Rocky Mountain spotted fever: Difference between revisions
| Line 56: | Line 56: | ||
==Treatment== | ==Treatment== | ||
[[Rocky Mountain spotted fever medical therapy|Medical therapy]] | [[Rocky Mountain spotted fever surgery|Surgical options]] | [[Rocky Mountain spotted fever primary prevention|Primary prevention]] | [[Rocky Mountain spotted fever secondary prevention|Secondary prevention]] | [[Rocky Mountain spotted fever cost-effectiveness of therapy|Financial costs]] | [[Rocky Mountain spotted fever future or investigational therapies|Future therapies]] | [[Rocky Mountain spotted fever medical therapy|Medical therapy]] | [[Rocky Mountain spotted fever surgery|Surgical options]] | [[Rocky Mountain spotted fever primary prevention|Primary prevention]] | [[Rocky Mountain spotted fever secondary prevention|Secondary prevention]] | [[Rocky Mountain spotted fever cost-effectiveness of therapy|Financial costs]] | [[Rocky Mountain spotted fever future or investigational therapies|Future therapies]] | ||
== Treatment == | == Treatment == | ||
Revision as of 19:21, 7 February 2012
For patient information click here.
| Rickettsia rickettsii | ||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Scientific classification | ||||||||||||||
| ||||||||||||||
| Binomial name | ||||||||||||||
| Rickettsia rickettsii Wolbach, 1919 |
Template:DiseaseDisorder infobox
|
Rocky Mountain spotted fever Microchapters |
|
Differentiating Rocky Mountain spotted fever from other Diseases |
|---|
|
Diagnosis |
|
Treatment |
|
Case Studies |
|
Rocky Mountain spotted fever On the Web |
|
American Roentgen Ray Society Images of Rocky Mountain spotted fever |
|
Directions to Hospitals Treating Rocky Mountain spotted fever |
|
Risk calculators and risk factors for Rocky Mountain spotted fever |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]
Please Take Over This Page and Apply to be Editor-In-Chief for this topic: There can be one or more than one Editor-In-Chief. You may also apply to be an Associate Editor-In-Chief of one of the subtopics below. Please mail us [2] to indicate your interest in serving either as an Editor-In-Chief of the entire topic or as an Associate Editor-In-Chief for a subtopic. Please be sure to attach your CV and or biographical sketch.
Overview
Historical Perspective
Pathophysiology
Epidemiology & Demographics
Risk Factors
Screening
Causes
Differentiating Rocky Mountain spotted fever
Complications & Prognosis
Diagnosis
History and Symptoms | Physical Examination | Laboratory tests | Electrocardiogram | X Rays | CT | MRI Echocardiography or Ultrasound | Other images | Alternative diagnostics
Treatment
Medical therapy | Surgical options | Primary prevention | Secondary prevention | Financial costs | Future therapies
Treatment
Appropriate antibiotic treatment should be initiated immediately when there is a suspicion of Rocky Mountain spotted fever on the basis of clinical and epidemiologic findings. Treatment should not be delayed until laboratory confirmation is obtained.
If the patient is treated within the first 4-5 days of the disease, fever generally subsides within 24-72 hours after treatment with an appropriate antibiotic (usually in the tetracycline class). In fact, failure to respond to a tetracycline antibiotic argues against a diagnosis of RMSF. Severely ill patients may require longer periods before their fever resolves, especially if they have experienced damage to multiple organ systems. Preventive therapy in non-ill patients who have had recent tick bites is not recommended and may, in fact, only delay the onset of disease.

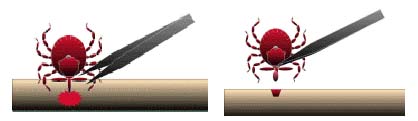
What is the best way to remove a tick?
- Use fine-tipped tweezers or notched tick extractor, and protect your fingers with a tissue, paper towel, or latex gloves. Persons should avoid removing ticks with bare hands.
- Grasp the tick as close to the skin surface as possible and pull upward with steady, even pressure. Do not twist or jerk the tick; this may cause the mouthparts to break off and remain in the skin. (If this happens, remove mouthparts with tweezers. Consult your health care provider if illness occurs.)
- After removing the tick, thoroughly disinfect the bite site and wash your hands with soap and water.
- Do not squeeze, crush, or puncture the body of the tick because its fluids may contain infectious organisms. Skin accidentally exposed to tick fluids can be disinfected with iodine scrub, rubbing alcohol, or water containing detergents.
- Save the tick for identification in case you become ill. This may help your doctor to make an accurate diagnosis. Place the tick in a sealable plastic bag and put it in your freezer. Write the date of the bite on a piece of paper with a pencil and place it in the bag.
Do folklore remedies work?
