to cause serious adverse reactions in nursing infants, women who require rosuvastatin treatment should be advised not to nurse their infants. | |||
|useInPed=The safety and effectiveness of rosuvastatin in patients 10 to 17 years of age with heterozygous familial hypercholesterolemia were evaluated in a controlled clinical trial of 12 weeks duration followed by 40 weeks of open-label exposure. Patients treated with 5 mg, 10 mg, and 20 mg daily rosuvastatin had an adverse experience profile generally similar to that of patients treated with placebo. Although not all adverse reactions identified in the adult population have been observed in clinical trials of children and adolescent patients, the same warnings and precautions for adults should be considered for children and adolescents. There was no detectable effect of rosuvastatin on growth, weight, BMI (body mass index), or sexual maturation in pediatric patients (10 to 17 years of age). Adolescent females should be counseled on appropriate contraceptive methods while on rosuvastatin therapy. Rosuvastatin has not been studied in controlled clinical trials involving prepubertal patients or patients younger than 10 years of age. Doses of rosuvastatin greater than 20 mg have not been studied in the pediatric population. | |||
In children and adolescents with homozygous familial hypercholesterolemia experience is limited to eight patients (aged 8 years and above). | |||
In a pharmacokinetic study, 18 patients (9 boys and 9 girls) 10 to 17 years of age with heterozygous FH received single and multiple oral doses of rosuvastatin . Both Cmax and AUC of rosuvastatin were similar to values observed in adult subjects administered the same doses. | |||
| | |useInGeri=Of the 10,275 patients in clinical studies with rosuvastatin, 3159 (31%) were 65 years and older, and 698 (6.8%) were 75 years and older. No overall differences in safety or effectiveness were observed between these subjects and younger subjects, and other reported clinical experience has not identified differences in responses between the elderly and younger patients, but greater sensitivity of some older individuals cannot be ruled out. | ||
Elderly patients are at higher risk of myopathy and rosuvastatin should be prescribed with caution in the elderly | |||
|useInRenalImpair=Rosuvastatin exposure is not influenced by mild to moderate renal impairment (CLcr ≥ 30 mL/min/1.73 m2); however, exposure to rosuvastatin is increased to a clinically significant extent in patients with severe renal impairment who are not receiving hemodialysis. Rosuvastatin dosing should be adjusted in patients with severe renal impairment (CLcr < 30 mL/min/1.73 m2) not requiring hemodialysis. | |||
|useInHepaticImpair=Rosuvastatin is contraindicated in patients with active liver disease, which may include unexplained persistent elevations of hepatic transaminase levels. Chronic alcohol liver disease is known to increase rosuvastatin exposure; Rosuvastatin should be used with caution in these patients. | |||
|useInRenalImpair=( | |othersTitle=Asian Patients | ||
|useInOthers=Pharmacokinetic studies have demonstrated an approximate 2‑fold increase in median exposure to rosuvastatin in Asian subjects when compared with Caucasian controls. Rosuvastatin dosage should be adjusted in Asian patients | |||
| | |||
|othersTitle= | |||
|useInOthers= | |||
|administration=(Oral/Intravenous/etc) | |administration=(Oral/Intravenous/etc) | ||
|monitoring======Condition 1===== | |monitoring======Condition 1===== | ||
Revision as of 16:54, 30 June 2014
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]; Associate Editor(s)-in-Chief: Alejandro Lemor, M.D. [2]
Disclaimer
WikiDoc MAKES NO GUARANTEE OF VALIDITY. WikiDoc is not a professional health care provider, nor is it a suitable replacement for a licensed healthcare provider. WikiDoc is intended to be an educational tool, not a tool for any form of healthcare delivery. The educational content on WikiDoc drug pages is based upon the FDA package insert, National Library of Medicine content and practice guidelines / consensus statements. WikiDoc does not promote the administration of any medication or device that is not consistent with its labeling. Please read our full disclaimer here.
