Prostate cancer medical therapy: Difference between revisions
| Line 64: | Line 64: | ||
{{MedCondContrAbs | {{MedCondContrAbs | ||
|MedCond = Prostate cancer|Androderm|Methyltestosterone}} | |MedCond = Prostate cancer|Androderm|Methyltestosterone|Nandrolone}} | ||
==References== | ==References== | ||
Revision as of 20:03, 6 January 2015
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]
|
Prostate cancer Microchapters |
|
Diagnosis |
|---|
|
Treatment |
|
Case Studies |
|
Prostate cancer medical therapy On the Web |
|
American Roentgen Ray Society Images of Prostate cancer medical therapy |
|
Risk calculators and risk factors for Prostate cancer medical therapy |
Overview
Treatment for prostate cancer may involve watchful waiting, surgery, radiation therapy including brachytherapy (prostate brachytherapy) and external beam radiation, High Intensity Focused Ultrasound (HIFU), chemotherapy, cryosurgery, hormonal therapy, or some combination. Which option is best depends on the stage of the disease, the Gleason score, and the PSA level. Other important factors are the man's age, his general health, and his feelings about potential treatments and their possible side effects. Because all treatments can have significant side effects, such as erectile dysfunction and urinary incontinence, treatment discussions often focus on balancing the goals of therapy with the risks of lifestyle alterations.
Medical Therapy
Radiation therapy

Radiation therapy, also known as radiotherapy, is often used to treat all stages of prostate cancer, or when surgery fails. Radiotherapy uses ionizing radiation to kill prostate cancer cells. When absorbed in tissue, Ionizing radiation such as Gamma and x-rays damage the DNA in cells, which increases the probability of apoptosis (cell death). Two different kinds of radiation therapy are used in prostate cancer treatment: external beam radiation therapy and brachytherapy (specifically prostate brachytherapy).
External beam radiation therapy uses a linear accelerator to produce high-energy x-rays which are directed in a beam towards the prostate. A technique called Intensity Modulated Radiation Therapy (IMRT) may be used to adjust the radiation beam to conform with the shape of the tumor, allowing higher doses to be given to the prostate and seminal vesicles with less damage to the bladder and rectum. External beam radiation therapy is generally given over several weeks, with daily visits to a radiation therapy center. New types of radiation therapy may have fewer side effects than traditional treatment. One of these is Tomotherapy.

Permanent implant brachytherapy is a popular treatment choice for patients with low to intermediate risk features, can be performed on an outpatient basis, and is associated with good 10-year outcomes with relatively low morbidity[1] It involves the placement of about 100 small "seeds" containing radioactive material (such as iodine-125 or palladium-103) with a needle through the skin of the perineum directly into the tumor while under spinal or general anesthetic. These seeds emit lower-energy X-rays which are only able to travel a short distance. Although the seeds eventually become inert, they remain in the prostate permanently. The risk of exposure to others from men with implanted seeds is generally accepted to be insignificant.[2]
Radiation therapy is commonly used in prostate cancer treatment. It may be used instead of surgery or after surgery in early stage prostate cancer. In advanced stages of prostate cancer radiation is used to treat painful bone metastases. Radiation treatments also can be combined with hormonal therapy for intermediate risk disease, when radiation therapy alone is less likely to cure the cancer. Some radiation oncologists combine external beam radiation and brachytherapy for intermediate to high risk situations. One study found that the combination of six months of androgen suppressive therapy combined with external beam radiation had improved survival compared to radiation alone in patients with localized prostate cancer.[3] Others use a "triple modality" combination of external beam radiation therapy, brachytherapy, and hormonal therapy.
Radiation therapy uses high-energy rays or particles to kill cancer cells.[4] When delivered in the correct dosage, radiation can reduce the risk of recurrence.
Less common applications for radiotherapy are when cancer is compressing the spinal cord, or sometimes after surgery, such as when cancer is found in the seminal vesicles, in the lymph nodes, outside the prostate capsule, or at the margins of the biopsy.