No. Folklore remedies, such as the use of petroleum jelly or hot matches, do little to encourage a tick to detach from skin. In fact, they may make matters worse by irritating the tick and stimulating it to release additional saliva or regurgitate gut contents, increasing the chances of transmitting the pathogen. These methods of tick removal should be avoided.
Pharmacotherapy
Doxycycline (100 mg every 12 hours for adults or 4 mg/kg body weight per day in two divided doses for children under 45 kg [100 lbs]) is the drug of choice for patients with Rocky Mountain spotted fever. Therapy is continued for at least 3 days after fever subsides and until there is unequivocal evidence of clinical improvement, generally for a minimum total course of 5 to 10 days. Severe or complicated disease may require longer treatment courses. Doxycycline is also the preferred drug for patients with ehrlichiosis, another tick-transmitted infection with signs and symptoms that may resemble Rocky Mountain spotted fever.
Tetracyclines are usually not the preferred drug for use in pregnant women because of risks associated with malformation of teeth and bones in unborn children. Chloramphenicol is an alternative drug that can be used to treat Rocky Mountain spotted fever; however, this drug may be associated with a wide range of side effects and may require careful monitoring of blood levels.
Prevention
Primary Prevention

Limiting exposure to ticks reduces the likelihood of infection with Rocky Mountain spotted fever. In persons exposed to tick-infested habitats, prompt careful inspection and removal of crawling or attached ticks is an important method of preventing disease. It may take extended attachment time before organisms are transmitted from the tick to the host.
It is unreasonable to assume that a person can completely eliminate activities that may result in tick exposure. Therefore, prevention measures should emphasize personal protection when exposed to natural areas where ticks are present:
- Wear light-colored clothing which allows you to see ticks that are crawling on your clothing.
- Tuck your pants legs into your socks so that ticks cannot crawl up the inside of your pants legs.
- Apply repellents to discourage tick attachment. Repellents containing permethrin can be sprayed on boots and clothing, and will last for several days. Repellents containing DEET (n, n-diethyl-m-toluamide) can be applied to the skin, but will last only a few hours before reapplication is necessary. Use DEET with caution on children. Application of large amounts of DEET on children has been associated with adverse reactions.
- Conduct a body check upon return from potentially tick-infested areas by searching your entire body for ticks. Use a hand-held or full-length mirror to view all parts of your body. Remove any tick you find on your body.
- Parents should check their children for ticks, especially in the hair, when returning from potentially tick-infested areas. *Ticks may also be carried into the household on clothing and pets and only attach later, so both should be examined carefully to exclude ticks.
Secondary Prevention
Tick Control
Strategies to reduce populations of vector ticks through area-wide application of acaricides (chemicals that will kill ticks and mites) and control of tick habitats (e.g., leaf litter and brush) have been effective in small-scale trials. New methods being developed include applying acaricides to animal hosts by using baited tubes, boxes, and feeding stations in areas where these pathogens are endemic. Biological control with fungi, parasitic nematodes, and parasitic wasps may play supportive roles in integrated tick control efforts. Community-based, integrated, tick-management strategies may prove to be an effective public health response to reduce the incidence of tick-borne infections. However, limiting exposure to ticks is currently the most effective method of prevention of tick-transmitted diseases.
History
Rocky Mountain spotted fever was first recognized in 1896 in the Snake River Valley of Idaho and was originally called “black measles” because of the characteristic rash. It was a dreaded and frequently fatal disease that affected hundreds of people in this area. By the early 1900s, the recognized geographic distribution of this disease grew to encompass parts of the United States as far north as Washington and Montana and as far south as California, Arizona, and New Mexico.
Howard T. Ricketts was the first to establish the identity of the infectious organism that causes this disease. He and others characterized the basic epidemiological features of the disease, including the role of tick vectors. Their studies found that Rocky Mountain spotted fever is caused by Rickettsia rickettsii. This species is maintained in nature by a complex cycle involving ticks and mammals; humans are considered to be accidental hosts and are not involved in the natural transmission cycle of this pathogen. Tragically—and ironically—Dr. Ricketts died of typhus (another rickettsial disease) in Mexico in 1910, shortly after completing his remarkable studies on Rocky Mountain spotted fever.
References
http://www.cdc.gov/ncidod/diseases/submenus/sub_rmsf.htm
External links
| Wikimedia Commons has media related to Rocky Mountain spotted fever. |
Template:Wikispecies Template:Wikispecies
- Association of State and Territorial Directors of Health Promotion and Public Health Education
- Centers for Disease Control - Rocky Mountain spotted fever
Template:SIB Template:Bacterial diseases de:Rocky-Mountains-Fleckfieber eo:Makula febro uk:Висипний тиф Скелястих Гір