Overview
Rosuvastatin is a HMG-CoA reductase inhibitor that is FDA approved for the {{{indicationType}}} of hyperlipidemia and mixed dyslipidemia, hypertriglyceridemia, primary dysbetalipoproteinemia (Type III hyperlipoproteinemia), homozygous familial hypercholesterolemia, slowing of the progression of atherosclerosis, primary prevention of cardiovascular disease. Common adverse reactions include headache, myalgia, abdominal pain, asthenia, and nausea.
Adult Indications and Dosage
FDA-Labeled Indications and Dosage (Adult)
General Dosing Information
- Dosing Information
- 5 to 40 mg orally once daily.
Homozygous Familial Hypercholesterolemia
- Dosing Information
- 20 mg once daily
Off-Label Use and Dosage (Adult)
Guideline-Supported Use
There is limited information regarding Off-Label Guideline-Supported Use of Rosuvastatin in adult patients.
Non–Guideline-Supported Use
Acute Coronary Syndrome
Prophylaxis for Atrial Fibrillation
Prophylaxis for Cardiovascular Event in Percutaneous Coronary Intervention (PCI)
- Dosing Information
- 40 mg preprocedure
Prophylaxis for Venous Thromboembolism
- Dosing Information
- 20 mg/day
Metabolic Syndrome
- Dosing Information
- 10 mg/day
Pediatric Indications and Dosage
FDA-Labeled Indications and Dosage (Pediatric)
Heterozygous Familial Hypercholesterolemia in Pediatric Patients (10 to 17 years of age)
- Dosing Information
- 5‑20 mg/day; the maximum recommended dose is 20 mg/day
Off-Label Use and Dosage (Pediatric)
Guideline-Supported Use
There is limited information regarding Off-Label Guideline-Supported Use of Rosuvastatin in pediatric patients.
Non–Guideline-Supported Use
There is limited information regarding Off-Label Non–Guideline-Supported Use of Rosuvastatin in pediatric patients.
Contraindications
- Patients with a known hypersensitivity to any component of this product. Hypersensitivity reactions including rash, pruritus, urticaria, and angioedema have been reported with rosuvastatin.
- Patients with active liver disease, which may include unexplained persistent elevations of hepatic transaminase levels.
- Women who are pregnant or may become pregnant. Because HMG‑CoA reductase inhibitors decrease cholesterol synthesis and possibly the synthesis of other biologically active substances derived from cholesterol, rosuvastatin may cause fetal harm when administered to regnant women. Additionally, there is no apparent benefit to therapy during pregnancy, and safety in pregnant women has not been established. If the patient becomes pregnant while taking this drug, the patient should be apprised of the potential hazard to the fetus and the lack of known clinical benefit with continued use during pregnancy.
- Nursing mothers. Because another drug in this class passes into breast milk, and because HMG‑CoA reductase inhibitors have the potential to cause serious adverse reactions in nursing infants, women who require rosuvastatin treatment should be advised not to nurse their infants.
Warnings
Skeletal Muscle Effects
Cases of myopathy and rhabdomyolysis with acute renal failure secondary to myoglobinuria have been reported with HMG-CoA reductase inhibitors, including Rosuvastatin. These risks can occur at any dose level, but are increased at the highest dose (40 mg).
Rosuvastatin should be prescribed with caution in patients with predisposing factors for myopathy (e.g., age ≥ 65 years, inadequately treated hypothyroidism, renal impairment).
The risk of myopathy during treatment with Rosuvastatin may be increased with concurrent administration of some other lipid-lowering therapies (fibrates or niacin), gemfibrozil, cyclosporine, lopinavir/ritonavir, or atazanavir/ritonavir. Cases of myopathy, including rhabdomyolysis, have been reported with HMG-CoA reductase inhibitors, including rosuvastatin, coadministered with colchicine, and caution should be exercised when prescribing Rosuvastatin with colchicine.
Rosuvastatin therapy should be discontinued if markedly elevated creatine kinase levels occur or myopathy is diagnosed or suspected. Rosuvastatin therapy should also be temporarily withheld in any patient with an acute, serious condition suggestive of myopathy or predisposing to the development of renal failure secondary to rhabdomyolysis (e.g., sepsis, hypotension, dehydration, major surgery, trauma, severe metabolic, endocrine, and electrolyte disorders, or uncontrolled seizures).