Radiation therapy is often offered to men whose medical problems make surgery more risky. Radiation therapy appears to cure small tumors that are confined to the prostate just about as well as surgery. However, some issues remain unresolved, such as whether radiation should be given to the rest of the pelvis, how much the absorbed dose should be, and whether hormonal therapy should be given at the same time.
Side effects of radiation therapy might occur after a few weeks into treatment. Both types of radiation therapy may cause diarrhea and mild rectal bleeding due to radiation proctitis, as well as urinary incontinence and impotence. Symptoms tend to improve over time. Rates for impotence when comparing radiation to nerve-sparing surgery are similar. Radiation has lower rates of incontinence but higher rates of occasional mild rectal bleeding.[5] Men who have undergone external beam radiation therapy may have a slightly higher risk of later developing colon cancer and bladder cancer.[6]
Hormonal therapy
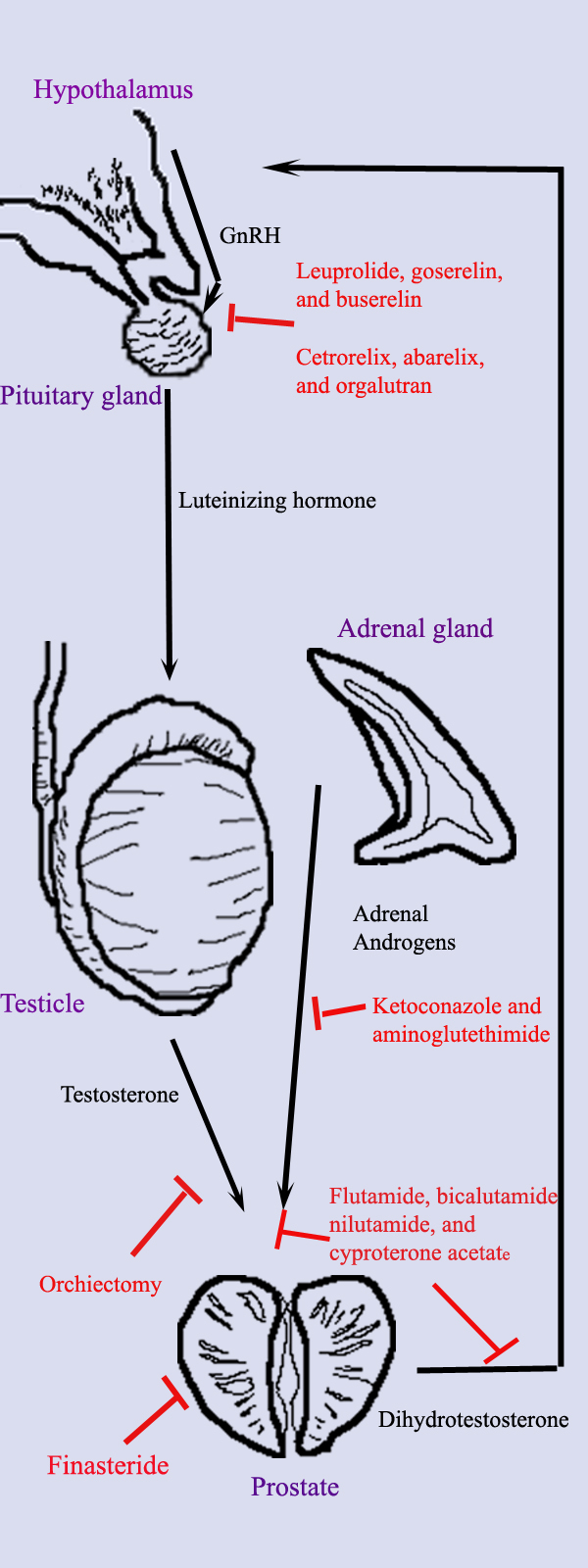
Hormonal therapy uses medications or surgery to block prostate cancer cells from getting dihydrotestosterone (DHT), a hormone produced in the prostate and required for the growth and spread of most prostate cancer cells. Blocking DHT often causes prostate cancer to stop growing and even shrink. However, hormonal therapy rarely cures prostate cancer because cancers which initially respond to hormonal therapy typically become resistant after one to two years. Hormonal therapy is therefore usually used when cancer has spread from the prostate. It may also be given to certain men undergoing radiation therapy or surgery to help prevent return of their cancer.[7]
Hormonal therapy for prostate cancer targets the pathways the body uses to produce DHT. A feedback loop involving the testicles, the hypothalamus, and the pituitary, adrenal, and prostate glands controls the blood levels of DHT. First, low blood levels of DHT stimulate the hypothalamus to produce gonadotropin releasing hormone (GnRH). GnRH then stimulates the pituitary gland to produce luteinizing hormone (LH), and LH stimulates the testicles to produce testosterone. Finally, testosterone from the testicles and dehydroepiandrosterone from the adrenal glands stimulate the prostate to produce more DHT. Hormonal therapy can decrease levels of DHT by interrupting this pathway at any point. There are several forms of hormonal therapy:
- Orchiectomy is surgery to remove the testicles. Because the testicles make most of the body's testosterone, after orchiectomy testosterone levels drop. Now the prostate not only lacks the testosterone stimulus to produce DHT, but also it does not have enough testosterone to transform into DHT.
- Antiandrogens are medications such as flutamide, bicalutamide, nilutamide, and cyproterone acetate which directly block the actions of testosterone and DHT within prostate cancer cells.
