Rhinoplasty: Difference between revisions
m (Robot: Automated text replacement (-{{SIB}} +, -{{EH}} +, -{{EJ}} +, -{{Editor Help}} +, -{{Editor Join}} +)) |
m (Robot: Automated text replacement (-{{reflist}} +{{reflist|2}}, -<references /> +{{reflist|2}}, -{{WikiDoc Cardiology Network Infobox}} +)) |
||
| Line 170: | Line 170: | ||
== References == | == References == | ||
{{reflist}} | {{reflist|2}} | ||
<!-- This section is quite cluttered and it would be best if it were reduced We could keep the best items in the list, but I am not in the position to do this. | <!-- This section is quite cluttered and it would be best if it were reduced We could keep the best items in the list, but I am not in the position to do this. | ||
Latest revision as of 14:27, 6 September 2012
|
WikiDoc Resources for Rhinoplasty |
|
Articles |
|---|
|
Most recent articles on Rhinoplasty Most cited articles on Rhinoplasty |
|
Media |
|
Powerpoint slides on Rhinoplasty |
|
Evidence Based Medicine |
|
Clinical Trials |
|
Ongoing Trials on Rhinoplasty at Clinical Trials.gov Clinical Trials on Rhinoplasty at Google
|
|
Guidelines / Policies / Govt |
|
US National Guidelines Clearinghouse on Rhinoplasty
|
|
Books |
|
News |
|
Commentary |
|
Definitions |
|
Patient Resources / Community |
|
Patient resources on Rhinoplasty Discussion groups on Rhinoplasty Patient Handouts on Rhinoplasty Directions to Hospitals Treating Rhinoplasty Risk calculators and risk factors for Rhinoplasty
|
|
Healthcare Provider Resources |
|
Causes & Risk Factors for Rhinoplasty |
|
Continuing Medical Education (CME) |
|
International |
|
|
|
Business |
|
Experimental / Informatics |
Editors-In-Chief: Martin I. Newman, M.D., FACS, Cleveland Clinic Florida [1]; Michel C. Samson, M.D., FRCSC, FACS [2]; Jay Pensler, M.D., Northwestern University Feinberg School of Medicine [3]
Overview
Rhinoplasty (Template:Lang-el, "Nose" + [Plassein] error: {{lang}}: text has italic markup (help), "to shape") is a surgical procedure which is usually performed by either an Plastic Surgeon, otolaryngologist-head and neck surgeon, or maxillofacial surgeon, or in order to improve the function (reconstructive surgery) and/or the appearance (cosmetic surgery) of a human nose. Rhinoplasty is also commonly called a "nose reshaping" or "nose job". Rhinoplasty can be performed to meet aesthetic goals or for reconstructive purposes to correct trauma, birth defects or breathing problems. It can be combined with other surgical procedures such as chin augmentation to enhance the aesthetic results.
History
Rhinoplasty was first developed by Sushruta, an important physician (often regarded as the "father of plastic surgery") who lived in ancient India circa 500 BC, which he first described in his text Sushruta Samhita. He and his later students and disciples used rhinoplasty to reconstruct noses that were amputated as a punishment for crimes. The techniques of forehead flap rhinoplasty he developed are practiced almost unchanged to this day. This knowledge of plastic surgery existed in India up to the late 18th century as can be seen from the reports published in Gentleman's Magazine (October, 1794).
The first intranasal rhinoplasty in the West was performed by John Orlando Roe in 1887. It was later used for cosmetic purposes by Jacques Joseph (b. Jakob Lewin Joseph) in 1898 to help a patient who felt that the shape or size of his nose caused embarrassment and social discomfort. Joseph's first rhinoplasty patient was a young man whose large nose caused him such embarrassment that he felt unable to appear in public. He approached Joseph because he had heard of a previous successful otoplasty, or "ear reshaping," which the surgeon had performed.

