Q fever pathophysiology: Difference between revisions
Ahmed Younes (talk | contribs) No edit summary |
m (Bot: Removing from Primary care) |
||
| (35 intermediate revisions by 6 users not shown) | |||
| Line 1: | Line 1: | ||
__NOTOC__ | __NOTOC__ | ||
{{CMG}} | |||
{{CMG}};{{AE}}{{AY}} | |||
{{Q fever}} | {{Q fever}} | ||
==Overview== | |||
Q fever is a disease caused by [[Coxiella burnetii|''C. burnetii'']], an [[intracellular]], [[gram-negative]] [[proteobacteria|proteobacterium]]. The disease can have a wide range of clinical presentations and affect many organ systems due to the unique [[virulence factors]] of the [[organism]]. | |||
== | ==Pathophysiology== | ||
===Transmission=== | |||
The organism is transmitted through:<ref name="pmid17423643">{{cite journal |vauthors=Marrie TJ |title=Q fever - a review |journal=Can. Vet. J. |volume=31 |issue=8 |pages=555–63 |year=1990 |pmid=17423643 |pmc=1480833 |doi= |url=}}</ref> | |||
*Aerosols: Inhalation of contaminated aerosols is the main mode of transmission | |||
*Ingestion of raw dairy products | |||
*[[vertical transmission|Vertical (mother to fetus) transmission]] has been reported | |||
*[[Parenteral]] | |||
*[[Tick bites]] | |||
===Pathogenesis=== | |||
The infection has two phases, which correlate to changes in the [[lipopolysaccharide]] of ''[[Coxiella burnetii|C.]] [[Coxiella burnetii|burnetii]]'':<ref name="pmid1489455">{{cite journal |vauthors=Choyce DP |title=Anterior chamber lens exchange |journal=J Cataract Refract Surg |volume=18 |issue=5 |pages=537 |year=1992 |pmid=1489455 |doi= |url=}}</ref> | |||
:*Phase I: Characterized by a smooth [[lipopolysaccharide]] capsule. Despite being less efficient in the invasion of host cells, [[antibodies]] against phase I are always isolated from acute Q fever patients. | |||
:*Phase II: Characterized by a rough [[lipopolysaccharide]] capsule. [[Antibodies]] against phase II have been isolated from chronic Q fever patients. | |||
[[Coxiella burnetii|''C. burnetii'']] can exist in two forms: the small cell form and the large cell form. The small and large cell forms are [[Antigen|antigenically different]], which plays a role in the [[virulence]] of the [[organism]]. | |||
====Small cell form<ref name="urlDiagnosis of Q Fever">{{cite web |url=http://jcm.asm.org/content/36/7/1823.short |title=Diagnosis of Q Fever |format= |work= |accessdate=}}</ref>==== | |||
The small cell form is often described as the spore form of [[Coxiella burnetii|''C. burnetii'']]. It can resist external environmental factors such as heat, pressure, and disinfectants for long periods of time. | |||
====Large cell form==== | |||
The large cell form is the active form of the [[organism]]. It persists in [[macrophages]] inside acidic [[vacuoles]]. | |||
== | *The [[genome]] of ''[[Coxiella burnetii|C.]] [[Coxiella burnetii|burnetii]]'' was analyzed in 1995. Multiple [[genes]] encoding for [[sodium|Na+ ion]] proton exchange have been discovered, explaining the ability of the organism to survive in a [[PH|low pH]] environment. | ||
* There is a delay between the entry of the [[organism]] into the host cell and the fusion with [[lysosomes]]. This delay is thought to be due to the transformation from the small cell variant into the large cell variant. | |||
* The [[acidic]] environment inside the [[lysosome]] has little effect on the large cell form of the organism. | |||
====Virulence factors==== | |||
*The [[lipopolysaccharide]] capsule is one of the most important [[virulence factors]] of the organism. | |||
*The different phases of infection are associated with changes in the [[lipopolysaccharide]] capsule. | |||
:*[[Lipopolysaccharide|Lipopolysaccharide phase I]] (smooth polysaccharide) is associated with protection against the host's [[immune response]]. | |||