- Medications which block the production of adrenal androgens such as DHEA include ketoconazole and aminoglutethimide. Because the adrenal glands only make about 5% of the body's androgens, these medications are generally used only in combination with other methods that can block the 95% of androgens made by the testicles. These combined methods are called total androgen blockade (TAB). TAB can also be achieved using antiandrogens.
- GnRH action can be interrupted in one of two ways. GnRH antagonists suppress the production of LH directly, while GnRH agonists suppress LH through the process of downregulation after an initial stimulation effect. Abarelix is an example of a GnRH antagonist, while the GnRH agonists include leuprolide, goserelin, triptorelin, and buserelin. Initially, GnRH agonists increase the production of LH. However, because the constant supply of the medication does not match the body's natural production rhythm, production of both LH and GnRH decreases after a few weeks.[8]
- A very recent Trial I study (N=21) found that Abiraterone Acetate caused dramatic reduction in PSA levels and Tumor sizes in aggressive end-stage prostate cancer for 70% of patients. This is prostate cancer that resists all other treatments (e.g., castration, other hormones, etc.). Officially the impacts on life-span are not yet known because subjects have not been taking the drug very long. Larger Trial III Clinical Studies are in the works. If successful an approved treatment is hoped for around 2011.[9][10]
The most successful hormonal treatments are orchiectomy and GnRH agonists. Despite their higher cost, GnRH agonists are often chosen over orchiectomy for cosmetic and emotional reasons. Eventually, total androgen blockade may prove to be better than orchiectomy or GnRH agonists used alone.
Each treatment has disadvantages which limit its use in certain circumstances. Although orchiectomy is a low-risk surgery, the psychological impact of removing the testicles can be significant. The loss of testosterone also causes hot flashes, weight gain, loss of libido, enlargement of the breasts (gynecomastia), impotence and osteoporosis. GnRH agonists eventually cause the same side effects as orchiectomy but may cause worse symptoms at the beginning of treatment. When GnRH agonists are first used, testosterone surges can lead to increased bone pain from metastatic cancer, so antiandrogens or abarelix are often added to blunt these side effects. Estrogens are not commonly used because they increase the risk for cardiovascular disease and blood clots. The antiandrogens do not generally cause impotence and usually cause less loss of bone and muscle mass. Ketoconazole can cause liver damage with prolonged use, and aminoglutethimide can cause skin rashes.