Rhinoplasty can be performed under a general anesthetic, sedation, or with local anesthetic. Initially, local anesthesia which is a mixture of lidocaine and epinephrine is injected to numb the area, and temporarily reduce vascularity. There are two possible approaches to the nose: closed approach and open approach. In closed rhinoplasty, incisions are made inside the nostrils. In open rhynoplasty, an additional inconspicuous incision is made across the columella, the bit of skin that separates the nostrils. The surgeon first separates the skin and soft tissues of the nose from the underlying structures. Reshapes the cartilage and bone, and then sutures the incisions closed. Some surgeons use a stent or packin inside the nose, followed by tape or stent on the outside.
The patient returns home after the surgery. Most surgeons recommend antibiotics, pain medications, and steroid medication after surgery. Most people choose to remain home for a week, although it is safe to be outdoors. If there are external sutures, they are usually removed 4 to 5 days after surgery. The external cast is removed at one week. If there are internal stents, they are usually removed at four days to two weeks. The periorbital bruising usually lasts two weeks. Due to wound healing, there is moderate shifting and settling of the nose over the first year.
In some cases, the surgeon may shape a small piece of the patient's own cartilage or bone, as a graft, to strengthen or change the shape of the nose. Usually the cartilage is harvested from the septum If there isn't enough septum cartilage, which can occur in revision rhinoplasty, cartilage can be harvested from the concha of the ear or the ribs. In the rare case where bone is required, it is harvested from the cranium, the hip, or the ribs. Sometimes a synthetic implant may be used to augment the bridge of the nose.
To improve nasal breathing function, a septoplasty may also be performed. If there is turbinate hypertrophy, an inferior turbinectomy can be done.
Although rhinoplasty is usually considered to be safe and successful, several complications can arise. Post operative bleeding is uncommon and often resolves without needing treatment. Infection is rare and can occasionally progress to an abscess that requires surgical drainage under general anesthetic. Adhesions, which are scars that form to bridge across the nasal cavity from the septum to the turbinates, are also rare but cause nasal obstruction to breathing and usually need to be cut away. A hole can be inadvertently made at the time of surgery in the septum, called a septal perforation. This can cause chronic nose bleeding, crusting, difficult breathing and whistling with breathing.
If too much of the underlying structure of the nose (cartilage and/or bone) is removed, this can cause the overlying nasal skin to have little shape resulting in a "polly beak" deformity. Likewise if the septum is not supported, the bridge of the nose can sink resulting in a "saddle nose" deformity. The tip of the nose can be over-rotated causing the nostrils to be too visible and creating a pig-like look. If the cartilages of the tip of the nose are over-resected, this can cause a pinched look to the tip. If an incision is made across the collumella (open approach rhinoplasty) there can be variable degree of numbness to the nose that may take months to resolve.
The cost of rhinoplasty varies regionally and between surgeons. If it is for functional reasons, like breathing correction, it can be covered by many health plans. For example in 2006 in Ontario, Canada the provincial health insurance carrier paid $480, while the cost for cosmetic rhinoplasty varied between $1,000 and $10,000.
Ethnic rhinoplasty
Although techniques and methods employed during rhinoplasty surgeries are the same regardless of race, there are some trends that apply to patients of certain ethnic backgrounds, due to their similar anatomic features.
East Asian patients often want their noses to appear narrower and their bridges higher. If very little elevation of the bridge is desired, the nasal bones can be cut and moved towards the midline. This technique will narrow the brige and also cause a slight elevation in the dorsum. East Asian patients who seek greater augmentation of the bridge of their nose require implants. A variety of alloplastic implants including Gore-Tex, Med-Por, or silicone can be used. Tissues from the patient's own body (autologous) can be used for augmentation, in order to reduce the risk of complications such as infection or extrusion. Septum cartilage, rib cartilage (costal cartilage), ear cartilage (auricular cartilage), and fascia are being often used. In non surgical rhinoplasty, filler materials such as hyaluronic acid or calcium based microspheres can be injected under the skin, in the bridge of the nose. These injections however, are non permanent lasting between six months to a year.