:*[[Lipopolysaccharide|Lipopolysaccharide phase II]] (rough polysaccharide) is isolated from avirulent, non-infectious host cells and is not associated with protection of the virus from the host cell. | |||
*Both [[Humoral immunity|humoral]] and [[cell mediated immunity]] are involved in the immune response against ''[[Coxiella burnetii|C. burnetii]]''. However, [[cell mediated immunity]] is more important in defending against the organism and people with [[Immunosuppression|deficient cell mediated immunity]] are more susceptible to developing [[chronic]] [[infection]]. | |||
===Q fever as a biological weapon=== | |||
*Because of its route of infection, ''[[Coxiella burnetii|C. burnetii]]'' can be used as a [[biological warfare]] agent. | |||
*Q-fever is a category "B" agent. It is highly contagious and very stable in aerosols at a wide range of temperatures. | |||
*Just 1-2 particles are enough to infect an individual. | |||
*Q-fever [[microorganisms]] can survive on surfaces up to 60 days (like sporulating bacteria). | |||
*According to [[WHO]] estimates, 50 kg of [[Coxiella burnetii|''C. burnetii'']], if spread in an area of 2 square kilometers, is capable of:<ref name="urlapps.who.int">{{cite web |url=http://apps.who.int/iris/bitstream/10665/39444/1/24039.pdf |title=apps.who.int |format= |work= |accessdate=}}</ref> | |||
:*Infecting 500,000 humans | |||
:*Killing 150 individuals | |||
:*Causing acute illness in 125,000 individuals | |||
:*Causing chronic illness in 9,000 individuals | |||
{| | ==Microscopic pathology== | ||
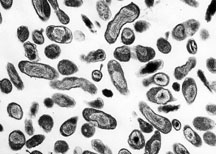
| [[Image:Coxiella burnetii. | |||
*''[[Coxiella burnetii|C.]] [[Coxiella burnetii|burnetii]]'' is a [[gram negative]], polymorphic, [[Intracellular|intracellular organism]].<ref name="urlQ Fever on JSTOR">{{cite web |url=http://www.jstor.org/stable/4458369?seq=1#page_scan_tab_contents |title=Q Fever on JSTOR |format= |work= |accessdate=}}</ref> | |||
*It was previously classified as a ''Rickettsia'', but now is considered a [[Proteobacteria|proteobacterium]]. | |||
{| class="wikitable" | |||
![[Image:Q_fever.jpg|center|300px|thumb|''Coxiella brutenii'']] | |||
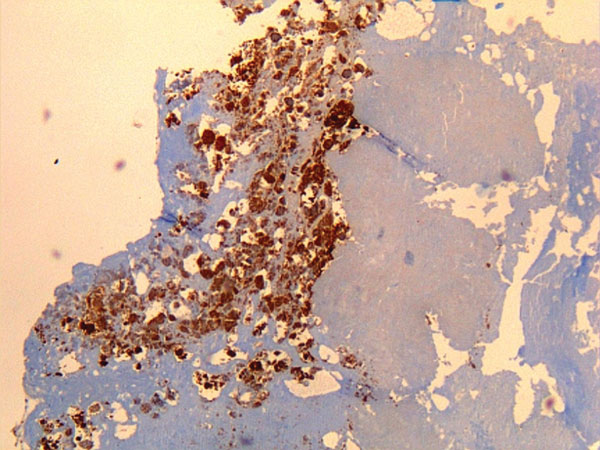
![[Image:Immunohistochemical detection of Coxiella burnetii in resected cardiac valve of a 60-year-old man with Q fever endocarditis - By Mahamat A, Edouard S, Demar M, Abboud P, Patrice J-Y, La Scola B, et al. -Public domain-, via Wikime.jpg|center|300px|thumb|Immunohistochemical detection of ''Coxiella burnetii'' in resected cardiac valve of a 60-year-old man with Q fever - By Mahamat A, Edouard S, Demar M, Abboud P, Patrice J-Y, La Scola B, et al. -Public domain-, via Wikime ]] | |||
|} | |} | ||
==References== | ==References== | ||
{{Reflist|2}} | {{Reflist|2}} | ||
[[Category: | [[Category:Emergency mdicine]] | ||
[[Category:Disease]] | |||
[[Category:Up-To-Date]] | |||
[[Category:Infectious disease]] | [[Category:Infectious disease]] | ||
[[Category: | [[Category:Gastroenterology]] | ||
[[Category:Hepatology]] | |||
[[Category:Pulmonology]] | |||
Latest revision as of 23:56, 29 July 2020
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1];Associate Editor(s)-in-Chief: Ahmed Younes M.B.B.CH [2]
|
Q fever Microchapters |
|
Diagnosis |
|---|
|
Treatment |
|
Case Studies |
|
Q fever pathophysiology On the Web |
|
American Roentgen Ray Society Images of Q fever pathophysiology |
|
Risk calculators and risk factors for Q fever pathophysiology |
Overview
Q fever is a disease caused by C. burnetii, an intracellular, gram-negative proteobacterium. The disease can have a wide range of clinical presentations and affect many organ systems due to the unique virulence factors of the organism.