Cardiovascular Effects of Androgen Suppression Therapy in Prostate Cancer
Androgen suppression therapy, which includes GnRH agonist, antiandrogens and bilateral orchiectomy, is used for the treatment of prostate cancer. Androgen suppression therapy use has been associated with increased incidence of cardiovascular risk factors. In fact, androgen suppression therapy contributes to an increase in obesity, modification of the body composition, a decrease in insulin sensitivity and dyslipidemia.[11] The science advisory from the American Heart Association, American Cancer Society, and American Urological Association recommends regular follow up for the evaluation of cardiovascular risk factors among patients with prostate cancer on androgen suppression therapy. Among patients with pre-existing cardiovascular disease, secondary prevention should be optimized.[11]
In addition, androgen suppression therapy use is associated with increased risk of myocardial infarction (MI), stroke[12] and shorter time to MI.[13] A cohort of 73,196 patients with prostate cancer, among which one third received GnRH agonist revealed an association between GnRH agonist use and increased incidence of diabetes (HR=1.44; P < 0.001), coronary heart disease (HR=1.16; P < 0.001) and MI (HR=1.11; P = 0.03).[14]
The association between androgen suppression therapy use and increased cardiovascular mortality is controversial. While this association has been reported in some studies,[15][16] others suggest that this association is only valid when the subject has co-existing comorbidities or other cardiac risk factors.[17] A metanalysis of 8 randomized clinical trials of 4141 patients demonstrates that androgen suppression therapy use in prostate cancer is not significantly associated with increased cardiovascular mortality (RR=0.93; 95% CI, 0.79-1.10; P = 0.41).[18] However, a metanalysis of 11 randomized clinical trials of 4805 patients reports that androgen suppression therapy use is associated with decreased prostate cancer related mortality (RR=0.69; 95% CI, 0.56-0.84; P < 0.001) and decreased overall mortality (RR=0.86; 95% CI, 0.80-0.93; P <0.001).[18]
Palliative care
Palliative care for advanced stage prostate cancer focuses on extending life and relieving the symptoms of metastatic disease. As noted above Abiraterone Acetate is showing some promise in treating advance stage prostate cancer. It causes a dramatic reduction in PSA levels and Tumor sizes in aggressive advanced-stage prostate cancer for 70% of patients. Chemotherapy may be offered to slow disease progression and postpone symptoms. The most commonly used regimen combines the chemotherapeutic drug docetaxel with a corticosteroid such as prednisone.[19] Bisphosphonates such as zoledronic acid have been shown to delay skeletal complications such as fractures or the need for radiation therapy in patients with hormone-refractory metastatic prostate cancer.[20]
Bone pain due to metastatic disease is treated with opioid pain relievers such as morphine and oxycodone. External beam radiation therapy directed at bone metastases may provide pain relief. Injections of certain radioisotopes, such as strontium-89, phosphorus-32, or samarium-153, also target bone metastases and may help relieve pain.