Patients of African descent commonly seek narrowing of wide nostrils in a procedure known as alar base reduction. This procedure may include removing sections of the base of the nostrils or sections of the nose where it meets the face. Risk of keloid scar formation is very low, if the patient has had not had keloids in the past. The tip of the nose can be restructured by removing tiny sections of cartilage to give the nose more definition, or adding cartilage grafts to provide additional structure to the nasal tip.
Revision rhinoplasty
Revision rhinoplasty is a nose operation carried out to correct or revise an unsatisfactory outcome from a previous rhinoplasty. It is also known as secondary rhinoplasty. Occasionally there can be a third rhinoplasty or in some instaces even more surgeries may be required. An unsatisfactory outcome occurs in 5 to 20% of rhinoplasties. There are two main reasons for performing secondary rhinoplasty. The first is purely cosmetic. A patient may be unsatisfied with all or part of a previous "nose reshaping”. A nasal fracture may not have been reduced enough, or too much. A prominent or bulbous nasal tip may have not been addressed appropriately, or over-aggressively. The nose may looked pinched, it may look like a parrot’s beak, or like a boxer’s nose. In all cases of surgery there is scarring and in some individuals the scarring can be unpredictable. There are many scenarios in which previous nose surgery may have left a nose aesthetically unappealing to a patient. The second reason for revision rhinoplasty is functional. The original nasal surgery may have been carried out to help with difficulties in breathing, and the outcome may have been unsatisfactory. Alternatively, the original surgery may have been performed for cosmetic reasons, but may have disrupted a normal physiologic mechanism involving the inspiration or expiration of air, making it difficult to breathe exposing a previously undiagnosed problem. Secondary rhinoplasty, and especially tertiary rhinoplasty, are extremely complicated procedures. This is self-evident because it is clear that even when the patient was operated upon for the first time, even when the tissues were “virginal,” and untouched the desired result were not obtained.
Reconstructive rhinoplasty
Reconstructive rhinoplasty refers to restoring the normal shape and function of the nose following damage from: traumatic accident, autoimmune disorder, intra-nasal drug abuse, previous injudicious cosmetic surgery, cancer involvement, or congenital abnormality. Rhinoplasty can restore skin coverage; recreate normal contours, and re-establish nasal airflow. Rhinoplasty for traumatic deformity: Traumatic accidents are the commonest cause of nasal deformity. Typically the nasal bones are broken and displaced. Occasionally, the nasal cartilages are disrupted or displaced, and in the worst cases the nasal dorsum is collapsed. Rhinoplasty allows shaving of the displaced bony humps, and re-alignment of the nasal bones after they are cut. When cartilage is disrupted, stitching of the cartilage for re-suspension, or use of cartilage grafts to camouflage depressions allows re-establishment of normal nasal contour. When the dorsum is collapsed, grafts of rib cartilage, ear cartilage, or cranial bone can be used to restore continuity to the dorsum. Although synthetic implants are also available for augmenting the nasal dorsum, cartilage or bone graft from the patient’s own body poses fewer risks of infection or rejection.
Rhinoplasty for collapsed nose due to septum perforation: Autoimmune problems such as Wegener’s Granulomatosis, Sarcoidosis, Churg-Strauss Syndrome, and Relapsing Polychondritis can lead to creation of a hole in the nasal septum, and loss of support in the dorsum leading to a saddle nose deformity. Intra nasal use of drugs such as cocaine, or extreme abuse of nasal decongestant sprays can similarly cause septum perforation and nasal dorsum collapse. Dorsum reconstruction is accomplished through the use of rib cartilage or bone grafts.
Rhinoplasty to correct nasal obstruction following injudicious cosmetic surgery: Reconstructive rhinoplasty after injudicious cosmetic surgery allows the restoration of normal breathing. When nasal cartilages are over-aggressively trimmed during rhinoplasty, the nose can appear pinched and nasal potency compromised. Patients complain of nasal blockage that is worsened by attempts at deep inspiration. Internal cartilage grafts to support the nasal tip (batton grafts) or widen the middle vault of the nose (spreader grafts) can be quite effective in restoring normal breathing. These grafting techniques will increase the size of the nasal tip and widen the dorsum.[1] Khosh et al.