There have been rare reports of immune-mediated necrotizing myopathy (IMNM), an autoimmune myopathy, associated with statin use. IMNM is characterized by: proximal muscle weakness and elevated serum creatine kinase, which persist despite discontinuation of statin treatment; muscle biopsy showing necrotizing myopathy without significant inflammation; improvement with immunosuppressive agents.
All patients should be advised to promptly report to their physician unexplained muscle pain, tenderness, or weakness, particularly if accompanied by malaise or fever or if muscle signs and symptoms persist after discontinuing Rosuvastatin.
Liver Enzyme Abnormalities
It is recommended that liver enzyme tests be performed before the initiation of Rosuvastatin, and if signs or symptoms of liver injury occur.
Increases in serum transaminases AST (SGOT) or ALT (SGPT)] have been reported with HMG‑CoA reductase inhibitors, including Rosuvastatin. In most cases, the elevations were transient and resolved or improved on continued therapy or after a brief interruption in therapy. There were two cases of jaundice, for which a relationship to Rosuvastatin therapy could not be determined, which resolved after discontinuation of therapy. There were no cases of liver failure or irreversible liver disease in these trials.
In a pooled analysis of placebo-controlled trials, increases in serumtransaminases to >3 times the upper limit of normal occurred in 1.1% of patients taking Rosuvastatin versus 0.5% of patients treated with placebo.
There have been rare postmarketing reports of fatal and non-fatal hepatic failure in patients taking statins, including rosuvastatin. If serious liver injury with clinical symptoms and/or hyperbilirubinemia or jaundice occurs during treatment with Rosuvastatin, promptly interrupt therapy. If an alternate etiology is not found, do not restart Rosuvastatin.
Rosuvastatin should be used with caution in patients who consume substantial quantities of alcohol and/or have a history of chronic liver disease. Active liver disease, which may include unexplained persistent transaminase elevations, is a contraindication to the use of Rosuvastatin.
Concomitant Coumarin Anticoagulants
Caution should be exercised when anticoagulants are given in conjunction with Rosuvastatin because of its potentiation of the effect of coumarin-type anticoagulants in prolonging the prothrombin time/INR. In patients taking coumarin anticoagulants and Rosuvastatin concomitantly, INR should be determined before starting Rosuvastatin and frequently enough during early therapy to ensure that no significant alteration of INR occurs.
Proteinuria and Hematuria
In the Rosuvastatin clinical trial program, dipstick-positive proteinuria and microscopic hematuria were observed among Rosuvastatin treated patients. These findings were more frequent in patients taking Rosuvastatin 40 mg, when compared to lower doses of Rosuvastatin or comparator HMG‑CoA reductase inhibitors, though it was generally transient and was not associated with worsening renal function. Although the clinical significance of this finding is unknown, a dose reduction should be considered for patients on Rosuvastatin therapy with unexplained persistent proteinuria and/or hematuria during routine urinalysis testing.
Endocrine Effects
Increases in HbA1c and fasting serum glucose levels have been reported with HMG‑CoA reductase inhibitors, including Rosuvastatin. Based on clinical trial data with Rosuvastatin, in some instances these increases may exceed the threshold for the diagnosis of diabetes mellitus.
Although clinical studies have shown that Rosuvastatin alone does not reduce basal plasma cortisol concentration or impair adrenal reserve, caution should be exercised if Rosuvastatin is administered concomitantly with drugs that may decrease the levels or activity of endogenous steroid hormones such as ketoconazole, spironolactone, and cimetidine.
Adverse Reactions
Clinical Trials Experience
Because clinical studies are conducted under widely varying conditions, adverse reaction rates observed in the clinical studies of a drug cannot be directly compared to rates in the clinical studies of another drug and may not reflect the rates observed in clinical practice.
Adverse reactions reported in ≥ 2% of patients in placebo-controlled clinical studies and at a rate greater than placebo are shown in Table 1. These studies had a treatment duration of up to 12 weeks.