Androgen ablation therapy
In 1941, Charles Huggins reported that androgen ablation therapy causes regression of primary and metastatic androgen-dependent prostate cancer.[21] Androgen ablation therapy causes remission in 80-90% of patients undergoing therapy, resulting in a median progression-free survival of 12 to 33 months. After remission an androgen-independent phenotype typically emerges, where the median overall survival is 23–37 months from the time of initiation of androgen ablation therapy.[22] The actual mechanism contributes to the progression of prostate cancer is not clear and may vary between individual patient. A few possible mechanisms have been proposed.[23] Scientists have established a few prostate cancer cell lines to investigate the mechanism involved in the progression of prostate cancer. LNCaP, PC-3, and DU-145 are commonly used prostate cancer cell lines. The LNCaP cancer cell line was established from a human lymph node metastatic lesion of prostatic adenocarcinoma. PC-3 and DU-145 cells were established from human prostatic adenocarcinoma metastatic to bone and to brain, respectively. LNCaP cells express androgen receptor (AR), however, PC-3 and DU-145 cells express very little or no AR. AR, an androgen-activated transcription factor, belongs to the steroid nuclear receptor family. Development of the prostate is dependent on androgen signaling mediated through AR, and AR is also important during the development of prostate cancer. The proliferation of LNCaP cells is androgen-dependent but the proliferation of PC-3 and DU-145 cells is androgen-insensitive.Elevation of AR expression is often observed in advanced prostate tumors in patients.[24][25] Some androgen-independent LNCaP sublines have been developed from the ATCC androgen-dependent LNCaP cells after androgen deprivation for study of prostate cancer progression. These androgen-independent LNCaP cells have elevated AR expression and express prostate specific antigen upon androgen treatment. Androgens paradoxically inhibit the proliferation of these androgen-independent prostate cancer cells.[26][27][28] Androgen at a concentration of 10-fold higher than the physiological concentration has also been shown to cause growth suppression and reversion of androgen-independent prostate cancer xenografts or androgen-independent prostate tumors derived in vivo model to an androgen-stimulated phenotype in athymic mice.[29][30] These observation suggest the possibility to use androgen to treat the development of relapsed androgen-independent prostate tumors in patients. Oral infusion of green tea polyphenols, a potential alternative therapy for prostate cancer by natural compounds, has been shown to inhibit the development, progression, and metastasis as well in autochthonous transgenic adenocarcinoma of the mouse prostate (TRAMP) model, which spontaneously develops prostate cancer.[31]
Contraindicated medications
Prostate cancer is considered an absolute contraindication to the use of the following medications:
References
- ↑ Nag, S (1999). "American Brachytherapy Society Recommendations for Transperineal Permanent Brachytherapy of Prostate Cancer". Int. J. Rad. Onc. Biol. Phys. 44 (4): 789–799. ?. Unknown parameter
|month=ignored (help); Unknown parameter|coauthors=ignored (help) Review. - ↑ Perez, CA (1993). "Localized carcinoma of the prostate (stages T1B, T1C, T2, and T3). Review of management with external beam radiation therapy". Cancer. 72 (11): 3156–73. doi:10.1002/1097-0142(19931201)72:11<3156::AID-CNCR2820721106>3.0.CO;2-G. PMID 7694785. Unknown parameter
|month=ignored (help); Unknown parameter|coauthors=ignored (help) Review. - ↑ D'Amico AV, Manola J, Loffredo M, Renshaw AA, DellaCroce A, Kantoff PW (2004). "6-month androgen suppression plus radiation therapy vs radiation therapy alone for patients with clinically localized prostate cancer: a randomized controlled trial". JAMA. 292 (7): 821–7. doi:10.1001/jama.292.7.821. PMID 15315996.