Rhinoplasty for skin cancer excision: Excision of skin cancers from the nose can lead to loss of internal support as well as external skin coverage. Skin cancer excision in the nose is commonly accomplished via the Mohs’ technique. Once the cancer is removed, reconstructive rhinoplasty aims to provide skin coverage utilizing techniques such as skin graft, local skin flaps, or pedicle flaps. If cancer resection leads to loss of tissue in the area of the nasal tip, cartilage grafts are utilized to maintain support and prevent long-term distortion, by the force of scar contracture.
Rhinoplasty for Rhinophyma: Rhinophyma is the late stage manifestation of a skin condition known as Rosacea, where the skin is infected with acne roseacea. The skin in the area of the nasal tip becomes red, thickened, and enlarged as exemplified by W C Fields. Although known acne treatments such as antibiotics and Acutane can halt the progression of this disease, thickening of the skin and obscuring of the nasal tip landmarks can only be remedied by surgical correction. Currently, laser excision of thickened abnormal skin represents the best option in rhinoplasty for Rhinophyma. The CO2 laser and the Erbium YAG laser are the most effective types of laser for this disorder.[2]
Rhinoplasty for congenital nasal deformity: Vascular malformations and cleft lip anomalies are relatively common causes of congenital nasal deformities. In vascular malformations, the disease process can cause distortions of the skin and underlying structure of the nose. In cleft palate abnormalities, the size, position, and orientation of the nasal tip cartilages may be distorted. Rhinoplasty for reconstruction of vascular malformations can involve laser treatment of the skin and possible surgical excision. When the underlying cartilage structure is disturbed, cartilage grafts and stitching of the native nasal cartilages can help improve nasal appearance. In cleft lip patients, reconstructive rhinoplasty allows re-orientation of the nasal tip cartilages. Additional refinements with cartilage grafts to the tip are also frequently employed.[3]
Source*[4]
Side Effects of Rhinoplasty
Following your procedure, you will experience side effects commonly associated with rhinoplasty. These side effects are considered normal and are usually temporary.
Swelling: Expect swelling of your nose and the surrounding tissues to peak approximately thirty-six to forty-eight hours after surgery. You can expect more pronounced swelling if osteotomies (cuts or fractures to the nasal bones) were made during your procedure. Swelling is usually greatest when you rise in the morning. This side effect begins to subside within the first two weeks but will take at least a year to disappear completely.
Bruising: Bruising may occur between the eyes and on the cheeks, especially if you've had osteotomies performed. Bruising peaks approximately two days after surgery and then disappears, usually within two weeks.
Pain: The pain associated with rhinoplasty is usually mild. Most of the pain will probably disappear by the second or third day after surgery.
Nasal blockage: Congestion is to be expected following nasal surgery and may feel similar to the effects of a head cold. Cold-like symptoms are common for about six weeks after surgery.
Drainage: Following surgery, you can expect some nasal drainage to be tinged with blood, especially during the first day or two. You may notice an increase in nasal drainage when you rise to an upright position after being in a reclining position. This is normal and is not a cause for concern.
Stiffness in upper lip: Your upper lip may feel stiff, making it more difficult to smile. This feeling will usually dissipate within a few weeks.
Numbness of tip: The tip of your nose may feel numb, but the numbness usually disappears within a few months.
Depression: Don't be surprised if you discover that you feel a little blue in the days following your surgery. This is a common occurrence following surgery, when bruising and swelling are at their worst. This emotional letdown may be due to the fact that your face temporarily looks worse than it did prior to surgery, but it may also be attributable to stress, fatigue, or metabolic changes in your body. Rest assured that these feelings usually disappear within a few days.
Source*Paul S. Nassif, M.D., F.A.C.S.
In the Operating Room
This section gives a small introduction to the surgical techniques used during a rhinoplasty.
Much more detail about performing the rhinoplasty operation can be found at this online Rhinoplasty Tutorial.