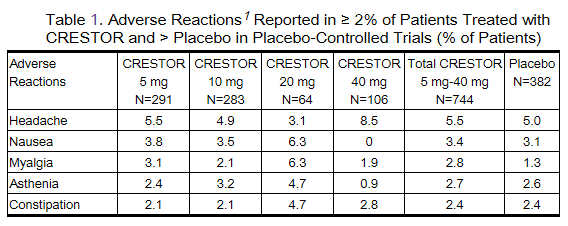
Other adverse reactions reported in clinical studies were abdominal pain, dizziness, hypersensitivity (including rash, pruritus, urticaria, and angioedema) and pancreatitis. The following laboratory abnormalities have also been reported: dipstick-positive proteinuria and microscopic hematuria; elevated creatine phosphokinase, transaminases, glucose, glutamyl transpeptidase, alkaline phosphatase, and bilirubin; and thyroid function abnormalities.
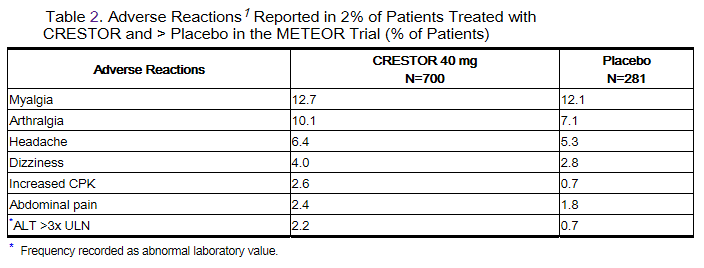
In the METEOR study, involving 981 participants treated with rosuvastatin 40 mg (n=700) or placebo (n=281) with a mean treatment duration of 1.7 years, 5.6% of subjects treated with rosuvastatin versus 2.8% of placebo-treated subjects discontinued due to adverse reactions. The most common adverse reactions that led to treatment discontinuation were: myalgia, hepatic enzyme increased, headache, and nausea.
Adverse reactions reported in ≥ 2% of patients and at a rate greater than placebo are shown in Table 2.
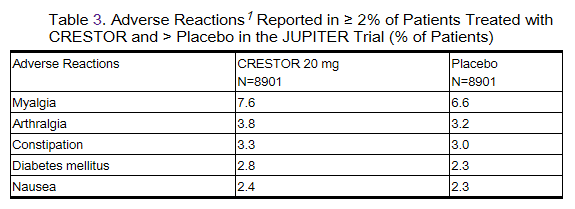
In the JUPITER study, 17,802 participants were treated with rosuvastatin 20 mg (n=8901) or placebo (n=8901) for a mean duration of 2 years. A higher percentage of rosuvastatin-treated patients versus placebo-treated patients, 6.6% and 6.2%, respectively, discontinued study medication due to an adverse event, irrespective of treatment causality. Myalgia was the most common adverse reaction that led to treatment discontinuation.
In JUPITER, there was a significantly higher frequency of diabetes mellitus reported in patients taking rosuvastatin (2.8%) versus patients taking placebo (2.3%). Mean HbA1c was significantly increased by 0.1% in rosuvastatin-treated patients compared to placebo-treated patients. The number of patients with a HbA1c > 6.5% at the end of the trial was significantly higher in rosuvastatin-treated versus placebo-treated patients.
Adverse reactions reported in ≥ 2% of patients and at a rate greater than placebo are shown in Table 3.
Postmarketing Experience
The following adverse reactions have been identified during postapproval use of rosuvastatin : arthralgia, fatal and non-fatal hepatic failure, hepatitis, jaundice, thrombocytopenia, depression, sleep disorders (including insomnia and nightmares) and gynecomastia. Because these reactions are reported voluntarily from a population of uncertain size, it is not always possible to reliably estimate their frequency or establish a causal relationship to drug exposure.
There have been rare reports of immune-mediated necrotizing myopathy associated with statin use.