Pathophysiology
Transmission
The organism is transmitted through:[1]
- Aerosols: Inhalation of contaminated aerosols is the main mode of transmission
- Ingestion of raw dairy products
- Vertical (mother to fetus) transmission has been reported
- Parenteral
- Tick bites
Pathogenesis
The infection has two phases, which correlate to changes in the lipopolysaccharide of C. burnetii:[2]
- Phase I: Characterized by a smooth lipopolysaccharide capsule. Despite being less efficient in the invasion of host cells, antibodies against phase I are always isolated from acute Q fever patients.
- Phase II: Characterized by a rough lipopolysaccharide capsule. Antibodies against phase II have been isolated from chronic Q fever patients.
C. burnetii can exist in two forms: the small cell form and the large cell form. The small and large cell forms are antigenically different, which plays a role in the virulence of the organism.
Small cell form[3]
The small cell form is often described as the spore form of C. burnetii. It can resist external environmental factors such as heat, pressure, and disinfectants for long periods of time.
Large cell form
The large cell form is the active form of the organism. It persists in macrophages inside acidic vacuoles.
- The genome of C. burnetii was analyzed in 1995. Multiple genes encoding for Na+ ion proton exchange have been discovered, explaining the ability of the organism to survive in a low pH environment.
- There is a delay between the entry of the organism into the host cell and the fusion with lysosomes. This delay is thought to be due to the transformation from the small cell variant into the large cell variant.
- The acidic environment inside the lysosome has little effect on the large cell form of the organism.
Virulence factors
- The lipopolysaccharide capsule is one of the most important virulence factors of the organism.
- The different phases of infection are associated with changes in the lipopolysaccharide capsule.
- Lipopolysaccharide phase I (smooth polysaccharide) is associated with protection against the host's immune response.
- Lipopolysaccharide phase II (rough polysaccharide) is isolated from avirulent, non-infectious host cells and is not associated with protection of the virus from the host cell.
- Both humoral and cell mediated immunity are involved in the immune response against C. burnetii. However, cell mediated immunity is more important in defending against the organism and people with deficient cell mediated immunity are more susceptible to developing chronic infection.
Q fever as a biological weapon
- Because of its route of infection, C. burnetii can be used as a biological warfare agent.
- Q-fever is a category "B" agent. It is highly contagious and very stable in aerosols at a wide range of temperatures.
- Just 1-2 particles are enough to infect an individual.
- Q-fever microorganisms can survive on surfaces up to 60 days (like sporulating bacteria).
- According to WHO estimates, 50 kg of C. burnetii, if spread in an area of 2 square kilometers, is capable of:[4]
- Infecting 500,000 humans
- Killing 150 individuals
- Causing acute illness in 125,000 individuals
- Causing chronic illness in 9,000 individuals
Microscopic pathology
- C. burnetii is a gram negative, polymorphic, intracellular organism.[5]
- It was previously classified as a Rickettsia, but now is considered a proteobacterium.
References
- ↑ Marrie TJ (1990). "Q fever - a review". Can. Vet. J. 31 (8): 555–63. PMC 1480833. PMID 17423643.
- ↑ Choyce DP (1992). "Anterior chamber lens exchange". J Cataract Refract Surg. 18 (5): 537. PMID 1489455.
- ↑ "Diagnosis of Q Fever".
- ↑ "apps.who.int" (PDF).
- ↑ "Q Fever on JSTOR".