- ↑ American Cancer Society: Radiation Treatment
- ↑ Lawton, CA (1991). "Long-term treatment sequelae following external beam irradiation for adenocarcinoma of the prostate: analysis of RTOG studies 7506 and 7706". Int J Radiat Oncol Biol Phys. 21 (4): 935–9. PMID 1917622. Unknown parameter
|month=ignored (help); Unknown parameter|coauthors=ignored (help) - ↑ Brenner, DJ (2000). "Second malignancies in prostate carcinoma patients after radiotherapy compared with surgery". Cancer. 88 (2): 398–406. doi:10.1002/(SICI)1097-0142(20000115)88:2<398::AID-CNCR22>3.0.CO;2-V. PMID 10640974. Unknown parameter
|month=ignored (help); Unknown parameter|coauthors=ignored (help) - ↑ Robson, M (1996). "How is androgen-dependent metastatic prostate cancer best treated?". Hematol Oncol Clin North Am. 10 (3): 727–47. doi:10.1016/S0889-8588(05)70364-6. PMID 8773508. Unknown parameter
|month=ignored (help); Unknown parameter|coauthors=ignored (help) Review. - ↑ Loblaw, DA (2004). "American Society of Clinical Oncology recommendations for the initial hormonal management of androgen-sensitive metastatic, recurrent, or progressive prostate cancer". J Clin Oncol. 22 (14): 2927–41. doi:10.1200/JCO.2004.04.579. PMID 15184404. Unknown parameter
|month=ignored (help); Unknown parameter|coauthors=ignored (help) Erratum in: J Clin Oncol. 2004 November 1;22(21):4435. - ↑ de Bono, Johann (2004). "Phase I Clinical Trial of a Selective Inhibitor of CYP17, Abiraterone Acetate, Confirms That Castration-Resistant Prostate Cancer Commonly Remains Hormone Driven". J Clin Oncol: online. doi:10.1200/JCO.2007.15.9749. PMID 15184404. Unknown parameter
|month=ignored (help); Unknown parameter|coauthors=ignored (help) Erratum in: J Clin Oncol. Early Release, published ahead of print July 21, 2008 - ↑ Richard Warry (July 22, 2008). "Drug for deadly prostate cancer". BBC. Retrieved 2008-07-23.
- ↑ 11.0 11.1 Levine GN, D'Amico AV, Berger P, Clark PE, Eckel RH, Keating NL; et al. (2010). "Androgen-deprivation therapy in prostate cancer and cardiovascular risk: a science advisory from the American Heart Association, American Cancer Society, and American Urological Association: endorsed by the American Society for Radiation Oncology". Circulation. 121 (6): 833–40. doi:10.1161/CIRCULATIONAHA.109.192695. PMC 3023973. PMID 20124128.
- ↑ Jespersen CG, Nørgaard M, Borre M (2014). "Androgen-deprivation Therapy in Treatment of Prostate Cancer and Risk of Myocardial Infarction and Stroke: A Nationwide Danish Population-based Cohort Study". Eur Urol. 65 (4): 704–9. doi:10.1016/j.eururo.2013.02.002. PMID 23433805.
- ↑ D'Amico AV, Denham JW, Crook J, Chen MH, Goldhaber SZ, Lamb DS; et al. (2007). "Influence of androgen suppression therapy for prostate cancer on the frequency and timing of fatal myocardial infarctions". J Clin Oncol. 25 (17): 2420–5. doi:10.1200/JCO.2006.09.3369. PMID 17557956.
- ↑ Keating NL, O'Malley AJ, Smith MR (2006). "Diabetes and cardiovascular disease during androgen deprivation therapy for prostate cancer". J Clin Oncol. 24 (27): 4448–56. doi:10.1200/JCO.2006.06.2497. PMID 16983113.
- ↑ Tsai HK, D'Amico AV, Sadetsky N, Chen MH, Carroll PR (2007). "Androgen deprivation therapy for localized prostate cancer and the risk of cardiovascular mortality". J Natl Cancer Inst. 99 (20): 1516–24. doi:10.1093/jnci/djm168. PMID 17925537.
- ↑ Van Hemelrijck M, Garmo H, Holmberg L, Ingelsson E, Bratt O, Bill-Axelson A; et al. (2010). "Absolute and relative risk of cardiovascular disease in men with prostate cancer: results from the Population-Based PCBaSe Sweden". J Clin Oncol. 28 (21): 3448–56. doi:10.1200/JCO.2010.29.1567. PMID 20567006.
- ↑ Nanda A, Chen MH, Braccioforte MH, Moran BJ, D'Amico AV (2009). "Hormonal therapy use for prostate cancer and mortality in men with coronary artery disease-induced congestive heart failure or myocardial infarction". JAMA. 302 (8): 866–73. doi:10.1001/jama.2009.1137. PMID 19706860.