There have been rare postmarketing reports of cognitive impairment (e.g., memory loss, forgetfulness, amnesia, memory impairment, confusion) associated with statin use. These cognitive issues have been reported for all statins. The reports are generally nonserious, and reversible upon statin discontinuation, with variable times to symptom onset (1 day to years) and symptom resolution (median of 3 weeks).
Drug Interactions
Cyclosporine
Cyclosporine increased rosuvastatin exposure (AUC) 7‑fold. Therefore, in patients taking cyclosporine, the dose of rosuvastatin should not exceed 5 mg once daily.
Gemfibrozil
Gemfibrozil significantly increased rosuvastatin exposure. Due to an observed increased risk of myopathy/rhabdomyolysis, combination therapy with rosuvastatin and gemfibrozil should be avoided. If used together, the dose of rosuvastatin should not exceed 10 mg once daily.
Protease Inhibitors
Coadministration of rosuvastatin with certain protease inhibitors given in combination with ritonavir has differing effects on rosuvastatin exposure. The protease inhibitor combinations lopinavir/ritonavir and atazanavir/ritonavir increase rosuvastatin exposure (AUC) up to threefold. For these combinations the dose of rosuvastatin should not exceed 10 mg once daily. The combinations of tipranavir/ritonavir or fosamprenavir/ritonavir produce little or no change in rosuvastatin exposure. Caution should be exercised when rosuvastatin is coadministered with protease inhibitors given in combination with ritonavir.
Coumarin Anticoagulants
Rosuvastatin significantly increased INR in patients receiving coumarin anticoagulants. Therefore, caution should be exercised when coumarin anticoagulants are given in conjunction with rosuvastatin. In patients taking coumarin anticoagulants and rosuvastatin concomitantly, INR should be determined before starting rosuvastatin and frequently enough during early therapy to ensure that no significant alteration of INR] occurs.
Niacin
The risk of skeletal muscle effects may be enhanced when rosuvastatin is used in combination with lipid-modifying doses (≥1 g/day) of niacin; caution should be used when prescribing with rosuvastatin.
Fenofibrate
When rosuvastatin was coadministered with fenofibrate, no clinically significant increase in the AUC of rosuvastatin or fenofibrate was observed. Because it is known that the risk of myopathy during treatment with HMG-CoA reductase inhibitors is increased with concomitant use of fenofibrates, caution should be used when prescribing fenofibrates with rosuvastatin.
Colchicine
Cases of myopathy, including rhabdomyolysis, have been reported with HMG‑CoA reductase inhibitors, including rosuvastatin, coadministered with colchicine, and caution should be exercised when prescribing rosuvastatin with colchicine.
Use in Specific Populations
Pregnancy
Pregnancy Category (FDA): X
Rosuvastatin is contraindicated in women who are or may become pregnant. Serum cholesterol and triglycerides increase during normal pregnancy, and cholesterol products are essential for fetal development. Atherosclerosis is a chronic process and discontinuation of lipid-lowering drugs during pregnancy should have little impact on long-term outcomes of primary hyperlipidemia therapy
There are no adequate and well-controlled studies of rosuvastatin in pregnant women. There have been rare reports of congenital anomalies following intrauterine exposure to HMG CoA reductase inhibitors. In a review of about 100 prospectively followed pregnancies in women exposed to other HMG CoA reductase inhibitors, the incidences of congenital anomalies, spontaneous abortions, and fetal deaths/stillbirths did not exceed the rate expected in the general population. However, this study was only able to exclude a three-to-fourfold increased risk of congenital anomalies over background incidence. In 89% of these cases, drug treatment started before pregnancy and stopped during the first trimester when pregnancy was identified.
Rosuvastatin crosses the placenta in rats and rabbits. In rats, rosuvastatin was not teratogenic at systemic exposures equivalent to a human therapeutic dose of 40 mg/day. At 10 12 times the human dose of 40 mg/day, there was decreased pup survival, decreased fetal body weight among female pups, and delayed ossification. In rabbits, pup viability decreased and maternal mortality increased at doses equivalent to the human dose of 40 mg/day
Rosuvastatin may cause fetal harm when administered to a pregnant woman. If the patient becomes pregnant while taking rosuvastatin, the patient should be apprised of the potential risks to the fetus and the lack of known clinical benefit with continued use during pregnancy.