The incisions for a rhinoplasty are hidden inside the nose which is refered to as the closed rhinoplasty technique. Some surgeons may combine the intranasal incisions with a small incision across the base of the nose depicted by the dotted line,this is refered to as the open rhinoplasty technique. Surgeon preference and/or patient anatomy may dictate the type of approach ,open versus closed,used in a apticular patient.

The incisions allow the surgeon to see the size and shape of the cartilages and bones on the inside of the nose, so that they can be altered.
Here, the scissors are pointing out the lower lateral cartilage (in blue), which is one of the cartilages that gives the tip of the nose its shape. The red line shows the location of the planned incision across the bottom of the nose.

Once the skin has been lifted from the bone and cartilage framework of the nose, often the first task is to remove a hump, if one is present. Part of the hump is made of bone, and part of the hump is cartilage.
In the photograph, the black line shows the desired profile. The nose is made of bone above the scalloped grey line and cartilage below that line. The part of the hump made of bone is shaded red, and the part of the hump made of cartilage is shaded blue.

The soft cartilage of the hump is removed with a scalpel, and the bony hump is often removed with a chisel, shown at the top of this photograph. "Osteotome" is the medical term for a chisel. This photograph also shows the copper hammer that is used with the osteotome.

After the main part of the hump is removed with an osteotome, files are used to smooth out the remaining bone. The files are also called rasps, and they come in different shapes, orientations, and grades.
Some surgeons use rasps to remove the entire hump, foregoing use of the osteotome.

A common complaint is that the tip of the nose is too wide. Many surgical techniques are available to narrow the tip of the nose, depending on what is causing the excess width.
In this photo, a suture is being placed to narrow the tip of the nose. The red line outlines the edge of the tip cartilage, which is narrowed when the suture tightens the fold of the cartilage at its apex. The suture is in light blue, ending in the needle, which appears white in the photograph. The cartilage is being held in place with tweezers, which are shaded green.

If the position of the nasal bones gives excess width to the upper part of the nose, the bones are moved inward, to a more narrow position. This skull shows in blue the position of the bones in the nose. For orientation, the eye sockets are outlined in red.
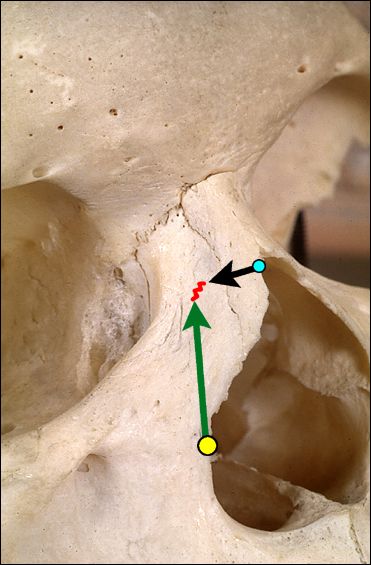
To narrow a nasal bone, two cuts are made in the bone with a tiny chisel: one cut starting at the yellow dot and extending up along the green arrow, and another cut starting at the blue dot and extending out along the black arrow. The piece of bone thus loosened from the skull is pushed inward, narrowing the nose.
These chisel cuts are made from underneath the skin, so there is no scar in the area after healing.

At the end of the procedure, after the incisions are closed, the nose is dressed, to hold it securely in place as it heals.
This photo shows the nose just before the dressing and splint are placed. The purple marks on the nose guided the surgeon in making accurate cuts in the bone during surgery.

Preparing for the metal splint: the nose is first covered with paper tape in a manner to help maintain the nose's new shape.

After taping, the metal splint is designed and cut and shaped, and it is placed on the nose.

The metal splint is then covered with the tape, to hold it in place. The operation is now completed. The dressing will be removed in one week.
Non-surgical rhinoplasty
Non-surgical rhinoplasty refers to a procedure in which fillers are used to alter and shape a person's nose without invasive surgery.[4] This procedure has been performed by doctors since 2003.[5] By filling in depressed areas, lifting the angle of the tip or smoothing the appearance of bumps on the bridge of the nose,[6] it can create a symmetrical nose that goes in harmony with the rest of a person's face, creating a better balance, and give the appearance of a smaller nose.
Although the procedure is usually performed for aesthetic purposes, it can also be used to correct some birth defects. Because the procedure is not invasive, the bruising and swelling are minimal. Duration of results depends on the type of filler used. Radiesse (calcium hydroxyapatite) lasts for 8 to 12 months and this is the filler that is ideal. Hyaluronic acid fillers usually last for 5-6 months. Artefill, a permanent filler was recently approved by the FDA.
See also
References
External links
- Rhinoplasty Surgical Procedure Anaesthetics, Surgical Procedure, Post-Op Care
- Rhinoplasty at the Encyclopedia of Surgery Demographics, description, diagnosis/preparation, aftercare, risks
- Rhinoplasty Surgery - Guide University of Maryland plastic surgery guides series
- Online Rhinoplasty Tutorial How the rhinoplasty is performed, with detailed descriptions and photographs taken during surgery
|
Cleft lip and palate Microchapters |
|
Diagnosis |
|---|
|
Treatment |
|
Case Studies |
|
Rhinoplasty On the Web |
|
American Roentgen Ray Society Images of Rhinoplasty |
Template:Operations and other procedures on the nose, mouth, and pharynx
ar:عملية تجميل الأنف cs:Rhinoplastika de:Rhinoplastik it:Rinoplastica he:ניתוח אף