- ↑ 18.0 18.1 Nguyen PL, Je Y, Schutz FA, Hoffman KE, Hu JC, Parekh A; et al. (2011). "Association of androgen deprivation therapy with cardiovascular death in patients with prostate cancer: a meta-analysis of randomized trials". JAMA. 306 (21): 2359–66. doi:10.1001/jama.2011.1745. PMID 22147380. Review in: Ann Intern Med. 2012 Apr 17;156(8):JC4-04, JC4-05
- ↑ Tannock, IF (2004). "Docetaxel plus prednisone or mitoxantrone plus prednisone for advanced prostate cancer". N Engl J Med. 351 (15): 1502–12. doi:10.1056/NEJMoa040720. PMID 1547021. Unknown parameter
|month=ignored (help); Unknown parameter|coauthors=ignored (help) - ↑ Saad F, Gleason DM, Murray R, Tchekmedyian S, Venner P, Lacombe L, Chin JL, Vinholes JJ, Goas JA, Chen B (2002). "A randomized, placebo-controlled trial of zoledronic acid in patients with hormone-refractory metastatic prostate carcinoma". J Natl Cancer Inst. 94 (19): 1458–68. PMID 12359855.
- ↑ Huggins C, Steven RE and Hodges CV, Studies on prostatic cancer. Arch. Sug. 43:209–223, 1941.
- ↑ Hellerstedt BA and Pienta KJ, The current state of hormonal therapy for prostate cancer, CA Cancer J. Clin. 52: 154–179, 2002.PMID 12018929
- ↑ Feldman BJ, Feldman D. The development of androgen-independent prostate cancer. Nat Rev Cancer. 2001 Oct;1(1):34–45. PMID 11900250
- ↑ Linja MJ, Savinainen KJ, Saramaki OR, Tammela TL, Vessella RL, Visakorpi T. Amplification and overexpression of androgen receptor gene in hormone-refractory prostate cancer. Cancer Res. 2001 May 1;61(9):3550–5. PMID 11325816
- ↑ Ford OH 3rd, Gregory CW, Kim D, Smitherman AB, Mohler JL. Androgen receptor gene amplification and protein expression in recurrent prostate cancer. J Urol. 2003 Nov;170(5):1817–21.PMID 14532783
- ↑ Kokontis J, Takakura K, Hay N, Liao S. Increased androgen receptor activity and altered c-myc expression in prostate cancer cells after long-term androgen deprivation. Cancer Res. 1994 March 15;54(6):1566–73. PMID 7511045
- ↑ Umekita Y, Hiipakka RA, Kokontis JM, Liao S. Human prostate tumor growth in athymic mice: inhibition by androgens and stimulation by finasteride. Proc Natl Acad Sci U S A. 1996 October 15;93(21):11802-7. PMID 8876218
- ↑ Kokontis JM, Hsu S, Chuu CP, Dang M, Fukuchi J, Hiipakka RA, Liao S. Role of androgen receptor in the progression of human prostate tumor cells to androgen independence and insensitivity. Prostate. 2005 December 1;65(4):287-98. PMID 16015608
- ↑ Chuu CP, Hiipakka RA, Fukuchi J, Kokontis JM, Liao S. Androgen causes growth suppression and reversion of androgen-independent prostate cancer xenografts to an androgen-stimulated phenotype in athymic mice. Cancer Res. 2005 March 15;65(6):2082–4. PMID 15781616
- ↑ Chuu CP, Hiipakka RA, Kokontis JM, Fukuchi J, Chen RY, Liao S. Inhibition of tumor growth and progression of LNCaP prostate cancer cells in athymic mice by androgen and liver X receptor agonist. Cancer Res. 2006 July 1;66(13):6482–6. PMID 16818617
- ↑ Gupta S, Hastak K, Ahmad N, Lewin JS, Mukhtar H. Inhibition of prostate carcinogenesis in TRAMP mice by oral infusion of green tea polyphenols. Proc Natl Acad Sci U S A. 2001 August 28;98(18):10350-5. PMID 11504910