Pregnancy Category (AUS): D
There is no Australian Drug Evaluation Committee (ADEC) guidance on usage of Rosuvastatin in women who are pregnant.
Labor and Delivery
There is no FDA guidance on use of Rosuvastatin during labor and delivery.
Nursing Mothers
It is not known whether rosuvastatin is excreted in human milk, but a small amount of another drug in this class does pass into breast milk. In rats, breast milk concentrations of rosuvastatin are three times higher than plasma levels; however, animal breast milk drug levels may not accurately reflect human breast milk levels. Because another drug in this class passes into human milk and because HMG‑CoA reductase inhibitors have a potential to cause serious adverse reactions in nursing infants, women who require rosuvastatin treatment should be advised not to nurse their infants.
Pediatric Use
The safety and effectiveness of rosuvastatin in patients 10 to 17 years of age with heterozygous familial hypercholesterolemia were evaluated in a controlled clinical trial of 12 weeks duration followed by 40 weeks of open-label exposure. Patients treated with 5 mg, 10 mg, and 20 mg daily rosuvastatin had an adverse experience profile generally similar to that of patients treated with placebo. Although not all adverse reactions identified in the adult population have been observed in clinical trials of children and adolescent patients, the same warnings and precautions for adults should be considered for children and adolescents. There was no detectable effect of rosuvastatin on growth, weight, BMI (body mass index), or sexual maturation in pediatric patients (10 to 17 years of age). Adolescent females should be counseled on appropriate contraceptive methods while on rosuvastatin therapy. Rosuvastatin has not been studied in controlled clinical trials involving prepubertal patients or patients younger than 10 years of age. Doses of rosuvastatin greater than 20 mg have not been studied in the pediatric population.
In children and adolescents with homozygous familial hypercholesterolemia experience is limited to eight patients (aged 8 years and above).
In a pharmacokinetic study, 18 patients (9 boys and 9 girls) 10 to 17 years of age with heterozygous FH received single and multiple oral doses of rosuvastatin . Both Cmax and AUC of rosuvastatin were similar to values observed in adult subjects administered the same doses.
Geriatic Use
Of the 10,275 patients in clinical studies with rosuvastatin, 3159 (31%) were 65 years and older, and 698 (6.8%) were 75 years and older. No overall differences in safety or effectiveness were observed between these subjects and younger subjects, and other reported clinical experience has not identified differences in responses between the elderly and younger patients, but greater sensitivity of some older individuals cannot be ruled out.
Elderly patients are at higher risk of myopathy and rosuvastatin should be prescribed with caution in the elderly
Gender
There is no FDA guidance on the use of Rosuvastatin with respect to specific gender populations.
Race
There is no FDA guidance on the use of Rosuvastatin with respect to specific racial populations.
Renal Impairment
Rosuvastatin exposure is not influenced by mild to moderate renal impairment (CLcr ≥ 30 mL/min/1.73 m2); however, exposure to rosuvastatin is increased to a clinically significant extent in patients with severe renal impairment who are not receiving hemodialysis. Rosuvastatin dosing should be adjusted in patients with severe renal impairment (CLcr < 30 mL/min/1.73 m2) not requiring hemodialysis.
Hepatic Impairment
Rosuvastatin is contraindicated in patients with active liver disease, which may include unexplained persistent elevations of hepatic transaminase levels. Chronic alcohol liver disease is known to increase rosuvastatin exposure; Rosuvastatin should be used with caution in these patients.
Females of Reproductive Potential and Males
There is no FDA guidance on the use of Rosuvastatin in women of reproductive potentials and males.
Immunocompromised Patients
There is no FDA guidance one the use of Rosuvastatin in patients who are immunocompromised.
Asian Patients
Pharmacokinetic studies have demonstrated an approximate 2‑fold increase in median exposure to rosuvastatin in Asian subjects when compared with Caucasian controls. Rosuvastatin dosage should be adjusted in Asian patients
Administration and Monitoring
Administration
(Oral/Intravenous/etc)
Monitoring
Condition 1
(Description regarding monitoring, from Warnings section)
Condition 2
(Description regarding monitoring, from Warnings section)
Condition 3
(Description regarding monitoring, from Warnings section)
IV Compatibility
Solution
Compatible
- Solution 1
- Solution 2
- Solution 3
Not Tested
- Solution 1
- Solution 2
- Solution 3
Variable
- Solution 1
- Solution 2
- Solution 3
Incompatible
- Solution 1
- Solution 2
- Solution 3
Y-Site
Compatible
- Solution 1
- Solution 2
- Solution 3
Not Tested
- Solution 1
- Solution 2
- Solution 3
Variable
- Solution 1
- Solution 2
- Solution 3
Incompatible
- Solution 1
- Solution 2
- Solution 3
Admixture
Compatible
- Solution 1
- Solution 2
- Solution 3
Not Tested
- Solution 1
- Solution 2
- Solution 3
Variable
- Solution 1
- Solution 2
- Solution 3
Incompatible
- Solution 1
- Solution 2
- Solution 3
Syringe
Compatible
- Solution 1
- Solution 2
- Solution 3
Not Tested
- Solution 1
- Solution 2
- Solution 3
Variable
- Solution 1
- Solution 2
- Solution 3
Incompatible
- Solution 1
- Solution 2
- Solution 3
TPN/TNA
Compatible
- Solution 1
- Solution 2
- Solution 3
Not Tested
- Solution 1
- Solution 2
- Solution 3
Variable
- Solution 1
- Solution 2
- Solution 3
Incompatible
- Solution 1
- Solution 2
- Solution 3
Overdosage
Acute Overdose
Signs and Symptoms
(Description)
Management
(Description)
Chronic Overdose
Signs and Symptoms
(Description)
Management
(Description)
Pharmacology
| |
Rosuvastatin
| |
| Systematic (IUPAC) name | |
| ? | |
| Identifiers | |
| CAS number | ? |
| ATC code | ? |
| PubChem | ? |
| Chemical data | |
| Formula | ? |
| Mol. mass | ? |
| Pharmacokinetic data | |
| Bioavailability | ? |
| Metabolism | ? |
| Half life | ? |
| Excretion | ? |
| Therapeutic considerations | |
| Pregnancy cat. |
? |
| Legal status | |
| Routes | ? |
Mechanism of Action
(Description)
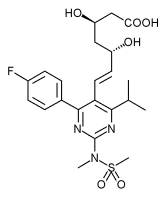
Structure
(Description with picture)
Pharmacodynamics
(Description)
Pharmacokinetics
(Description)
Nonclinical Toxicology
(Description)
Clinical Studies
Condition 1
(Description)
Condition 2
(Description)
Condition 3
(Description)
How Supplied
(Description)
Storage
There is limited information regarding Rosuvastatin Storage in the drug label.
Images
Drug Images
{{#ask: Page Name::Rosuvastatin |?Pill Name |?Drug Name |?Pill Ingred |?Pill Imprint |?Pill Dosage |?Pill Color |?Pill Shape |?Pill Size (mm) |?Pill Scoring |?NDC |?Drug Author |format=template |template=DrugPageImages |mainlabel=- |sort=Pill Name }}
Package and Label Display Panel
{{#ask: Label Page::Rosuvastatin |?Label Name |format=template |template=DrugLabelImages |mainlabel=- |sort=Label Page }}
Patient Counseling Information
(Patient Counseling Information)
Precautions with Alcohol
Alcohol-Rosuvastatin interaction has not been established. Talk to your doctor about the effects of taking alcohol with this medication.
Brand Names
There is limited information regarding Rosuvastatin Brand Names in the drug label.
Look-Alike Drug Names
- (Paired Confused Name 1a) — (Paired Confused Name 1b)
- (Paired Confused Name 2a) — (Paired Confused Name 2b)
- (Paired Confused Name 3a) — (Paired Confused Name 3b)
Drug Shortage Status
Drug Shortage
Price
References
The contents of this FDA label are provided by the National Library of Medicine.